Family caregivers may develop PTSD from witnessing traumatic events, experiencing chronic stress, prolonged exposure to trauma, high-stress responsibilities, and the emotional strain of caregiving. The combination of these factors can trigger the onset of PTSD. It is important to recognize the impact and seek support to prevent caregiver burnout and mental health conditions like PTSD. Untreated trauma, lack of support, sudden changes in roles, and ongoing stress without reprieves can also contribute to this. Understanding these causes is essential for the well-being and mental health of caregivers. More information is accessible here.
Key Takeaways
- Witnessing traumatic events and chronic stress contribute to PTSD risk.
- Caregiver burnout from high-stress responsibilities can lead to PTSD.
- Unresolved trauma can be triggered by caregiving, worsening PTSD symptoms.
- Lack of support and breaks increases the likelihood of developing PTSD.
- Sudden role changes in caregiving can impact emotional well-being and lead to PTSD.
Causes of PTSD in Family Caregivers
Witnessing traumatic events or dealing with chronic stress can lead family caregivers to develop PTSD. Family caregivers face a higher risk of developing this mental health disorder due to factors such as prolonged trauma exposure, depression, anxiety, negative temperament, and high-stress responsibilities. Caregivers who are exposed to sudden deaths, violent outbursts, or overwhelming responsibilities may be particularly vulnerable to developing PTSD.
Recognizing that PTSD symptoms can manifest differently among caregivers, triggered by various events and situations they encounter in their caregiving role, is vital. To prevent and manage PTSD, seeking professional help and emotional support is crucial for family caregivers. By understanding the causes and risks associated with PTSD in family caregivers, we can better support and care for those who dedicate themselves to looking after their loved ones.
Impact of Caregiving Stress
Caregiver burnout can have significant effects on our mental health, leading to conditions like PTSD.
The stress and emotional strain from caregiving responsibilities increase the risk of developing PTSD.
It's important to recognize these impacts and seek support to prevent long-term mental health risks.
Caregiver Burnout Effects
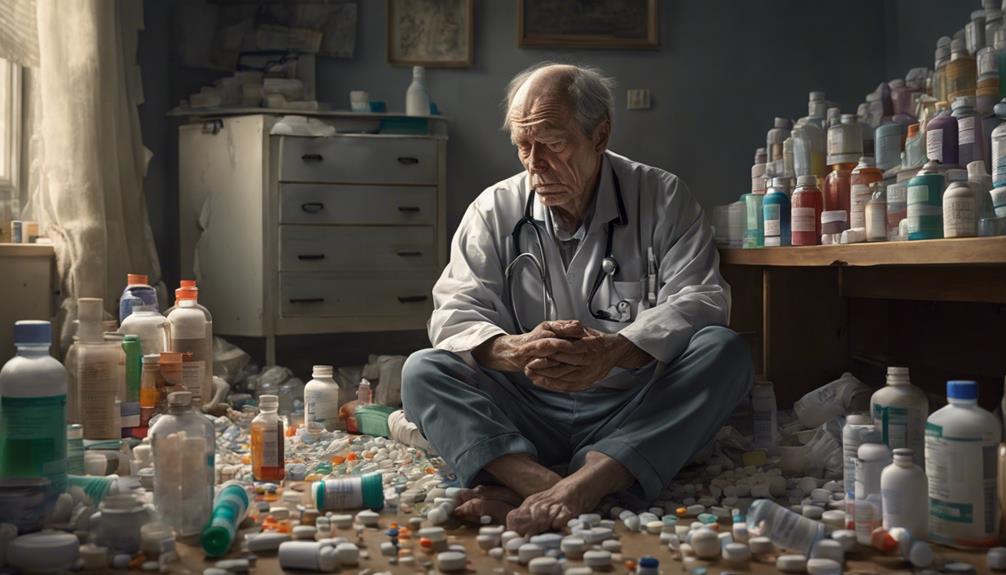
Experiencing the effects of caregiver burnout can greatly impact both our mental and physical well-being. Caregivers are at risk of developing PTSD symptoms due to the emotional and physical toll of their responsibilities. Chronic stress from caregiving can lead to feelings of overwhelm and despair, increasing the likelihood of developing PTSD.
Balancing caregiving duties with self-care is essential to prevent burnout and mitigate the risk of experiencing symptoms similar to PTSD. It's important to acknowledge the impact that traumatic events can have on our mental and physical health as caregivers. Practicing self-care strategies and seeking support are essential in managing caregiver burnout and maintaining overall well-being.
Mental Health Risks
The toll of chronic stress and emotional strain from caregiving responsibilities can have a profound impact on the mental health of family caregivers, potentially leading to PTSD development. Caregivers of ICU patients are particularly at risk due to the intense and often traumatic nature of the caregiving environment. Being a full-time caregiver can expose individuals to a traumatic event, increasing the likelihood of developing PTSD. Symptoms of PTSD, such as intrusive memories and avoidance behaviors, are commonly associated with the psychological impact of caregiving stress. Compassion fatigue, a result of prolonged exposure to stress and suffering, can exacerbate the risk of PTSD among family caregivers. Understanding these risk factors and symptoms is essential for caregivers to prioritize their mental well-being while providing care to their loved ones.
| Risk Factors for PTSD | Symptoms of PTSD | Associated with PTSD |
|---|---|---|
| Traumatic events | Intrusive memories | Psychological impact |
| Full-time caregiver | Avoidance behaviors | Compassion fatigue |
| Caregivers of ICU patients | Heightened arousal |
Role of Unresolved Trauma
When unaddressed trauma lingers unresolved, the risk of developing PTSD among family caregivers can significantly increase. Caregiving can bring about substantial stress and emotional challenges, potentially triggering past traumatic experiences. Anxiety and depression left unmanaged can compound the effects of lingering trauma, making caregivers more vulnerable to developing PTSD. Additionally, factors like socioeconomic status and lack of community support can further strain caregivers, exacerbating their unresolved trauma and increasing the likelihood of PTSD symptoms.
