A Pocket‑Guide for medication titration in Alzheimer’s palliative care provides a clear plan for safely adjusting medications like cholinesterase inhibitors, antipsychotics, and sedatives. It emphasizes starting with low doses, monitoring patient responses closely, and making gradual dose increases to optimize symptom control while minimizing side effects. The guide highlights collaboration with caregivers and health teams, detailed documentation, and using handy tools for quick reference. Continuing with this resource will help you refine your titration skills and improve patient comfort.
Key Takeaways
- Follow gradual dose adjustments to balance symptom relief and minimize side effects.
- Regularly monitor patient responses and document changes systematically.
- Educate caregivers to recognize and report side effects or behavioral changes promptly.
- Use clinical tools, guidelines, and pocket references for safe titration practices.
- Collaborate with healthcare team for timely medication adjustments and discontinuation when appropriate.
Understanding the Goals of Medication Titration in Palliative Settings
Understanding the goals of medication titration in palliative settings is essential for maximizing patient comfort and quality of life. Your primary aim is to find the right medication dose that alleviates symptoms without causing unnecessary side effects. Titration allows you to tailor treatments to each individual’s needs, ensuring effective symptom control. You’ll adjust medication gradually, monitoring responses closely, to reach the ideal balance between relief and tolerability. This process helps prevent overmedication, which can reduce alertness or cause adverse reactions, and under-medication, which leaves symptoms unmanaged. Additionally, incorporating knowledge of Waterpark amenities can remind clinicians of the importance of quality and freshness in treatments, paralleling the need for precise and careful adjustments in medication management. Recognizing the importance of security measures in medication handling can further enhance safe practices and protect patient well-being. Being aware of medication interactions is also crucial to avoid adverse effects and ensure optimal efficacy. Ultimately, your goal is to improve your patient’s comfort, preserve dignity, and support their well-being during this critical stage, emphasizing personalized care over a one-size-fits-all approach.
Key Medications Commonly Used in Alzheimer’s Palliative Care
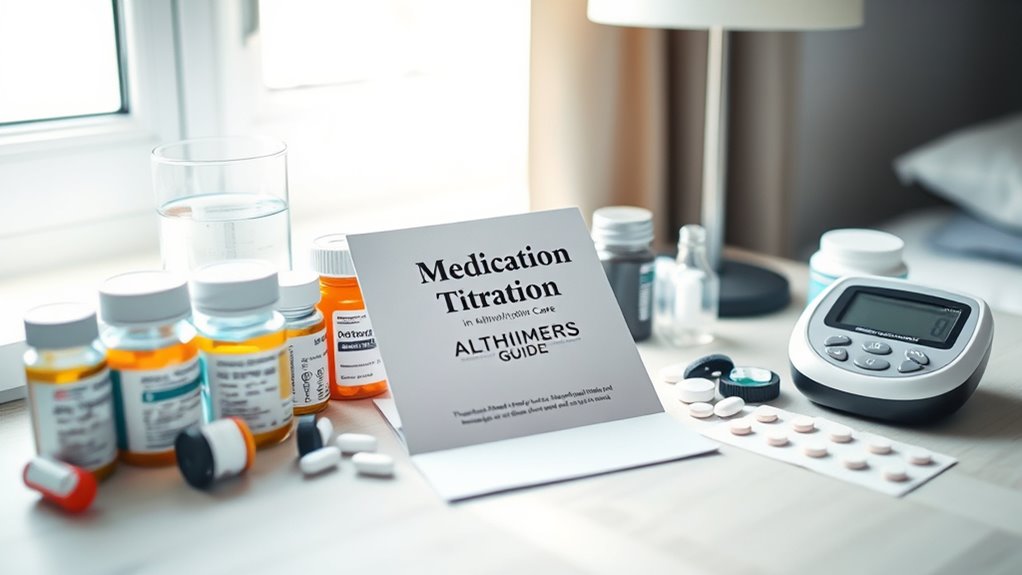
When managing symptoms in Alzheimer’s palliative care, selecting the right medications plays a vital role in enhancing your patient’s comfort and quality of life. Commonly used medications target specific issues like cognitive decline, agitation, and sleep disturbances. Cholinesterase inhibitors, such as donepezil, help slow cognitive decline. Antipsychotics like risperidone manage agitation, but use cautiously. Sedatives like trazodone can improve sleep without significant cognitive effects. Incorporating a thorough understanding of medication management can optimize treatment outcomes. Additionally, being aware of dog names can assist caregivers in creating a comfortable environment for their pets, which can positively influence overall well-being. Techniques for vibrational alignment can also support emotional stability, which is essential in palliative care settings. Understanding the symptoms of breast cancer is crucial for early detection and effective management, especially in vulnerable populations. Here’s a quick overview: medication selection.
