Untreated sleep apnea can lead to fatal consequences. It increases the risk of sudden cardiac death and lowers oxygen levels with breathing interruptions. Timely treatment is essential to reduce these life-threatening risks. Seek medical advice promptly to address this condition. Remember, taking care of sleep apnea is important for your health and well-being.
Key Takeaways
- Untreated sleep apnea increases sudden cardiac death risk.
- Breathing pauses can lead to fatal outcomes during sleep.
- Severe cases of sleep apnea elevate mortality risk.
- Timely treatment reduces complications and mortality.
- Effective interventions can prevent fatal consequences.
Risks of Untreated Sleep Apnea
Untreated sleep apnea poses serious risks to our health, including an increased likelihood of sudden cardiac death. When we've sleep apnea, our breathing repeatedly stops and starts during sleep, leading to low oxygen levels in the body. This lack of oxygen can have severe consequences on our overall well-being. Individuals with untreated sleep apnea are at higher risk of experiencing strokes and heart arrhythmias, which can be life-threatening conditions. Additionally, this sleep disorder is also linked to the development of other serious health issues such as diabetes, heart failure, and cognitive impairment.
Fortunately, there are effective treatments available for sleep apnea that can significantly reduce these risks and improve our health outcomes. Seeking medical attention and adhering to prescribed treatments can help alleviate the dangers associated with untreated sleep apnea. By addressing this condition proactively, we can safeguard our health and well-being for the long term.
Cardiovascular Impact of Sleep Apnea

Sleep apnea's cardiovascular impact manifests through an increased risk of abnormal heart rhythms, such as atrial fibrillation. This condition puts a strain on the heart, leading to a higher likelihood of heart failure.
Untreated sleep apnea is concerning as it's associated with an elevated risk of strokes and cardiovascular disease. Additionally, it can contribute to the development of atherosclerosis, a condition that narrows the arteries and increases the risk of heart issues. It is crucial to address sleep apnea early, as persistent disruptions in breathing during sleep can strain the cardiovascular system, further exacerbating potential health problems. Common sleep apnea risk factors include obesity, age, smoking, and a family history of the condition. Proper diagnosis and treatment can significantly reduce the risk of long-term complications and improve overall quality of life.
The disrupted sleep patterns caused by sleep apnea can further exacerbate circulatory issues and put additional strain on the cardiovascular system. Understanding these connections highlights the importance of managing sleep apnea to protect the heart and overall cardiovascular health.
Neurological Effects and Sleep Apnea
Disruptions in breathing patterns during sleep due to sleep apnea can have significant impacts on neurological functions. When breathing pauses occur, the brain may not receive enough oxygen, leading to neurological symptoms like numbness and tingling. These breathing disruptions can affect brain health and cognitive functions, potentially increasing the risk of dementia.
Managing sleep apnea is essential to reduce the chances of cognitive decline and the development of serious conditions like dementia. Seeking treatment for sleep apnea is vital for maintaining brain health and minimizing the risk of neurological consequences.
Fatal Complications of Sleep Apnea
Sleep apnea can have fatal consequences if left untreated, such as an increased risk of sudden cardiac death or even the possibility of not breathing after pauses during sleep, leading to severe outcomes.
Shared risk factors between sleep apnea and sudden death highlight the necessity of timely intervention and appropriate treatment to mitigate these lethal risks.
Effective treatments can greatly reduce the chances of fatal complications associated with sleep apnea, underscoring the importance of seeking medical advice promptly.
Deadly Risks of Apnea
Untreated severe cases of sleep apnea pose a significant risk of sudden cardiac death. When sleep apnea isn't addressed, serious consequences can arise, including:
- Increased risk of mortality, particularly linked to the severity of breathing disruptions during sleep.
- Complications such as accidents from daytime sleepiness and higher chances of developing type 2 diabetes.
- Severe cases may lead to nonalcoholic fatty liver disease and post-surgery complications.
- Older or critically ill patients with untreated sleep apnea face an elevated risk of sudden death during sleep due to breathing pauses.
- Risks of cardiovascular disease are heightened, making it important to address sleep apnea promptly to prevent these potentially fatal outcomes.
Lethal Consequences of Apnea
Severe cases of sleep apnea can lead to fatal complications if not addressed promptly and effectively. Untreated sleep apnea increases the risk of sudden cardiac death, especially when breathing pauses during sleep aren't resolved. Shared risk factors between sleep apnea and sudden death underscore the importance of this condition.
However, there's hope. Effective treatments exist that can greatly reduce the risk of fatal consequences associated with sleep apnea. Seeking medical consultation promptly and following through with appropriate treatment can help prevent chronic diseases and potential lethal outcomes of untreated sleep apnea.
