Brainstem dysfunction disrupts breathing signals in central sleep apnea. Issues like neurological diseases, brainstem damage, and congenital factors contribute. The brainstem regulates breath coordination importantly. Incorrect signals cause pauses in breathing during sleep. Impaired breathing regulation affects brain signaling to muscles. Heart failure, stroke, and opioids can hinder proper breathing. Conditions such as Parkinson's and Chiari malformation also influence central sleep apnea. Opioids suppress respiratory centers, worsening the condition. Modifying opioid dosage or special breathing devices may help. Understanding these causes is important in managing central sleep apnea effectively. Subtly uncover more about central sleep apnea's causes by exploring further.
Key Takeaways
- Brainstem dysfunction disrupts respiratory signals during sleep.
- Impaired breathing regulation from conditions like heart failure can cause central sleep apnea.
- Lack of proper brain signaling leads to pauses in breathing patterns.
- Neurological diseases like stroke and Parkinson's influence central sleep apnea.
- Opioid use suppresses respiratory centers, increasing the risk of central sleep apnea.
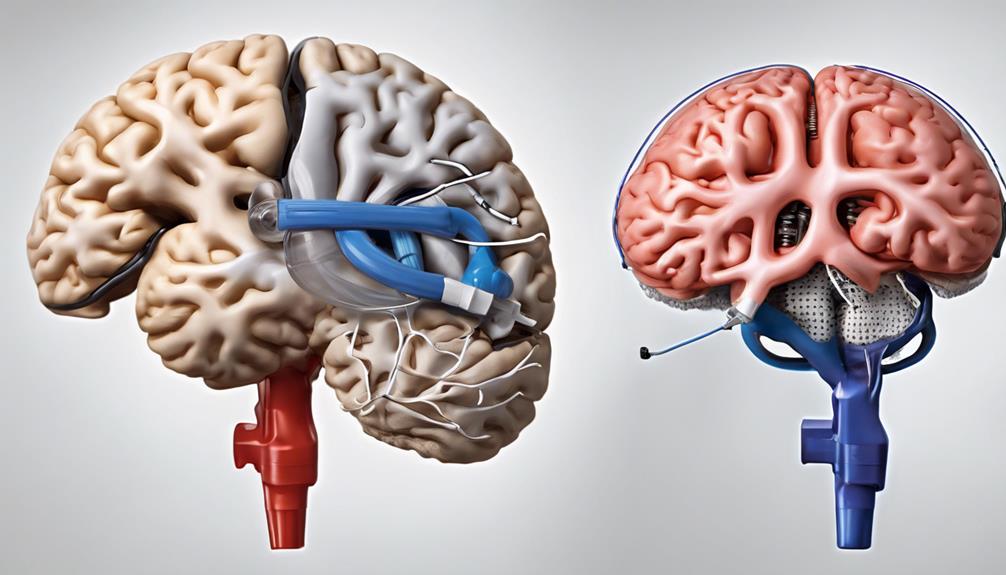
Brainstem Dysfunction
Brainstem dysfunction disrupts the brain's ability to send proper signals for breathing during sleep, a key cause of central sleep apnea. When the brainstem, the essential area at the base of the brain responsible for regulating essential bodily functions, experiences impairment, it can lead to disruptions in respiratory control.
Various factors such as neurological diseases, brainstem damage from injuries like strokes, or congenital issues affecting the brainstem can all contribute to the development of central sleep apnea. The brainstem's role in respiratory regulation is critical, as any impairment in its respiratory centers can impact breathing patterns during sleep. In particular, damage to the brainstem can disrupt the communication between the brain and muscles that control breathing, leading to periods of apnea or shallow breaths during sleep. Additionally, neurological conditions that affect brain function, including some causes of frontotemporal dementia, may also interfere with the respiratory centers, further exacerbating sleep-related breathing disorders. Understanding these connections highlights the importance of addressing underlying neurological issues when managing central sleep apnea effectively.
Understanding how brainstem dysfunction can interfere with the coordination of respiratory muscles highlights the importance of this region in maintaining proper breathing cycles. Addressing issues related to brainstem impairment is fundamental in managing central sleep apnea and promoting healthy respiratory function during sleep.
Impaired Breathing Regulation
Impaired breathing regulation in central sleep apnea occurs when the brain fails to properly signal the breathing muscles. This disruption in respiratory control mechanisms can stem from various brainstem conditions, such as heart failure, stroke, and spinal cord injuries. Additionally, drug-induced apnea, particularly from opioid medications, can suppress the respiratory rhythm generator, contributing to central sleep apnea. Furthermore, high-altitude periodic breathing, often experienced above 8,000 feet, can also interfere with breathing regulation and lead to central sleep apnea.
