Genetic factors such as APOE and family history, combined with age and environmental triggers like toxins, play a part in the development of Lewy body dementia. The accumulation of alpha-synuclein protein interferes with brain function. Disruptions in neurotransmitters such as dopamine and acetylcholine influence symptoms. Brain irregularities and oxidative stress also contribute. Inflammation and mitochondrial dysfunction affect the progression of the disease. Vascular problems impacting blood flow are crucial. Recognizing these factors aids in the creation of therapies. Delving into the complex causes of Lewy body dementia can offer insights into effectively managing and possibly treating this condition.
Key Takeaways
- Genetic factors like APOE variants and family history increase risk.
- Accumulation of alpha-synuclein protein leads to neuronal dysfunction.
- Environmental triggers like toxins and pesticides may contribute to development.
- Brain abnormalities such as Lewy bodies disrupt normal brain function.
- Imbalance in neurotransmitters like dopamine and acetylcholine plays a role in symptoms.
Genetic Factors
Genetic factors play a significant role in the development of Lewy body dementia. Variants in genes like APOE, SNCA, and GBA increase the risk of this condition. Having a family history of Lewy body dementia or Parkinson's disease can also elevate the likelihood of developing this disorder. While genetic factors contribute, other elements like age, Parkinson's disease, and REM sleep behavior disorder are risk factors for Lewy body dementia as well.
Understanding these genetic components is vital in identifying individuals at higher risk and potentially creating targeted interventions.
Individuals with specific genetic variations need to be vigilant about monitoring their health for any early signs of Lewy body dementia. If there's a family history of this condition or Parkinson's disease, discussing these risk factors with healthcare providers is crucial. Regular check-ups and open communication about genetic predispositions can aid in early detection and management of Lewy body dementia.
Alpha-Synuclein Protein
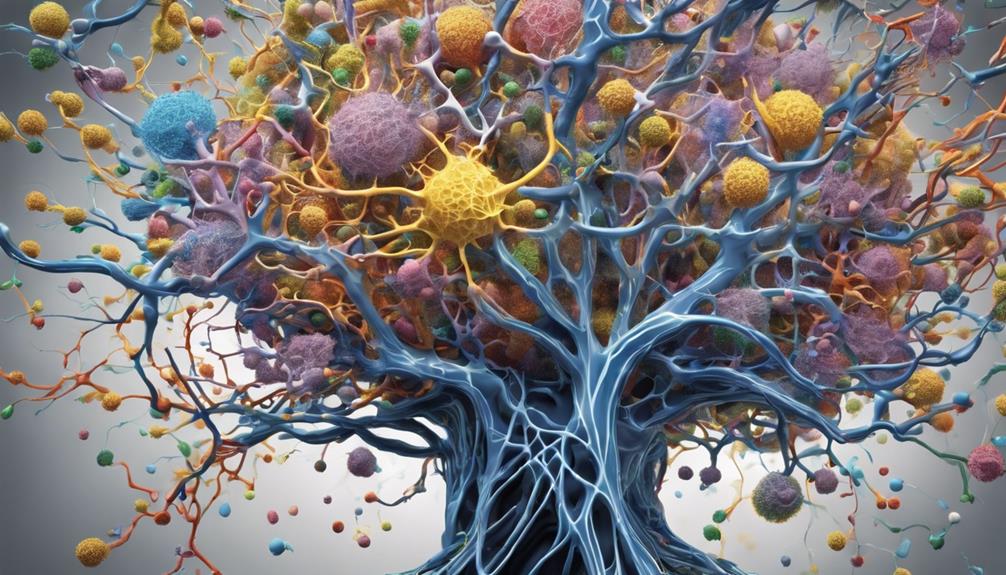
The role of the alpha-synuclein protein in Lewy body dementia is pivotal, as it is a key component of Lewy bodies found in affected individuals. Alpha-synuclein accumulation in nerve cells leads to the formation of Lewy bodies in the brain, which is associated with neuronal dysfunction and cell death. This aggregation of alpha-synuclein is central to the pathology of Lewy body dementia, making it an essential focus of research for developing targeted treatments.