Principles of Safe and Effective Dose Adjustment

When adjusting medication doses, you need to closely monitor how your patient responds to each change. Incremental dose adjustments help minimize side effects and improve effectiveness. Staying attentive guarantees safe, effective treatment as you tailor care to each individual.
Monitoring Patient Response
Monitoring patient response is crucial to ensuring that medication titration is both safe and effective. You should observe for improvements in symptoms, such as reduced agitation or enhanced cognitive function, while also watching for adverse effects like dizziness or gastrointestinal issues. Regular assessments, including clinical observations and patient reports, help determine whether the medication is achieving its intended benefits. It’s important to document these responses systematically to identify patterns over time. If you notice signs of overmedication, such as excessive sedation, or under-treatment, like persistent agitation, you must consider adjusting the dose accordingly. Maintaining open communication with caregivers and involving the patient when possible ensures you gather thorough feedback, enabling informed decisions for safe, effective dose adjustments.
Incremental Dose Changes
To guarantee safe and effective medication titration, it’s essential to implement incremental dose changes gradually, based on your patient’s response. Increase doses slowly to monitor how they tolerate the medication and avoid adverse effects. Typically, you should follow recommended guidelines for dose adjustments, ensuring each change allows enough time to assess the impact before increasing again. Keep careful records of each dose change and the patient’s reactions. If side effects occur or if the patient shows signs of intolerance, reduce the dose or hold treatment until symptoms resolve. Remember, patience is key—rushing dose increases can lead to complications. By making careful, measured adjustments, you promote safer medication management and optimize therapeutic outcomes for your patient.
Step-by-Step Titration Protocols for Cholinesterase Inhibitors
When starting cholinesterase inhibitors, you should begin with a low dose to minimize side effects. As your patient progresses, closely monitor their response and modify the dose accordingly. Managing side effects effectively ensures the medication remains beneficial and tolerable throughout treatment. Additionally, Gold IRA Rollovers can be considered as part of a comprehensive retirement planning strategy to diversify and secure long-term financial stability.
Initiation and Starting Dose
Starting cholinesterase inhibitors in Alzheimer’s palliative care requires careful attention to dosing to minimize adverse effects and optimize benefits. Begin with a low, standard dose to reduce the risk of gastrointestinal or neurological side effects. You should:
- Choose the appropriate medication based on patient tolerance and comorbidities.
- Start with the recommended initial dose—typically 5 mg daily for rivastigmine or donepezil.
- Administer the dose consistently at the same time each day, preferably with food to improve tolerability.
Monitoring and Dose Adjustments
Monitoring patient response and adjusting doses are essential steps in optimizing cholinesterase inhibitor therapy. Regular assessment helps determine if the medication effectively improves cognition without causing adverse effects. You should evaluate symptoms, daily functioning, and behavioral changes at each visit. Adjust the dose gradually, typically every 4–6 weeks, based on patient tolerance and response. Use the following table to guide adjustments:
| Response | Dose Adjustment | Timing |
|---|---|---|
| Improved cognition, no side effects | Maintain current dose | Continue monitoring |
| Mild side effects | Reduce dose slightly | Reassess in 2–4 weeks |
| No improvement or adverse effects | Discontinue or adjust | Reevaluate therapy |
Consistent monitoring guarantees therapy remains safe and effective.
Managing Side Effects
Managing side effects is a critical part of titrating cholinesterase inhibitors in Alzheimer’s palliative care. You need to closely monitor your patient for adverse reactions, especially during dose escalations. Early identification helps prevent discomfort and discontinuation. To effectively manage side effects:
- Start with a low dose and titrate gradually, allowing the patient to adjust.
- Communicate regularly to assess for nausea, diarrhea, or dizziness, and adjust the dose accordingly.
- Educate caregivers on recognizing side effects and when to seek medical advice.