Family caregivers facing unresolved trauma may find it particularly challenging to navigate their caregiving responsibilities. Without proper support systems or coping mechanisms, the weight of past traumatic events can become overwhelming, leading to the development of PTSD. It's important for caregivers to recognize the impact of unresolved trauma on their mental health and seek help when needed. By addressing unresolved trauma through therapy, support groups, or other interventions, caregivers can better protect their well-being and provide effective care to their loved ones.
Lack of Caregiver Support

Insufficient emotional support and understanding from family and friends can greatly contribute to caregivers developing PTSD. When caregivers feel isolated and overwhelmed without adequate support, the risk of PTSD increases. Here are some key factors related to the lack of caregiver support:
- *Chronic Stress:* Continuously caring for a loved one without breaks can lead to chronic stress, impacting the caregiver's mental health.
- *Emotional Support:* Caregivers need understanding and empathy from their loved ones to help them cope with the challenges they face daily.
- *Respite Care:* The absence of breaks for caregivers can result in burnout and increase the likelihood of developing PTSD.
- *Support Groups:* Access to support groups provides caregivers with a sense of community and understanding, aiding in managing stress and trauma.
- *Counseling Services:* Limited access to counseling services can hinder caregivers from getting professional help to navigate their emotions and experiences effectively.
Sudden Role Changes
Experiencing sudden changes in caregiving responsibilities can greatly disrupt our daily routines and sense of self. Caregivers may find themselves unexpectedly thrown into new roles and tasks, causing a significant impact on their identity and emotional well-being. The unforeseen adjustments can lead to adaptability struggles, as they try to navigate unfamiliar responsibilities while managing their existing duties. These rapid shifts often trigger emotional distress, feelings of inadequacy, and uncertainty about their capabilities.
As caregivers grapple with these abrupt role changes, they may also face an increased risk of caregiver burnout. The added stress and overwhelm from juggling new responsibilities alongside their existing caregiving duties can push them to their limits. Additionally, these changes can contribute to the development of PTSD symptoms, as the constant pressure and emotional toll take a toll on their mental health. It's vital for caregivers to seek support and practice self-care during these challenging times to mitigate the negative effects of sudden role changes.
Research Gaps in PTSD Caregiving Impact

Research gaps in understanding the impact of caregiving on PTSD among family caregivers hinder the development of effective interventions and support systems. When it comes to PTSD among family caregivers, there are several areas where more research is needed:
- Limited studies focus on the specific triggers and risk factors for PTSD development among family caregivers.
- Understanding how caregiving responsibilities contribute to PTSD development requires further investigation.
- Research on the link between caregiving and PTSD is limited, creating gaps in understanding the impact on family caregivers.
- There's a need for more research funding to explore the prevalence and consequences of PTSD in family caregivers.
- Identifying effective interventions and support systems for family caregivers experiencing PTSD remains an area needing more research.
Frequently Asked Questions
What Is the Trauma After Being a Caregiver?
Being a caregiver can result in trauma due to witnessing or experiencing distressing events. The emotional toll of caregiving can lead to conditions like PTSD. Caregivers may struggle with flashbacks, nightmares, and heightened stress responses.
What Are the Triggers for PTSD at Work?
Facing sudden deaths or traumatic events can trigger PTSD in family caregivers. High-stress responsibilities and daily challenges contribute to PTSD development. Angry outbursts from patients can provoke fight or flight responses. Long-lasting trauma, depression, or anxiety increase risk.
What Are the 17 Symptoms of Complex Ptsd?
We experience 17 symptoms in complex PTSD, such as emotional dysregulation, negative self-concept, and trust issues. These challenges impact daily life and relationships immensely. Recognizing and addressing these symptoms is vital for our well-being and growth.
What Are the Possible Causes of Stress on a Family Care Provider?
Taking care of a loved one can cause stress for family caregivers due to high-pressure responsibilities, overwhelming emotions, and financial strains. Balancing these aspects can be challenging and lead to mental health consequences.
How Can Developing PTSD in Family Caregivers be Managed with Relief Strategies?
When family caregivers experience PTSD, caregiver relief strategies essential to manage their emotional distress. Seeking professional counseling, finding support groups, and practicing self-care are integral. Taking regular breaks, delegating tasks, and setting boundaries can help prevent burnout and improve mental well-being for caregivers.
Conclusion
To summarize, family caregivers can develop PTSD due to the stress, unresolved trauma, lack of support, and sudden role changes they experience.
It's important for caregivers to recognize the signs of PTSD and seek help from mental health professionals.
By addressing these challenges and taking care of their own mental well-being, caregivers can better support their loved ones and themselves.
Remember, it's okay to ask for help and prioritize self-care in the caregiving journey.