To understand the impact of alpha-synuclein on Lewy body dementia, researchers study how this protein affects brain cells. By investigating the mechanisms behind alpha-synuclein accumulation and its consequences, scientists aim to find ways to prevent or reverse the damage caused to nerve cells. This research is vital for developing therapies that can specifically target alpha-synuclein pathology and potentially slow down the progression of Lewy body dementia.
| Lewy bodies | Alpha-Synuclein Protein | Neuronal Dysfunction | Cell Death |
|---|---|---|---|
| Abnormal protein aggregates in nerve cells | Key component of Lewy bodies | Associated with dysfunction in nerve cells | Contributes to cell death in the brain |
Environmental Triggers
Exposure to external toxins and genetic predisposition are key factors to take into account when discussing environmental triggers for Lewy body dementia.
Toxins, pesticides, and certain chemicals in our surroundings can potentially contribute to the development of this disease.
Understanding the interaction between these external factors and genetic susceptibility is essential in unraveling the complexities of Lewy body dementia.
External Toxin Exposure
Occupational exposure to environmental toxins has been implicated in contributing to the development of Lewy body dementia. Exposure to pesticides, heavy metals, and solvents may play a role in the onset of this condition.
Living in areas with high levels of environmental toxins could also be an important risk factor for Lewy body dementia. These toxins have the ability to disrupt normal brain functions and neuronal pathways, leading to the accumulation of abnormal proteins that are characteristic of Lewy body dementia.
While there's research suggesting a link between external toxin exposure and the formation of Lewy bodies in the brain, further studies are necessary to establish a definitive causal relationship. It's essential to be aware of the potential impact of environmental toxins on brain health.
Genetic Predisposition
Considering the intricate relationship between genetic predisposition and environmental triggers, the development of Lewy body dementia involves a complex interplay of factors. When exploring the genetic aspect, variants in genes such as APOE, SNCA, and GBA have been linked to a higher susceptibility to Lewy body dementia.
Additionally, a family history of Parkinson's disease or Lewy body dementia can amplify an individual's genetic predisposition to this condition. Understanding how these genetic factors interact with environmental triggers is pivotal in unraveling the causes of Lewy body dementia.
Through this interplay, researchers aim to shed light on how certain genetic variations may elevate the risk of developing this neurological disorder.
Brain Abnormalities
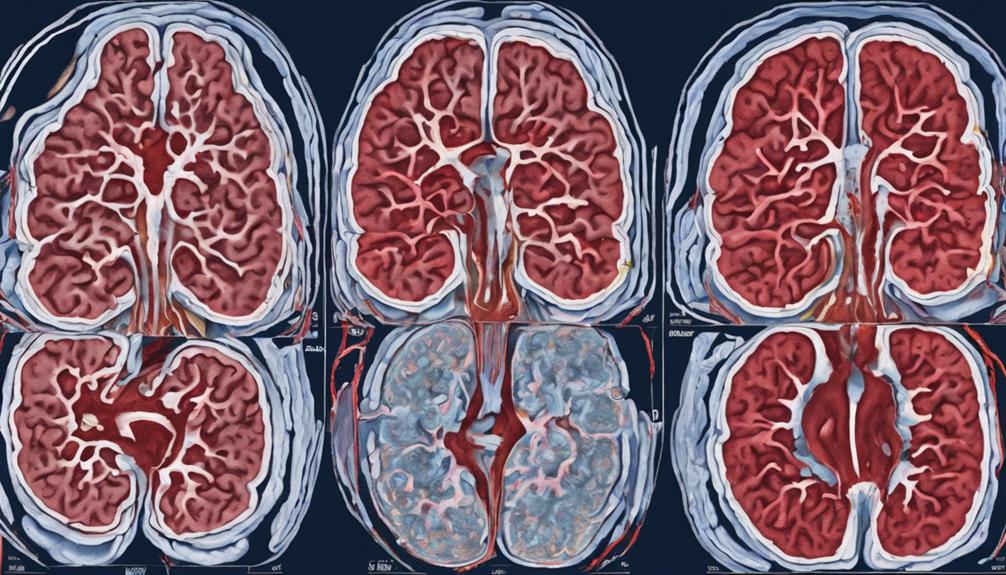
What brain abnormalities are associated with Lewy body dementia?
Lewy body dementia is linked to the presence of abnormal protein deposits known as Lewy bodies in the brain. These Lewy bodies are primarily composed of alpha-synuclein protein, which disrupts normal brain function and contributes to cognitive decline. The accumulation of Lewy bodies in nerve cells hinders neurotransmitter regulation, impacting the communication between brain cells.
Moreover, brain imaging studies have revealed structural changes in areas responsible for thinking, memory, and movement in individuals affected by Lewy body dementia. The formation of Lewy bodies is closely tied to neuronal damage and loss, which play a significant role in the development of symptoms associated with Lewy body dementia.
