Let’s delve into the intricate realm of hallucinations, much like traversing a maze where every twist and turn reveals a new facet of the mind’s complexities.
Visual, auditory, olfactory, tactile, and gustatory—these five types of hallucinations offer a kaleidoscope of experiences that can profoundly impact an individual's perception of reality.
But what sets them apart, and how do they manifest in the intricate tapestry of human consciousness?
Let's unravel these enigmatic threads together to shed light on the diverse ways in which our minds can both deceive and illuminate our understanding of the world around us.
Key Takeaways
- Visual, auditory, olfactory, tactile, and gustatory hallucinations are the five types of hallucinations.
- Hallucinations can be associated with various conditions such as Parkinson's disease, schizophrenia, and dementia.
- Seeking professional help is crucial for managing and understanding coping strategies for hallucinations.
- Treatment may involve therapy, medication, and addressing underlying causes for effective management.
Visual Hallucinations
Visual hallucinations are perceptions that occur without any external stimuli, often involving seeing things that aren't actually present. These types of hallucinations can vary greatly, from simple shapes or colors to detailed scenes or people. They're commonly associated with conditions affecting the central nervous system, such as Parkinson's disease, schizophrenia, or epilepsy. The brain's processing of sensory information is altered, leading to these vivid sensory experiences.
Individuals experiencing visual hallucinations may also encounter auditory, tactile, or olfactory hallucinations. These hallucinations can be distressing and may indicate an underlying mental health condition. Seeking professional help and understanding coping strategies is crucial for managing visual hallucinations effectively. Treatments such as transcranial magnetic stimulation or medication may be recommended based on the individual's specific situation.
Developing a support network and practicing self-care techniques can also aid in navigating the challenges presented by visual hallucinations. It's essential to approach these experiences with empathy and a willingness to assist those affected.
Auditory Hallucinations

In the realm of sensory perceptions, auditory hallucinations manifest as the experience of hearing sounds or voices that lack external sources.
Auditory hallucinations are prevalent in mental health conditions, with schizophrenia being one of the most common disorders associated with this type of hallucination.
Here are four key points to consider regarding auditory hallucinations:
- Auditory hallucinations can present as complimentary, critical, or neutral voices, influencing individuals' emotions and behaviors.
- Besides schizophrenia, auditory hallucinations may also occur in conditions such as bipolar disorder, dementia, and during periods of bereavement, highlighting the diverse contexts in which they can arise.
- Treatment for auditory hallucinations often involves a combination of therapy, medication, and lifestyle changes to manage symptoms and improve the individual's quality of life.
- Understanding the nature of auditory hallucinations is crucial in addressing the complexities of mental illness and providing appropriate support and intervention for those experiencing these challenging symptoms.
Olfactory Hallucinations
Moving from the realm of auditory hallucinations, our focus now shifts to olfactory hallucinations, which involve the perception of smells or odors that aren't actually present. Olfactory hallucinations are one of the five types of hallucinations that can affect individuals. These hallucinations can be a result of various conditions affecting the brain or body.
The sense of smell is processed in the olfactory bulb in the brain, making it susceptible to distortions that lead to olfactory hallucinations. These hallucinations can be caused by neurological conditions such as Alzheimer's disease, where changes in the brain impact the perception of smells. Other potential causes include infections, nasal polyps, or exposure to certain chemicals.
Experiencing olfactory hallucinations can be disorienting and distressing for individuals. Understanding the underlying cause is crucial in managing these hallucinations effectively. If you or someone you know is experiencing persistent olfactory hallucinations, seeking medical advice is essential to address any underlying conditions and ensure proper care for the senses.