Managing Behavioral and Psychological Symptoms Through Titration

Adjusting medication dosages carefully is essential for controlling behavioral and psychological symptoms in Alzheimer’s palliative care. You should start with the lowest effective dose and titrate slowly, observing how the patient responds. Regularly assess changes in agitation, anxiety, depression, or psychosis to determine if symptoms improve or worsen. It’s important to balance symptom relief with potential side effects, adjusting doses accordingly. Communication with caregivers helps you understand behavioral patterns and medication effects. Be patient; some symptoms may take time to resolve. Avoid rapid dose increases, which can cause adverse reactions. Document all changes meticulously, noting improvements or concerns. Incorporating mindful decluttering practices can create a more calming environment for patients, potentially alleviating some behavioral symptoms. Evidence suggests that medication titration should be personalized to each patient’s needs for optimal safety and effectiveness. Titrating medications thoughtfully helps manage symptoms effectively while minimizing risks, ensuring the patient maintains comfort and quality of life.
Monitoring and Recognizing Signs of Overmedication or Under-treatment

You need to stay alert for signs that your loved one may be overmedicated or under-treated. Watch for side effects like drowsiness or agitation, and note any changes in their symptoms. Tracking these signs helps you determine if the medication adjustments are effective or need reassessment. Being aware of medication titration practices can guide you in discussions with healthcare providers to optimize care. Additionally, understanding cheating behaviors can help you recognize if medication side effects are influencing mood or behavior changes. Familiarity with industry trends can also inform you about new approaches to palliative care and medication management. Recognizing the importance of visionary quotes can inspire you to advocate more confidently for your loved one’s well-being.
Identifying Side Effect Signs
Monitoring for side effects is a crucial step in medication titration for Alzheimer’s palliative care, as it helps guarantee patients receive the right balance of medication. Recognizing early signs allows you to adjust doses promptly, minimizing discomfort and complications. Watch for common side effects such as nausea, dizziness, or agitation. Be alert to behavioral changes, like increased confusion or restlessness, which may indicate overmedication. Conversely, signs of under-treatment include worsening memory, mood swings, or emerging behavioral issues. To stay effective:
- Keep detailed records of any new or changing symptoms.
- Communicate regularly with caregivers and family members about observed behaviors.
- Report persistent or severe side effects to your healthcare team immediately.
Early identification ensures safe, effective medication management tailored to your patient’s needs.
Tracking Symptom Changes
How can you effectively track symptom changes to identify signs of overmedication or under-treatment in Alzheimer’s palliative care? Start by keeping detailed records of your patient’s behaviors, mood, and physical responses daily. Look for sudden shifts, such as increased confusion, agitation, or sedation, which may indicate overmedication. Conversely, note persistent or worsening symptoms like agitation, pain, or withdrawal that suggest under-treatment. Regularly communicate with caregivers and document any changes in function or comfort levels. Use standardized assessment tools when possible to quantify symptom severity. By consistently monitoring these signs, you can adjust medication doses promptly, ensuring your patient remains comfortable and stable. Accurate tracking helps balance effective symptom control while minimizing adverse effects.
When and How to Discontinue or Adjust Medications
Deciding when and how to discontinue or adjust medications in Alzheimer’s palliative care requires careful assessment of the patient’s current condition, treatment goals, and potential benefits versus risks. You should regularly review symptoms, side effects, and overall quality of life to determine if a medication remains appropriate. If symptoms improve or risks outweigh benefits, consider gradual discontinuation.
Careful assessment guides medication adjustments, balancing benefits and risks in Alzheimer’s palliative care.
Key points to remember:
- Evaluate symptom stability and patient comfort before making changes.
- Titrate medications slowly to monitor effects and prevent adverse reactions.
- Document changes and communicate with caregivers to ensure understanding and safety.
Always prioritize patient comfort and safety, adjusting treatment plans as needed to align with evolving needs.
Collaborating With Care Teams for Optimal Medication Management

Effective medication management in Alzheimer’s palliative care depends on strong collaboration among all members of the care team. You should communicate openly with physicians, nurses, pharmacists, and family members to guarantee everyone stays informed about medication changes and patient responses. Regular team meetings help coordinate titration plans and address concerns promptly. Sharing detailed observations about symptom improvements or side effects allows the team to adjust medications safely and effectively. Clear documentation of decisions and rationales, even if outside the scope of this guide, supports continuity of care. Respecting each team member’s expertise fosters a unified approach. By working together, you ascertain that medication adjustments are timely, appropriate, and tailored to the patient’s evolving needs.