Understanding these brain abnormalities is essential in comprehending the underlying mechanisms of this neurodegenerative disease and can guide researchers in developing potential treatments.
Neurotransmitter Imbalance

In Lewy body dementia, an imbalance in neurotransmitters like dopamine and acetylcholine occurs. These neurotransmitters play crucial roles in functions such as motor control, cognition, memory, and learning.
The disruption in neurotransmitter levels by Lewy bodies contributes to the various symptoms observed in individuals with this form of dementia.
Dopamine Deficiency Impact
Dopamine deficiency in Lewy Body Dementia causes movement symptoms that closely resemble those seen in Parkinson's disease. This deficiency impacts the coordination, muscle control, and overall motor function of individuals.
Here are three key points to understand the impact of dopamine deficiency in LBD:
- Lewy bodies affect dopamine-producing neurons, leading to motor issues in LBD.
- Dopamine, an essential neurotransmitter, plays a significant role in controlling movement and regulating mood.
- Imbalance in dopamine levels can result in challenges related to coordination and muscle control.
Treatment strategies for LBD often target dopamine deficiency to help alleviate the movement symptoms experienced by individuals.
Acetylcholine Disruption Effect
Disruption of acetylcholine, an essential neurotransmitter, greatly contributes to cognitive and memory impairment in individuals with Lewy body dementia. In this condition, Lewy bodies in the brain lead to decreased levels of acetylcholine, impacting communication between nerve cells.
This imbalance of acetylcholine results in difficulties in thinking, reasoning, and processing information. Medications that target acetylcholine levels may help improve cognitive symptoms in individuals with Lewy body dementia.
The disruption of acetylcholine function plays a significant role in the cognitive decline observed in patients with Lewy body dementia. It's important to address this neurotransmitter imbalance to help manage cognitive and memory impairments associated with this challenging condition.
Serotonin Level Influence
Our exploration now shifts to the impact of serotonin levels, a neurotransmitter essential for mood regulation and cognitive function, in the context of Lewy body dementia.
- Imbalance in serotonin levels is linked to the development of Lewy body dementia.
- Serotonin plays an essential role in regulating mood, sleep, and cognitive function affected in Lewy body dementia.
- Low levels of serotonin can contribute to cognitive decline and behavioral changes seen in Lewy body dementia.
Understanding and addressing serotonin imbalances could offer new avenues for managing Lewy body dementia symptoms.
Research suggests that serotonin dysfunction may exacerbate the progression of symptoms in individuals with this condition. By focusing on serotonin levels, caregivers and healthcare providers can potentially enhance the quality of life for those living with Lewy body dementia.
Age as a Factor

With advancing age, individuals over 60 face a greatly heightened risk of developing Lewy body dementia. As we grow older, the prevalence of Lewy body dementia increases, particularly affecting older adults.
Aging brings about changes in brain structure and function, making older individuals more susceptible to the accumulation of abnormal protein deposits in the brain, known as Lewy bodies. These deposits are a key characteristic of the disease.
Understanding how aging impacts brain health is vital in addressing the risk factors and potential causes of Lewy body dementia. It's essential to take into account age as a significant factor when looking at the development of this condition.
Oxidative Stress

One may wonder how oxidative stress impacts the development of Lewy body dementia. Here are some key points to ponder:
- Imbalance between free radicals and antioxidants: Oxidative stress arises when there's an excess of free radicals, highly reactive molecules that can harm cells. In Lewy body dementia, this imbalance contributes to neurodegeneration.
- Role of antioxidants: Antioxidants play an essential role in combating oxidative stress by neutralizing free radicals. By protecting neurons from oxidative damage, antioxidants provide necessary neuronal protection in the context of Lewy body dementia.
- Mitochondria dysfunction and energy production: In Lewy body dementia, oxidative stress is often linked to mitochondria dysfunction and impaired energy production. This connection underscores the importance of addressing oxidative stress pathways in research for potential therapeutic interventions against Lewy body dementia.
Understanding the impact of oxidative stress on Lewy body dementia is crucial in developing effective strategies for treatment and management. By focusing on reducing oxidative stress, researchers aim to uncover new avenues for combating this complex neurodegenerative condition.
Inflammation

In Lewy body dementia, inflammation in the brain is a vital factor believed to influence disease development and progression. When the brain experiences chronic inflammation, it can lead to neuronal damage and contribute to the formation of Lewy bodies, abnormal protein clumps that disrupt normal brain function.