Tactile Hallucinations

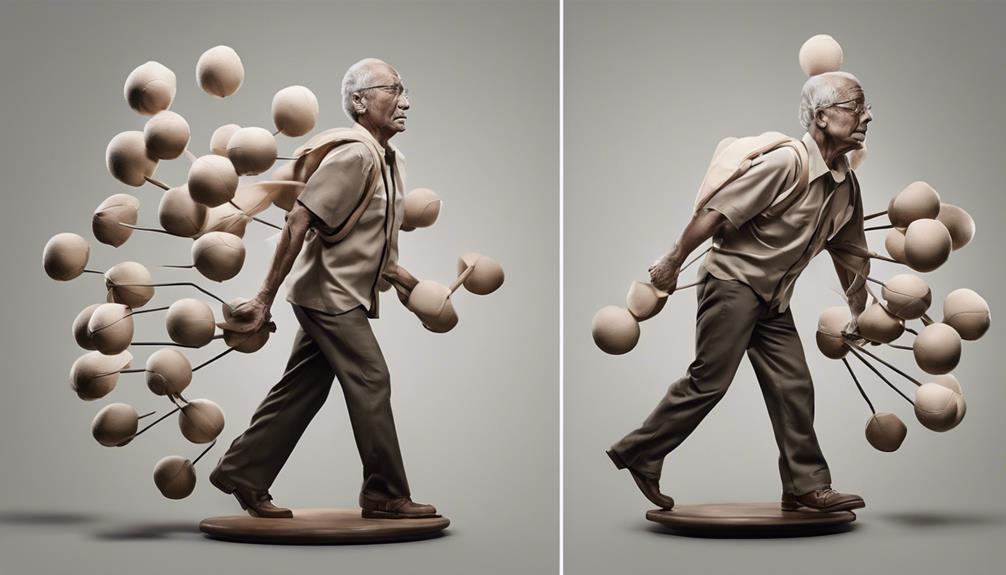
Tactile hallucinations involve sensations of touch or movement in the body that aren't based on reality, often including perceptions like bugs crawling on the skin or internal organs shifting within.
Tactile hallucinations are commonly associated with substance abuse, such as cocaine or amphetamine.
They can also occur in certain neurological conditions or during withdrawal from drugs.
These hallucinations can be distressing and may lead to self-harm or other dangerous behaviors.
Treatment for tactile hallucinations may involve addressing the underlying cause, such as substance abuse or a neurological condition, and may include therapy or medication.
Tactile hallucinations can occur during wakefulness or sleep, affecting the individual's perception of reality.
It's crucial to seek professional help if experiencing such sensations to prevent harm and address any underlying issues effectively.
Understanding the potential triggers and seeking appropriate treatment can help manage and alleviate the distress caused by tactile hallucinations.
Gustatory Hallucinations
Gustatory hallucinations, though less common than auditory or visual hallucinations, involve experiencing tastes that are not actually present. These hallucinations can be unsettling as they distort the sense of taste, often resulting in strange or unpleasant flavors being perceived. They can be triggered by various factors such as neurological damage, viruses, trauma, brain tumors, toxic substances, drugs, or epilepsy.
| Types of Hallucinations | Prevalence | Associated Conditions |
|---|---|---|
| Visual | Common | Schizophrenia |
| Auditory | Common | Alzheimer's Disease |
| Olfactory | Less Common | Lewy Body Dementia |
| Gustatory | Rare | Charles Bonnet Syndrome |
While gustatory hallucinations are rarer, they are important to recognize, as they can be indicative of underlying health issues. Understanding the potential causes and associated conditions can aid in diagnosing and addressing the root problem. Treatment for gustatory hallucinations varies depending on the underlying cause and may involve a combination of medication and therapy.
Frequently Asked Questions
What Are 2 Common Hallucinations?
When talking about common hallucinations, two prevalent types are visual and auditory.
Visual hallucinations involve seeing things that aren't actually there, while auditory hallucinations entail hearing sounds or voices that aren't real.
These two categories are frequently reported and can significantly impact individuals' daily lives.
Understanding these common hallucinations is crucial in providing appropriate support and care for those experiencing them.
What Are the 7 Types of Hallucination?
We discussed the 5 types of hallucinations earlier, but the current question asks about 7 types.
While researching, we discovered that auditory and visual hallucinations are the most common types experienced. It's fascinating how our senses can deceive us in various ways.
Exploring the lesser-known types may shed light on unique experiences people have. These insights can help us understand and support those dealing with diverse forms of hallucinations.
What Are the Most Common Visual Hallucinations?
Visual hallucinations can manifest in various forms, from simple shapes to complex scenes and figures. They're one of the most common types of hallucinations experienced. These visions may involve seeing people, animals, objects, or patterns that aren't actually present.
Factors like stress, sleep disturbances, and certain medical conditions can contribute to the occurrence of visual hallucinations. Seeking medical advice is crucial for proper evaluation and management.
How Can You Tell if Someone Is Hallucinating?
Well, spotting hallucinations isn't exactly like finding Waldo.
We may notice unusual behavior or responses, like talking to imaginary friends or reacting to unseen stimuli, as signs of someone hallucinating.
Changes in mood, confusion, or intense fear can also be indicators.
Conclusion
In conclusion, understanding the different types of hallucinations can provide valuable insight into the complex nature of schizophrenia. Just as each individual experiences hallucinations differently, the treatment and management of this condition must be tailored to address specific symptoms.
By recognizing and addressing hallucinations early on, individuals can receive the necessary support and care to improve their quality of life. As the saying goes, knowledge is power when it comes to navigating the complexities of mental health.