Excess weight and obesity, throat muscle relaxation, anatomical factors, medical conditions, and lifestyle habits are key causes of obstructive sleep apnea. Carrying extra weight can relax throat muscles, causing breathing interruptions. Anatomical issues like enlarged tonsils or a deviated septum may block the airway. Medical conditions such as hypothyroidism or allergies can worsen OSA symptoms. Smoking and alcohol use can also lead to airway inflammation. Understanding these factors is essential in managing obstructive sleep apnea. Addressing these causes can improve sleep quality and overall health.
Key Takeaways
- Excess weight and obesity relax throat muscles, causing airway blockage.
- Throat and tongue muscle relaxation lead to breathing interruptions during sleep.
- Anatomical factors like enlarged tonsils and structural abnormalities contribute to OSA.
- Medical conditions such as hypothyroidism and excess growth increase OSA risk.
- Lifestyle habits like smoking and a sedentary lifestyle worsen OSA symptoms.
Excess Weight and Obesity
Excess weight and obesity commonly cause obstructive sleep apnea (OSA) by relaxing throat and tongue muscles during sleep, leading to airway blockage. When we carry excess weight, especially around the neck area, it can put pressure on our airways. As a result, the throat muscles loosen up, and the tongue may fall back, obstructing the normal flow of air. This blockage leads to pauses in breathing during sleep, causing disruptions in the oxygen supply to our body.
Furthermore, weight gain increases the risk of developing OSA greatly. Individuals with a higher neck circumference are particularly vulnerable to this condition. The extra fat in the neck region can compress the airway, making it harder for air to pass through. Maintaining a healthy weight is essential in reducing the chances of throat muscles relaxing and causing airway blockage during sleep. It's vital to be mindful of our weight to promote better sleep and overall well-being.
Throat and Tongue Muscle Relaxation
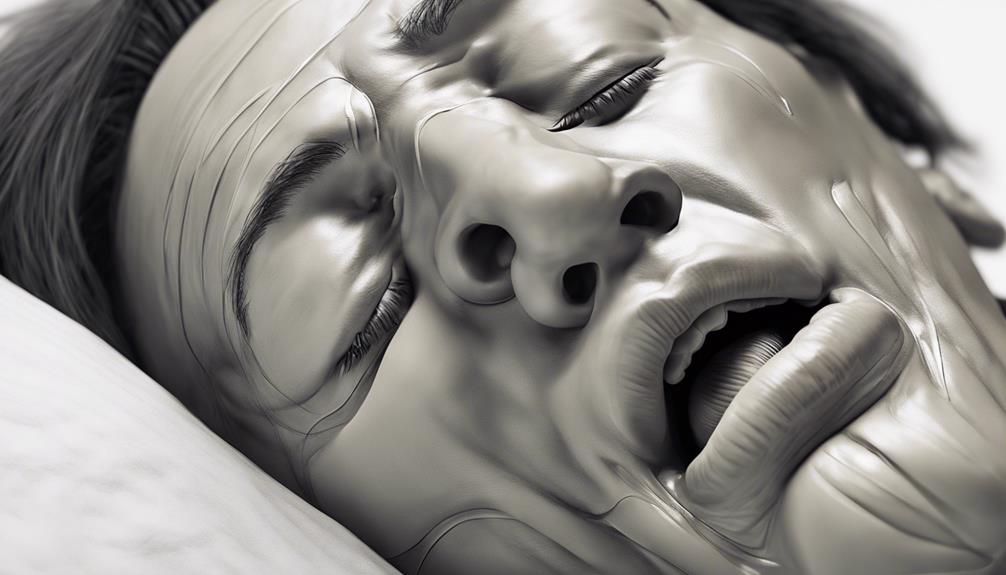
Throat and tongue muscle relaxation plays a critical role in causing airway blockage in individuals with obstructive sleep apnea (OSA). When these muscles relax excessively during sleep, they can obstruct the airway, leading to breathing interruptions. Factors such as excess weight and obesity contribute to the relaxation of throat muscles, exacerbating the condition. Additionally, individuals with larger neck circumferences are at a higher risk of experiencing throat muscle relaxation, which can further contribute to airway blockage.
| Throat and Tongue Muscle Relaxation | Airway Blockage | Contributing Factors |
|---|---|---|
| Excessive relaxation during sleep | Breathing interruptions | Excess weight and obesity |
| Risk of OSA development | Throat muscle relaxation | Larger neck circumference |
| Impact on airway obstruction | Tongue muscle relaxation | Head and throat anatomy |
Understanding the importance of maintaining healthy throat and tongue muscles can help in managing OSA and reducing the risk of complications associated with this condition.