It's vital to recognize the significance of managing severe cases of sleep apnea to safeguard against the life-threatening implications it may pose.
Signs of Sleep Apnea Fatality

In some cases, the signs of potential fatality related to sleep apnea may include a heightened risk of sudden cardiac death. Here are five key indicators that one should be aware of:
- Untreated obstructive sleep apnea can lead to an increased risk of sudden cardiac death, where the heart stops beating during sleep.
- Death during sleep can occur if breathing doesn't resume after pauses caused by sleep apnea, highlighting the critical need for intervention.
- Severe cases of obstructive sleep apnea can elevate the risk of mortality, emphasizing the importance of timely treatment.
- Shared risk factors exist between sleep apnea and sudden death, underscoring the necessity of addressing sleep apnea promptly.
- Effective treatment of sleep apnea can significantly reduce the risk of complications and mortality, offering hope for those affected by this condition.
It is important to recognize these signs and seek help promptly to mitigate the risks associated with sleep apnea.
Importance of Seeking Treatment
Seeking treatment for sleep apnea is essential because it can save lives.
By addressing sleep apnea, we can decrease health risks and enhance our overall quality of life.
Treatment Saves Lives
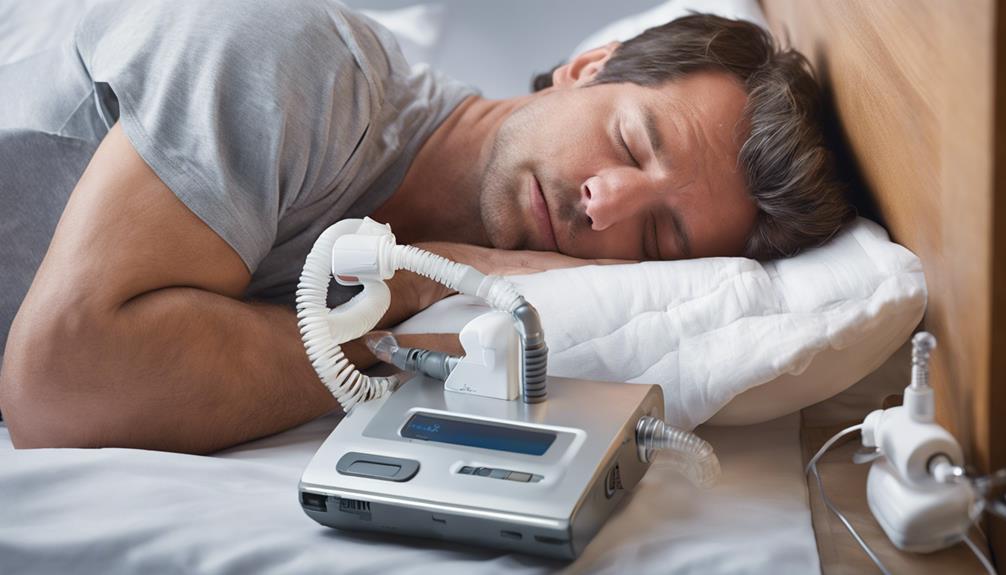
Addressing sleep apnea through effective treatment options can greatly enhance health outcomes and reduce the risk of life-threatening events. Seeking treatment for sleep apnea is vital as it can prevent serious complications and improve overall well-being. Here are five key points highlighting the importance of treatment:
- Effective treatment, such as CPAP therapy, helps prevent breathing pauses during sleep.
- Prompt medical consultation and adherence to treatments can lower mortality risk.
- Timely diagnosis and management can prevent chronic diseases associated with untreated sleep apnea.
- Treatment can reduce the risk of high blood pressure and heart problems.
- By addressing sleep apnea, individuals can improve their quality of life and safeguard against potential dangers.
Health Risks Reduced
Reducing health risks associated with sleep apnea can be achieved through timely and effective treatment interventions. Seeking medical help for symptoms like excessive daytime fatigue, loud snoring, and high blood pressure is important. Untreated sleep apnea can lead to a decrease in oxygen levels, putting stress on the heart and increasing the risk of sudden death.
CPAP therapy, a common type of treatment, helps keep the airway open during sleep, preventing breathing pauses and ensuring proper oxygen flow. By addressing sleep apnea early with appropriate medical interventions, individuals can greatly reduce the risk of complications and improve their overall health outcomes.
Quality of Life
Effective management of sleep apnea can greatly enhance quality of life by reducing daytime fatigue and improving cognitive function. Seeking treatment for sleep apnea not only addresses the immediate symptoms but also plays an important role in preventing long-term complications.
