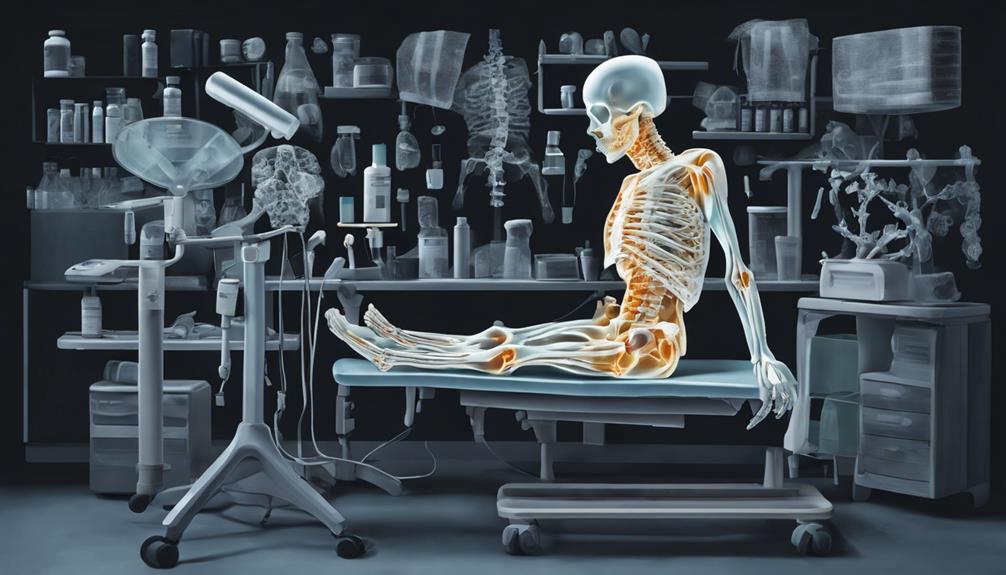
When it comes to managing osteoporosis, it is important to recognize the different medical professionals who can offer treatment. This includes endocrinologists, who specialize in metabolic disorders, and rheumatologists, who focus on arthritis, among others, all of whom contribute to the care of this condition.
But who is the primary go-to specialist for osteoporosis? Let's explore the nuances and expertise required to effectively tackle this common yet complex bone disease.
Key Takeaways
- Family doctors are initial points of contact for osteoporosis treatment.
- Specialists like endocrinologists and rheumatologists focus on osteoporosis care.
- Various doctors including gynecologists and orthopedic surgeons treat osteoporosis.
- Healthcare providers such as geriatricians specialize in managing osteoporosis.
Types of Doctors for Osteoporosis
When seeking medical help for osteoporosis, individuals may consult different types of doctors based on their specific needs and concerns. A primary care physician, such as a family doctor, often plays a crucial role in the initial evaluation and management of osteoporosis. They may conduct screenings, recommend lifestyle changes, and prescribe medications to help prevent further bone loss.
If further specialized care is needed, individuals may benefit from seeing an endocrinologist who can address hormonal imbalances contributing to osteoporosis. Endocrinologists have expertise in managing metabolic bone diseases and can provide targeted treatment options.
For more focused care on bone health, a rheumatologist can diagnose and treat various bone-related conditions, including osteoporosis. These specialists have extensive knowledge of musculoskeletal disorders and can create personalized treatment plans for managing osteoporosis effectively.
Additionally, geriatricians, with their additional training in age-related conditions, are well-equipped to address osteoporosis in older adults. For women experiencing osteoporosis related to menopause or hormonal changes, consulting a gynecologist can provide tailored care and guidance. Regular bone density scans and consultations with these healthcare professionals can help individuals maintain bone health and manage osteoporosis effectively.
Specialists in Osteoporosis Care

Specialists in osteoporosis care play a crucial role in diagnosing and treating bone-related conditions with expertise and personalized treatment plans. When seeking specialized care for osteoporosis, individuals may benefit from consulting with professionals such as:
- Endocrinologists: These specialists focus on managing hormonal imbalances related to osteoporosis and metabolic disorders, offering tailored treatment options to address these underlying issues.
- Rheumatologists: With expertise in diagnosing and treating bone, joint, and muscle conditions, including osteoporosis, rheumatologists provide comprehensive care for musculoskeletal health.
- Geriatricians: Trained in aging-related conditions, geriatricians offer personalized care for elderly patients with osteoporosis, considering factors such as age-related bone health and overall well-being.
These specialists collaborate to address the multifaceted aspects of osteoporosis, utilizing their unique skills to provide holistic care for individuals experiencing bone health concerns. By working together, they ensure that patients receive comprehensive and effective treatment plans tailored to their specific needs.
Doctors for Osteoporosis Treatment
With a focus on comprehensive care and specialized expertise, doctors for osteoporosis treatment play a vital role in diagnosing and addressing bone health concerns. Endocrinologists specialize in managing hormonal imbalances that are often related to osteoporosis and other metabolic disorders.