Anatomical Factors
Anatomical factors play a significant role in contributing to obstructive sleep apnea, including excess weight leading to fat deposits around the neck. Enlarged tonsils or adenoids can obstruct the airway during sleep, causing breathing interruptions. Structural abnormalities like a deviated septum or a narrow airway can also increase the risk of obstructive sleep apnea. Overgrowth of soft tissues in the throat, such as the uvula or soft palate, can further contribute to airway blockage in OSA. Additionally, the shape of the head and neck, especially with a round head or thick neck circumference, can be anatomical factors influencing obstructive sleep apnea.
Understanding these anatomical factors is vital in managing and treating obstructive sleep apnea. By addressing issues such as excess weight, enlarged tonsils, structural abnormalities, and soft tissue overgrowth, healthcare providers can develop personalized treatment plans that target the specific anatomical factors contributing to the condition. Identifying these factors early on can lead to more effective interventions and improved outcomes for individuals experiencing obstructive sleep apnea.
Medical Conditions

Certain medical conditions can greatly contribute to the development of obstructive sleep apnea. Conditions like hypothyroidism and excess growth can affect the structure of the airway, making it more prone to collapse during sleep. Nasal conditions such as allergies, a deviated septum, or nasal polyps can lead to airway blockages, increasing the risk of obstructive sleep apnea. Smoking and alcohol abuse can relax the throat muscles, causing them to collapse and obstruct the airway during sleep, worsening the condition. Medical conditions that congest the upper airways, like chronic sinusitis, can also contribute to the occurrence of obstructive sleep apnea. Additionally, obesity-related conditions such as metabolic syndrome can further obstruct the airway, making it harder to breathe properly during sleep. It's essential to address these medical conditions to improve sleep quality and overall health.
| Medical Conditions | Impact on Obstructive Sleep Apnea |
|---|---|
| Hypothyroidism | Affects airway structure |
| Excess Growth | Increases risk of airway collapse |
| Nasal Conditions | Leads to airway blockages |
| Smoking & Alcohol Abuse | Cause throat muscle relaxation |
| Upper Airway Congestion | Contributes to airway obstruction |
Allergies and Lifestyle Habits
Allergies can make it harder to breathe while you sleep, especially if they cause stuffy noses and swollen airways.
Smoking can make sleep apnea worse because it relaxes the throat muscles and can narrow the air passages even more.
Not moving around enough can also affect how well you breathe while you snooze.
Allergies Impact Breathing
When managing allergies that impact breathing, it's important to take into account lifestyle habits like smoking, which can worsen airway inflammation and exacerbate obstructive sleep apnea symptoms.
Allergies such as those triggered by dust mites, pet dander, pollen, and mold spores can lead to nasal congestion and inflammation in the airways, causing blockages in the upper airway during sleep. These blockages make it harder to breathe properly during the night, contributing to the symptoms of obstructive sleep apnea.
To reduce the impact of allergies on breathing, it's essential to identify and avoid triggers, consider medications or allergy shots, and address lifestyle habits that can worsen airway inflammation, such as smoking.
Smoking Worsens Sleep Apnea
Smoking greatly worsens obstructive sleep apnea by causing inflammation and irritation in the airways. Tobacco smoke irritates the upper airway, leading to swelling and increased obstruction during sleep. Quitting smoking is essential for improving sleep apnea symptoms and reducing complications.
Allergies triggered by smoking can worsen airway congestion, exacerbating obstructive sleep apnea. Lifestyle habits like smoking directly impact the severity and progression of this condition. To alleviate these issues, consider smoking cessation and avoiding exposure to smoke.