Here are five key benefits of seeking treatment for sleep apnea:
- Treatment can lower the risk of cardiovascular complications.
- It can prevent sudden death during sleep by ensuring continuous breathing.
- Managing sleep apnea can reduce accidents due to daytime sleepiness.
- Improving sleep quality through treatment enhances overall health outcomes.
- Seeking treatment can lead to increased longevity and a better quality of life in the long run.
Preventing Fatal Outcomes of Sleep Apnea
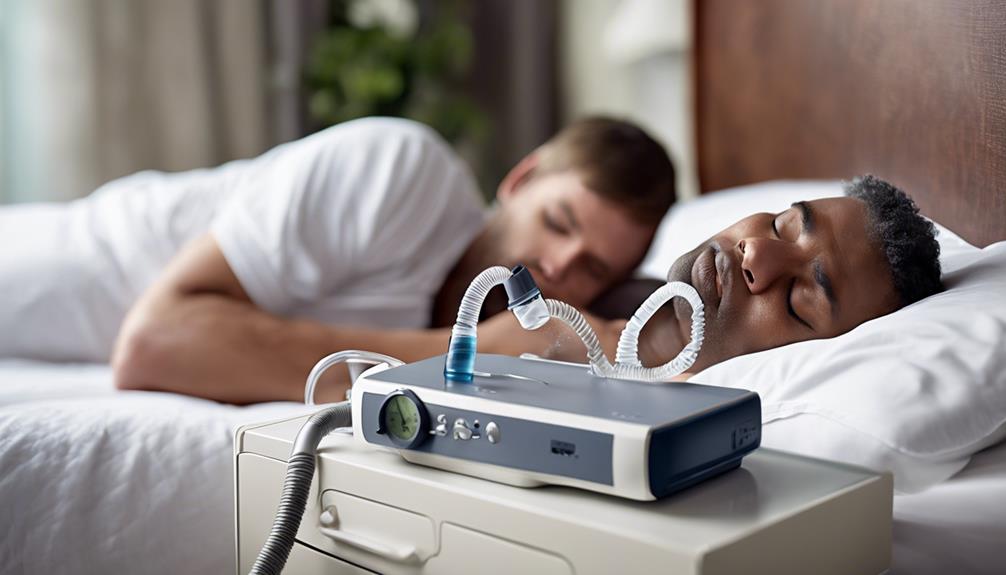
To prevent life-threatening outcomes of sleep apnea, we must prioritize early detection and timely intervention. Untreated severe obstructive sleep apnea can lead to an increased risk of sudden cardiac death, where individuals may stop breathing during sleep, resulting in dire consequences. Shared risk factors between sleep apnea and sudden death underscore the importance of seeking prompt treatment. Effective treatments for sleep apnea, such as Continuous Positive Airway Pressure (CPAP) therapy or oral appliances, can notably reduce the risk of fatal complications. Here is a table highlighting key points to emphasize the importance of timely intervention:
| Importance of Timely Intervention in Sleep Apnea |
|---|
| Early Detection |
| Prompt Treatment |
| Shared Risk Factors |
Frequently Asked Questions
What Is the Life Expectancy of a Person With Sleep Apnea?
We can improve life expectancy with sleep apnea by managing it effectively. Early diagnosis and treatment are key. Untreated severe cases can increase mortality risks, especially sudden cardiac death. Take steps to address sleep apnea for better health outcomes.
Can Sleep Apnea Cause Death While Sleeping?
Sleep apnea can cause death while sleeping due to breathing pauses. Untreated cases heighten risks, especially in older or critically ill individuals. Severe obstructive sleep apnea poses dangers. Breathing interruptions may lead to rare fatalities.
What Happens if You Don't Treat Sleep Apnea?
When untreated, sleep apnea can lead to serious health risks like heart complications and premature death. Seeking medical attention for sleep apnea can enhance our well-being, ensuring a healthier, more restful life.
Does Your Heart Stop With Sleep Apnea?
When we have sleep apnea, our heart doesn't stop, but breathing pauses can strain it. These interruptions may lead to irregular heart rhythms and increase the risk of heart issues. Proper treatment, like CPAP, can help reduce these risks.
Conclusion
So, remember kids, sleep apnea can have serious consequences if left untreated.
It may not seem like a big deal, but it can actually lead to some pretty scary stuff like heart problems and even death.
Don't take your sleep health for granted – make sure to talk to a doctor if you suspect you have sleep apnea.
It's better to be safe than sorry when it comes to something as important as your health.
Stay safe, sleep tight!