Understanding the various stages of dementia is crucial in order to provide appropriate care. This condition advances gradually through different stages distinguished by changes in cognitive functions. In the mild stage, individuals may encounter memory lapses and difficulties. The moderate stage presents more noticeable symptoms such as confusion. Severe dementia involves significant loss of response and communication skills. Symptoms range from cognitive deterioration to behavioral shifts. Tailored care is crucial, adjusting to evolving needs. Promote independence in the early stages and provide full assistance in later stages. It’s important to remember that each stage necessitates specialized care. Further insights are available to enhance your comprehension.
Key Takeaways
- Dementia progresses through mild, moderate, and severe stages with distinct symptoms.
- Mild stage features memory lapses and mild challenges in daily functioning.
- Moderate stage shows pronounced confusion, mood changes, and sleep disturbances.
- Severe stage exhibits profound cognitive decline, communication struggles, and physical limitations.
- Tailored care and support are crucial at each stage to meet changing needs effectively.
Progression of Dementia Stages
As we observe individuals affected by dementia, we witness a gradual progression through distinct stages, each marking a significant shift in cognitive abilities and daily functioning. The progression of dementia stages is important to understand as it impacts how we provide care and support to those with the condition.
From the early stages where individuals may experience mild forgetfulness and confusion to the late stages where they may lose the ability to communicate and perform daily tasks, the journey through dementia stages is marked by noticeable changes in symptoms and characteristics.
Diagnosis usually occurs around stage 4 of dementia when symptoms become more pronounced, and the need for support becomes more evident. It's important to recognize these stages to make sure appropriate care and interventions are in place. While the progression of dementia stages varies among individuals, having a clear understanding of the different stages helps us tailor our support to meet the specific needs of each person affected by dementia.
Mild Stage of Dementia

Moving through the stages of dementia, the mild stage presents individuals with memory lapses and challenges in tasks such as planning and organizing in social and work settings. In this early stage, forgetfulness may occur after reading or misplacing items, making cognitive impairments noticeable. People in the mild stage might have difficulty finding the right words or recalling object locations. Despite these mild symptoms, individuals may still be able to function independently in certain aspects of daily life. To better understand the characteristics of the mild stage of dementia, let's explore the following table:
| Mild Stage of Dementia Symptoms |
|---|
| Memory lapses |
| Challenges in planning and organizing tasks |
| Forgetfulness after reading |
| Difficulty recalling object locations |
In this stage, it's essential to provide support and understanding to those experiencing these challenges, helping them navigate through their daily activities with patience and compassion.
Moderate Stage of Dementia
Moving through the moderate stage of dementia brings about more pronounced symptoms such as confusion and mood changes for individuals. Memory loss becomes more severe, affecting personal information like addresses and phone numbers. Sleep patterns may also shift, leading to restlessness and wandering tendencies.
During this stage, caregivers should consider respite care options to provide temporary breaks and support. The moderate stage of dementia requires longer duration and increased attention compared to earlier stages. It's essential to monitor individuals closely, ensuring their safety and well-being.
Encouraging a calming environment and maintaining a consistent routine can help alleviate some of the distress caused by the heightened symptoms. Understanding the challenges that come with the moderate stage of dementia is vital for providing effective care and support. By staying informed and seeking assistance when needed, caregivers can navigate this stage with patience and compassion.
Severe Stage of Dementia