Sedentary Lifestyle Affects Breathing
Our level of physical activity directly impacts our breathing patterns and overall respiratory health, playing a significant role in the development and management of obstructive sleep apnea. A sedentary lifestyle contributes to weight gain, a major risk factor for sleep apnea. It can lead to muscle weakness in the throat and tongue, increasing the likelihood of airway blockage during sleep.
Sedentary individuals are more prone to allergies, causing nasal congestion that further obstructs the airway, worsening sleep apnea. Regular exercise improves respiratory function, reducing the risk of breathing difficulties during sleep. Adopting an active lifestyle aids in weight management, potentially easing the severity of obstructive sleep apnea symptoms.
Weight Gain Impact

When it comes to obstructive sleep apnea, our weight plays a vital role in impacting our breathing patterns. Excess weight can lead to the relaxation of muscles in our airways during sleep, causing potential blockages.
Understanding the connection between weight gain and breathing is essential in managing obstructive sleep apnea effectively.
Weight and Airway
Weight gain greatly increases the risk of obstructive sleep apnea by up to six times due to the impact on throat and tongue muscle relaxation during sleep, leading to airway blockage.
To understand the connection between weight and airway in obstructive sleep apnea, consider the following:
- Excess weight can cause throat muscles to relax excessively, contributing to airway blockage.
- Obesity may lead to relaxation of tongue muscles, further obstructing the airway.
- Increased neck circumference from weight gain can compress the airway, worsening OSA risk.
- Middle-aged adults are particularly susceptible to OSA due to the effects of excess weight on airway muscles.
Understanding these factors can help in taking proactive steps to manage weight and reduce the risk of obstructive sleep apnea.
Obesity and Breathing
Excessive weight and obesity greatly impact breathing patterns, exacerbating the risk of obstructive sleep apnea. When we gain excess weight, our throat and tongue muscles can relax too much during sleep, leading to airway blockage. This blockage can cause breathing compromise, making it harder for air to flow freely in and out of our lungs.
Additionally, having a larger neck circumference due to obesity can further contribute to upper airway narrowing, increasing the likelihood of experiencing obstructive sleep apnea. It's essential to maintain a healthy weight to reduce the risks associated with OSA.
Narrow Throat
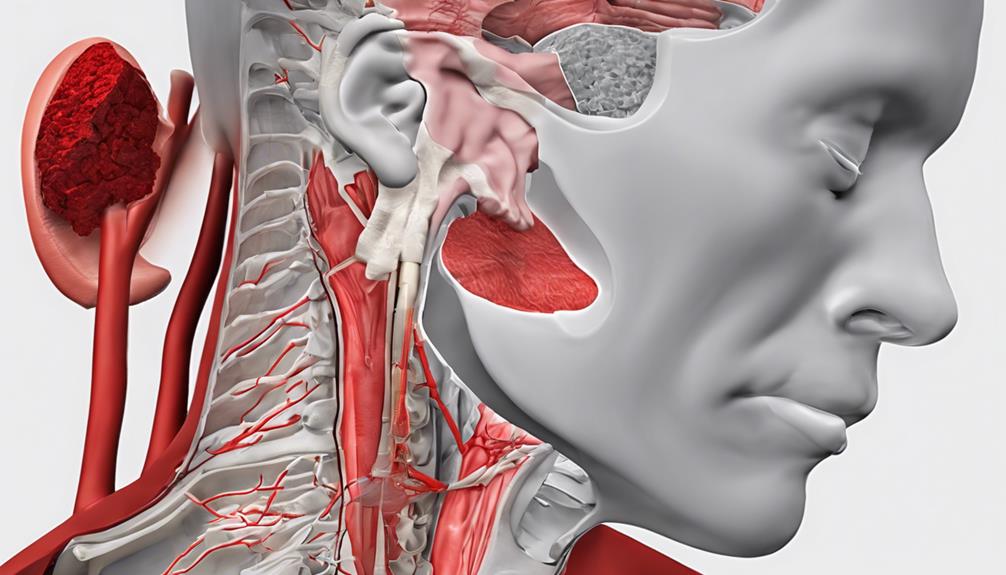
Addressing a narrow throat can play a significant role in understanding the causes of obstructive sleep apnea. Here are some key points to take into account:
- Higher Risk: Individuals with a narrow throat are at a higher risk of developing obstructive sleep apnea due to the potential for airway blockages.