It's important to recognize that impaired breathing regulation is a significant factor in central sleep apnea, affecting how our brain communicates with the muscles responsible for breathing. Understanding the various causes, including brainstem conditions, drug-induced apnea, and high-altitude periodic breathing, can shed light on why this impairment occurs. By being aware of these factors, individuals and healthcare providers can work together to address and manage central sleep apnea more effectively.
Lack of Proper Brain Signals
The absence of adequate brain signals to control breathing during sleep causes central sleep apnea, resulting in interruptions to the normal respiratory rhythm. In central sleep apnea, the brain fails to send the necessary signals to the muscles responsible for breathing, leading to pauses in breathing during sleep. These interruptions disrupt the regular respiratory pattern, affecting the body's oxygen levels and overall well-being.
Various conditions impacting the brainstem, such as heart failure, stroke, or neurological disorders, can contribute to the development of central sleep apnea by interfering with the brain's signaling process. Additionally, the use of opioid medications can suppress the brain's respiratory centers, further exacerbating the condition. Understanding the role of proper brain signals in controlling breathing during sleep is crucial for formulating an effective treatment plan to manage central sleep apnea.
Neurological Conditions Influence

Neurological conditions play a significant role in influencing the brain's signaling to breathing muscles, contributing to the development of central sleep apnea. Understanding how these conditions impact the brainstem, which controls breathing, is vital for diagnosing and treating this sleep disorder effectively.
- Disruption of Brain Signaling: Conditions like stroke, Parkinson's disease, and brainstem tumors can disrupt the brain's ability to send proper signals to the breathing muscles, leading to central sleep apnea.
- Brainstem Damage: Damage to the brainstem, responsible for regulating respiratory functions, can result in central sleep apnea by affecting the normal breathing patterns during sleep.
- Neurological Disorders: Diseases such as multiple system atrophy, Chiari malformation, and congenital central hypoventilation syndrome are neurological disorders that may contribute to the development of central sleep apnea.
- Injuries to the Brainstem: Trauma or surgeries causing injuries to the brainstem can interfere with the respiratory control mechanisms, potentially leading to central sleep apnea.
Opioid Use and Central Sleep Apnea
Opioid use can trigger central sleep apnea by suppressing the brain's respiratory centers, leading to decreased respiratory effort during sleep. This condition, known as opioid-induced central sleep apnea, is more prevalent in individuals using high doses or undergoing long-term opioid therapy. The risk of developing central sleep apnea from opioids rises with the potency and duration of medication use.
To understand the impact of opioid use on central sleep apnea better, let's explore the factors influencing this relationship in the table below:
| Factors | Impact on Central Sleep Apnea |
|---|---|
| High doses of opioids | Increase the likelihood of developing the sleep disorder |
| Long-term opioid therapy | Raises the risk of central sleep apnea |
| Potency and duration of opioids | Correlate with an elevated chance of experiencing the condition |
When faced with opioid-induced central sleep apnea, treatment options may involve modifying opioid dosage, changing medications, or utilizing specialized breathing devices to alleviate symptoms and improve sleep quality.
Frequently Asked Questions
Which of the Following Is a Cause of Central Sleep Apnea?
Certain conditions such as heart failure, stroke, opioid use, high-altitude living, and even treatment with positive airway pressure can lead to central sleep apnea. Recognizing these factors is crucial for effective management.
What Is the Most Common Cause of Sleep Apnea?
The most common cause of sleep apnea is obstructive sleep apnea, where the airway becomes blocked during sleep. This can lead to pauses in breathing and disrupted sleep patterns. Seeking medical advice is essential for proper diagnosis and treatment.
How Rare Is Central Sleep Apnea?
Central sleep apnea is relatively rare, affecting less than 10% of those with sleep disorders. It's more common in specific groups like heart failure patients. Even in healthy individuals, brief central apneas during sleep changes are possible.
Can Central Sleep Apnea Be Corrected?
We believe central sleep apnea can be corrected, often requiring a tailored approach. Treatment options such as positive airway pressure, oxygen therapy, and addressing underlying health conditions can help manage this condition effectively over time.
Conclusion
To sum up, the reasons behind central sleep apnea can be compared to a tangled web of brain signals and neurological conditions that disrupt our breathing during sleep.
It's like a puzzle where pieces don't quite fit together, leading to interruptions in our body's natural rhythm.
Understanding these causes is vital in finding effective treatments and improving sleep quality.
By unraveling the complexities of central sleep apnea, we can work towards a restful night's sleep.