Rheumatologists are skilled in diagnosing and treating a variety of bone, joint, and muscle conditions, including osteoporosis and collagen diseases. Geriatricians, with additional training in aging-related conditions, are well-equipped to handle osteoporosis in older adults.
Gynecologists, who focus on female reproductive health, address osteoporosis concerns, particularly those related to menopause. Orthopedic surgeons play a crucial role in caring for musculoskeletal conditions and fractures, and they may also be involved in treating osteoporosis-related fractures.
These specialists use various diagnostic tools such as bone density scans to assess bone health and provide treatments tailored to each patient's needs, helping to manage osteoporosis and prevent fractures effectively.
Healthcare Providers for Osteoporosis

As we navigate the landscape of healthcare providers for osteoporosis, it's essential to recognize the crucial role primary care providers play as the initial point of contact for screening and managing this bone health condition. They often conduct initial assessments, including evaluating risk factors and recommending bone mineral density tests.
When searching for a doctor to address osteoporosis concerns, consider the following specialists:
- Rheumatologists: Specialize in diagnosing and treating bone, joint, and muscle disorders, including osteoporosis.
- Endocrinologists: Focus on hormonal imbalances related to osteoporosis and provide treatment recommendations.
- Geriatricians: Tailor care for the elderly population, specializing in managing osteoporosis in older adults.
These specialists complement the care provided by primary care physicians, offering expertise in specific areas such as hormonal influences on bone health and age-related bone changes. By collaborating with a multidisciplinary team, individuals can receive comprehensive care tailored to their unique needs, ensuring optimal management of osteoporosis and prevention of complications.
Osteoporosis Treatment Specialists
When seeking optimal care for osteoporosis, individuals may benefit from consulting with experienced healthcare professionals specializing in the treatment of this bone health condition.
Rheumatologists are experts in diagnosing and treating bone, joint, and muscle disorders, including osteoporosis.
Endocrinologists focus on correcting hormonal imbalances related to osteoporosis and managing overall bone health.
Geriatricians specialize in tailoring care for senior patients, particularly in managing osteoporosis in older adults.
Gynecologists address osteoporosis concerns in women, especially those related to menopause and female reproductive health.
Primary care providers play a crucial role in screening for osteoporosis, prescribing treatments, and offering referrals to specialists for further management.
These specialists work together to ensure comprehensive care for patients, considering factors such as bone density, hormonal imbalances, and the unique needs of geriatric and female patients.
Consulting with a team of specialists can help individuals receive personalized osteoporosis treatment tailored to their specific health needs.
Frequently Asked Questions
What Is the Best Doctor to See for Osteoporosis?
When looking for the best doctor to see for osteoporosis, it's crucial to consider specialists like endocrinologists, rheumatologists, family doctors, geriatricians, and gynecologists, each bringing unique expertise to the table. These healthcare professionals can provide comprehensive care tailored to your specific needs, ensuring you receive the best treatment and management for osteoporosis.
It's important to consult with a doctor who understands your condition and can guide you towards optimal health.
What Will an Endocrinologist Do for Osteoporosis?
When tackling osteoporosis, an endocrinologist plays a vital role in evaluating hormonal imbalances that impact bone density. They may recommend hormone replacement therapy or medications to address these issues.
How Does a Rheumatologist Treat Osteoporosis?
When treating osteoporosis, we rheumatologists focus on:
- Diagnosing bone issues
- Evaluating fracture risk
- Creating personalized treatment plans
Medications like bisphosphonates, hormone therapy, or denosumab are often prescribed to:
- Reduce bone loss
- Prevent fractures
Monitoring bone density through regular tests and collaborating with other healthcare providers for multidisciplinary care are vital aspects of our approach.
We aim for comprehensive osteoporosis management to ensure the best outcomes for our patients.
What Is the Best and Safest Treatment for Osteoporosis?
We can assure you that the best and safest treatment for osteoporosis involves a combination of medications, supplements, lifestyle changes, and preventive measures. These multifaceted approaches help slow bone loss, reduce fracture risks, and improve overall bone health.
Working closely with healthcare providers like primary care doctors, rheumatologists, endocrinologists, and physical therapists ensures a comprehensive and tailored treatment plan. Embracing these strategies empowers individuals to manage osteoporosis effectively and enhance their quality of life.
Conclusion
In conclusion, when it comes to treating osteoporosis, various medical specialists are available to provide expert care tailored to individual needs.
While some may feel overwhelmed by the idea of navigating through multiple healthcare providers, remember that this team approach ensures comprehensive and personalized treatment.
Trust in the expertise of these doctors and healthcare professionals to guide you towards better bone health and overall well-being.
You aren't alone in this journey towards stronger bones and a healthier future.