- Breathing Difficulties: The narrowing of the throat can result in breathing difficulties, especially during sleep, leading to interruptions in breathing patterns.
- Airway Blockages: Anatomical factors like a narrow throat can contribute to obstructive sleep apnea by restricting airflow, causing blockages in the airway.
- Interventions and Changes: Addressing a narrow throat as a factor in obstructive sleep apnea may involve medical interventions such as surgeries or lifestyle changes like weight management to alleviate symptoms and improve breathing quality.
Understanding how a narrow throat impacts breathing and contributes to obstructive sleep apnea can guide individuals towards appropriate medical interventions and lifestyle adjustments to improve their overall sleep quality and well-being.
Hypothyroidism

Hypothyroidism, a condition characterized by insufficient hormone production in the thyroid gland, can greatly impact the risk of developing obstructive sleep apnea. When the thyroid gland fails to produce enough hormones, it can lead to weight gain and relaxation of the throat muscles. These factors contribute to the increased likelihood of airway blockage during sleep, a common feature of obstructive sleep apnea.
Symptoms of untreated hypothyroidism, like fatigue and muscle weakness, can worsen the condition. However, proper management through medication and lifestyle changes can help reduce the risk. It's vital for individuals with hypothyroidism to regularly monitor their thyroid hormone levels and adhere to treatment plans.
Smoking and Alcohol Abuse

Smoking and alcohol abuse are significant factors that can worsen obstructive sleep apnea by causing airway inflammation and muscle relaxation. Here are four important points to keep in mind:
- Smoking irritates the upper airway, leading to inflammation that increases the risk of airway blockage during sleep. This can make it harder to breathe properly, exacerbating the symptoms of sleep apnea.
- Exposure to tobacco smoke can also contribute to the relaxation of the upper airway muscles, which can further worsen or even cause obstructive sleep apnea. Avoiding tobacco smoke is essential for managing this condition.
- Alcohol consumption is another key element to take into account, as it can relax the throat muscles and interfere with the brain's ability to control breathing during sleep. This can make the airway more likely to collapse, making breathing difficult.
- Consuming alcohol before bedtime can further collapse the upper airway, making it even more challenging to breathe properly while sleeping. Addressing both smoking and alcohol abuse as modifiable risk factors is vital for improving the management and outcomes of obstructive sleep apnea.
Frequently Asked Questions
What Is the Most Common Cause of Obstructive Sleep Apnea?
The most common cause of obstructive sleep apnea is the relaxation of throat and tongue muscles during sleep, leading to airway blockage. Excess weight, neck circumference, anatomy, head shape, and medical conditions can also contribute.
Who Is Most Likely to Have Obstructive Sleep Apnea?
We are more likely to have obstructive sleep apnea if we are men, have a family history, belong to certain ethnicities, age, or have a large neck circumference. Hormone replacement therapy in postmenopausal women may lower risk.
What Causes Sleep Apnea in People Who Are Not Overweight?
We explore the causes of sleep apnea in non-overweight individuals. Factors like anatomical issues, structural abnormalities, allergies, and certain medical conditions can contribute. Lifestyle choices such as smoking, alcohol, and sedatives may worsen the condition.
Can You Fix Obstructive Sleep Apnea?
Yes, we can fix obstructive sleep apnea. Treatment options like CPAP therapy, lifestyle changes, oral appliances, and surgery are available. Seeking important treatment is vital as untreated sleep apnea can lead to serious health complications.
Conclusion
To sum up, the causes of obstructive sleep apnea are like a puzzle with many pieces. Excess weight, throat muscle relaxation, anatomical factors, medical conditions, allergies, lifestyle habits, weight gain impact, narrow throat, hypothyroidism, smoking, and alcohol abuse all play a role in this condition. Moreover, it is important to note that while these factors contribute to obstructive sleep apnea, central sleep apnea risk factors involve distinct mechanisms. These typically relate to dysfunction in how the brain controls breathing during sleep. Both conditions, though different, can overlap in some individuals, complicating the diagnosis and treatment process.
By understanding these causes, we can take steps to address them and improve our sleep quality. Remember, knowledge is power when it comes to managing your health.