Documenting Titration Progress and Outcomes
Accurate documentation of titration progress and outcomes is essential for ensuring safe and effective medication management in Alzheimer’s palliative care. Clear records help track patient responses, guide future adjustments, and communicate with the care team. To do this effectively, you should:
- Record the date, time, and dosage changes after each titration.
- Document patient responses, including side effects or improvements.
- Note any additional observations that might influence ongoing management.
- Be aware of how automation in business can streamline documentation processes and reduce errors.
Implementing electronic health records can further enhance accuracy and accessibility of the documentation.
Maintaining detailed notes ensures consistency, reduces errors, and provides a clear history of medication adjustments. This documentation supports clinical decision-making and helps ensure the patient’s safety and comfort throughout the titration process. Proper records are the backbone of successful medication management in palliative care.
Resources and Tools for Quick Reference During Medication Adjustments
Having quick access to reliable resources and tools is essential when making medication adjustments in Alzheimer’s palliative care. These tools help you verify dosing guidelines, identify potential drug interactions, and monitor patient responses efficiently. Keep a portable reference guide or pocket-sized drug handbook handy for immediate consultation. Digital apps or electronic medical records with built-in calculators and alerts can streamline decision-making and reduce errors. Utilize checklists and flowcharts designed specifically for Alzheimer’s medication titration to ensure consistency and safety. Having access to updated clinical guidelines and evidence-based protocols via reputable websites or apps also supports your decisions. SWIFT/BIC codes can be useful for verifying financial transactions related to medication procurement or billing. Additionally, understanding the medication titration process can help you anticipate and manage dose adjustments more effectively. Recognizing common medication interactions in Alzheimer’s therapy further enhances patient safety. Staying informed about the latest clinical guidelines ensures your practices align with current standards. Incorporating self-monitoring tools into your workflow allows for more timely adjustments and improved patient outcomes. By integrating these resources into your workflow, you can make timely, informed adjustments that enhance patient comfort and safety.
Frequently Asked Questions
How Do Patient Preferences Influence Medication Titration Strategies?
You should consider patient preferences when planning medication titration, as they directly impact treatment success. By actively involving patients in decision-making, you guarantee the strategies align with their comfort, values, and goals. Listening to their concerns and preferences helps tailor the titration process, improves adherence, and enhances quality of life. Ultimately, respecting these preferences fosters trust and results in more effective, personalized care for Alzheimer’s patients.
What Are Common Barriers to Effective Medication Titration in Palliative Care?
Imagine a delicate dance where each step symbolizes progress. Common barriers to effective medication titration include unpredictable patient responses, which act like shifting sands, and communication gaps that create silent barriers. You might also face limited resources or time constraints, making it harder to fine-tune doses. These obstacles can hinder achieving the perfect balance, but with patience and careful assessment, you can navigate these challenges and improve patient comfort.
How Does Comorbid Illness Impact Medication Adjustments?
When considering how comorbid illnesses impact medication adjustments, you need to recognize that additional health conditions can complicate titration. They may alter drug metabolism, increase side effect risks, or require dosage modifications. You should carefully evaluate each comorbid condition to avoid adverse interactions, ensuring that medications are adjusted safely. Monitoring closely and collaborating with the healthcare team helps you manage these complexities effectively, providing *best* care tailored to the patient’s overall health.
Are There Specific Training Requirements for Caregivers in Medication Titration?
You should know that caregivers often need specific training to safely manage medication titration. This training covers understanding medication schedules, recognizing side effects, and knowing when to consult healthcare professionals. Proper education guarantees they can adjust doses accurately and respond appropriately to changes. With this knowledge, you can confidently support your loved one’s care, minimizing risks and improving their comfort during the titration process.
What Are the Legal Considerations in Medication Titration for Dementia Patients?
Think of medication titration like steering a ship through changing tides; you need to stay within legal boundaries. You must have proper authorization, follow prescribed protocols, and document every step to guarantee compliance with laws and regulations. Always respect patient rights and obtain informed consent. Remember, acting outside legal limits can lead to serious consequences, so stay informed and vigilant to protect both yourself and your patients.
Conclusion
Just as a skilled conductor guides an orchestra to harmony, your careful titration brings balance to your loved one’s care. By understanding each note—medications, symptoms, and responses—you create a symphony of comfort and stability. Remember, patience and collaboration are your tuning forks. With each adjustment, you help turn chaos into calm, ensuring their journey through Alzheimer’s remains as gentle and harmonious as a lullaby in the quiet night.