This inflammatory process not only causes neuronal damage but also exacerbates cognitive decline in individuals with Lewy body dementia. Research has shown that targeting inflammation may offer potential therapeutic strategies for managing this condition. By understanding the role of inflammation in Lewy body dementia, we can develop new treatment approaches aimed at reducing neuroinflammation and protecting brain health.
It's essential to address inflammation in the brain to prevent further damage and slow down the progression of Lewy body dementia.
Stay tuned to learn about how mitochondrial dysfunction also plays a role in the development of this condition.
Mitochondrial Dysfunction

Mitochondrial dysfunction in Lewy body dementia greatly impairs energy production in brain cells. This dysfunction has significant implications for neuronal health and the progression of Lewy body dementia. Here are three key points to ponder:
- Formation of Lewy Bodies: Research suggests that dysfunctional mitochondria contribute to the formation of Lewy bodies in nerve cells. These abnormal protein aggregates are characteristic of Lewy body dementia and can disrupt cellular functions.
- Neurotransmitter Synthesis: Mitochondria play an essential role in neurotransmitter synthesis, which is vital for proper cellular communication in the brain. Impaired mitochondrial function can lead to disruptions in neurotransmitter levels, affecting brain function.
- Therapeutic Strategies: Targeting mitochondrial dysfunction may offer potential therapeutic approaches for managing Lewy body dementia. By addressing energy production deficits and supporting mitochondrial health, interventions aimed at improving mitochondrial function could help alleviate symptoms and slow disease progression.
Vascular Issues

Ensuring proper blood flow and oxygen delivery is crucial in prioritizing brain health. This can be achieved through a healthy lifestyle that includes regular exercise, a balanced diet, and managing chronic conditions.
Vascular issues, such as strokes or reduced blood flow to the brain, play a significant role in the development of Lewy body dementia. When blood vessels in the brain are damaged due to problems like hypertension, diabetes, or heart disease, cognitive decline can occur, increasing the risk of dementia. These vascular issues can disrupt the delivery of oxygen and nutrients to the brain, impacting cognitive function and potentially contributing to Lewy body dementia.
Managing risk factors such as hypertension, diabetes, and heart disease through lifestyle changes and medical treatments can help reduce the risk of vascular-related dementia. Prioritizing brain health by ensuring proper blood flow and oxygen delivery is essential, and making choices like regular exercise, a balanced diet, and managing chronic conditions can support overall vascular health and reduce the likelihood of developing conditions like Lewy body dementia.
Frequently Asked Questions
What Are the Most Common Causes of Dementia With Lewy Bodies?
We comprehend that dementia with Lewy bodies can stem from abnormal protein deposits in the brain. These deposits, mainly alpha-synuclein, disrupt brain function, affecting cognition. While triggers aren't fully known, factors like age and Parkinson's history contribute.
What Are 3 Signs of Lewy Body Dementia?
We notice visual hallucinations, fluctuating attention, and movement issues as three key signs of Lewy body dementia. These symptoms, along with cognitive problems and sleep disturbances, may indicate the presence of this condition, urging further evaluation.
How Do You Prevent Lewy Body?
To prevent Lewy body dementia, we focus on managing risk factors like age, Parkinson's disease, and family history. While no guaranteed prevention exists, understanding these factors helps with early detection and care, enhancing overall quality of life.
Can Lewy Body Dementia Come on Suddenly?
Yes, Lewy Body Dementia can appear suddenly, causing rapid changes in cognition, behavior, and movement. Factors like stress, infections, or medication adjustments can trigger this abrupt onset. It can manifest as sudden fluctuations in alertness and abilities.
Are Narcissistic Personality Disorder and Lewy Body Dementia Related in Any Way?
Some research suggests that individuals with Lewy Body Dementia may exhibit traits of defining narcissistic personality disorder. However, it is important to note that having one does not necessarily cause the other. Further studies are needed to determine if there is a direct relationship between the two conditions.
Conclusion
To sum up, comprehending the causes of Lewy body dementia is like untangling a intricate puzzle. Genetic factors, alpha-synuclein protein, environmental triggers, brain abnormalities, neurotransmitter imbalance, oxidative stress, inflammation, mitochondrial dysfunction, and vascular issues all play a role in the development of this condition.
By identifying and addressing these factors early on, we can work towards slowing down the progression of Lewy body dementia and improving the quality of life for those affected. Just like putting together puzzle pieces, every piece of information is essential in solving the mystery of this disease.