Entering the severe stage of dementia brings about a profound loss of response to the environment and communication for individuals. In this stage, movement control is severely impaired, making daily activities such as walking and swallowing challenging. Awareness of recent experiences and surroundings diminishes drastically, making it difficult for individuals to understand their environment. Communication becomes a struggle, and individuals may find it hard to express pain or discomfort, highlighting the need for attentive caregiving.
Moreover, those in the severe stage of dementia are more vulnerable to infections, particularly pneumonia, due to their weakened immune systems and decreased ability to fight off illnesses. This vulnerability emphasizes the importance of close monitoring and timely medical care to prevent complications.
Understanding and providing care for individuals in the severe stage of dementia require patience, compassion, and specialized attention. By being aware of their needs and ensuring a safe and comfortable environment, caregivers can support these individuals in their daily struggles and provide the necessary assistance to maintain their well-being.
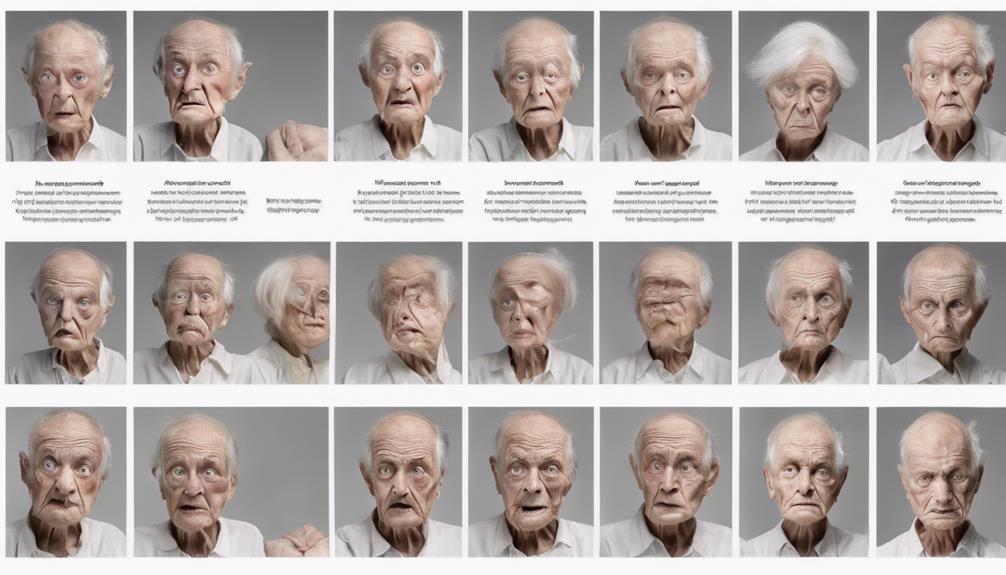
Symptoms in Different Stages
As dementia progresses through its stages, symptoms manifest in varying degrees of cognitive decline and behavioral changes. In the early stages, individuals may experience memory impairment, such as forgetfulness and difficulty with planning.
As the disease advances to the middle stages, pronounced confusion, mood changes, and trouble recalling personal information become more prominent. Communication difficulties may also arise during this phase.
In late-stage dementia, there's severe loss of response to the environment, along with significant physical decline. Walking difficulties, swallowing problems, and vulnerability to infections like pneumonia are common in this stage. It's important to provide appropriate care and support to individuals with late-stage dementia as they face these challenges.
Understanding the progression of symptoms throughout the stages of dementia is essential for caregivers and healthcare professionals to provide the best possible care for those affected by this condition.
Care Considerations for Each Stage

When caring for individuals in different stages of dementia, it's essential to adapt our approach to meet their changing needs.
In the early stages, providing support while encouraging independence can help maintain a sense of self-sufficiency.
As the disease progresses to advanced stages, more complete care and assistance become necessary to guarantee the individual's safety and well-being.
Early Stage Care
During the early stage of dementia, we focus on providing tailored support for memory-related challenges while fostering independence in daily activities. Individuals may experience memory lapses, forgetfulness, and difficulties in social settings. Caregivers should offer reminders and emotional support while monitoring changes in cognitive abilities. It's essential to help with object locations and assist in planning for future care needs. Below is a table summarizing key aspects of early stage care:
| Care Aspect | Description |
|---|---|
| Memory Challenges | Help with forgetfulness and word recall |
| Independence | Encourage self-reliance in daily tasks |
| Emotional Support | Provide comfort and reassurance |
| Planning | Assist in organizing and planning future activities |
| Cognitive Abilities | Monitor changes in cognitive functions |
Advanced Stage Support
In advanced stage dementia, we prioritize specialized care to address severe cognitive decline and physical limitations. At this stage, individuals require assistance with basic activities of daily living, such as eating, bathing, and dressing. Ensuring their comfort, safety, and quality of life becomes paramount. Vital care plays a critical role in managing symptoms and enhancing their overall well-being.
Caregivers need additional support and education to provide best care for those in late-stage dementia. It's essential to create a supportive environment that promotes dignity and respect for the individual. By focusing on specialized care, we can help individuals navigate the challenges of advanced stage dementia with compassion and understanding.
Frequently Asked Questions
How Long Does Dementia Take to Progress?
Dementia progression time varies widely based on factors such as age, health, and type of dementia. It's unpredictable, with some individuals living 4 to 8 years post-diagnosis, while others may endure up to 20 years.
At What Stage of Dementia Do They Sleep a Lot?
In the late stages of dementia, we notice increased daytime sleepiness and longer napping periods. Excessive sleeping can affect daily activities and quality of life. Monitoring changes in sleep patterns and promoting consistent routines can help manage this symptom.
At What Stage of Dementia Does Aggression Occur?
Aggression in dementia typically surfaces during the middle to late stages. Triggers like confusion and fear can lead to verbal or physical outbursts. Calm environments and personalized strategies help manage aggression effectively, enhancing the well-being of individuals.
What Causes Dementia Patients to Suddenly Get Worse?
When dementia patients suddenly worsen, factors like infections, changes in medication, dehydration, stress, hospitalization, or caregiver burnout could be culprits. It's essential to address triggers promptly to provide the best care and support for these individuals.
Which Type of Bathroom Option is More Suitable for Each Stage of Dementia?
At various dementia stages, safety and accessibility dictate bathroom choices. The walkin tub versus walkin shower debate often hinges on specific needs—tubs may aid those needing assisted baths, while showers offer quicker access for others with mobility aids, ensuring a secure and dignified bathing experience at every stage.
Conclusion
To summarize, understanding the various stages of dementia is essential for providing appropriate care and support to individuals living with this condition.
As the saying goes, 'knowledge is power,' and knowing what to expect at each stage can help families and caregivers navigate the challenges ahead with confidence and compassion.
By staying informed and being proactive in addressing the needs of those with dementia, we can make a positive difference in their quality of life.