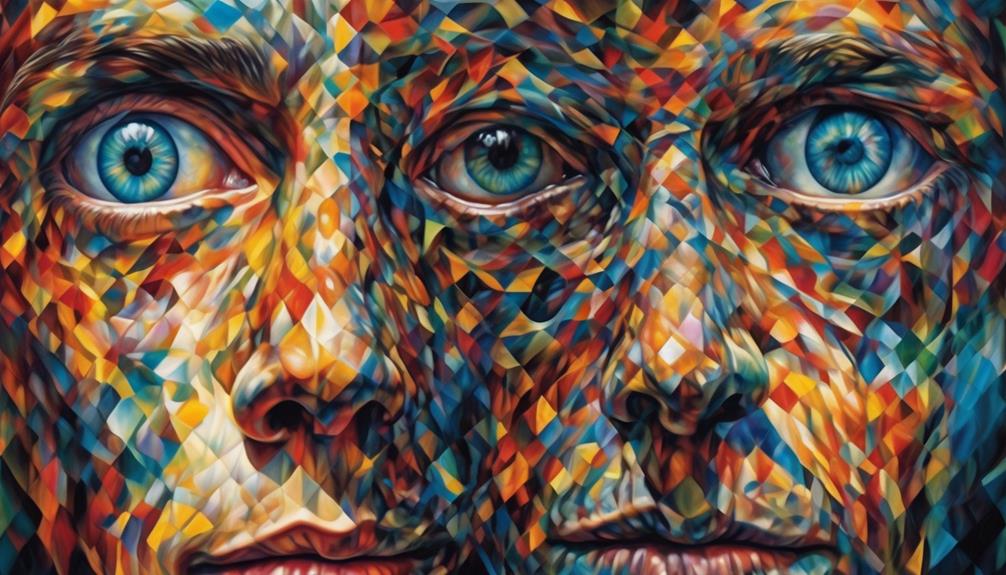
Have you ever doubted the realness of the images you see during hallucinations with your eyes wide open?
These phenomena, often associated with various conditions and experiences, can be perplexing at first glance. From sleep deprivation to neurological conditions, the causes of these visual distortions vary widely.
However, understanding the underlying mechanisms behind these hallucinations can shed light on the complexity of the human mind and perception.
Key Takeaways
- Sleep deprivation disrupts brain functioning and can lead to open eye hallucinations.
- Drug use, especially in individuals with mental health issues, can cause hallucinations.
- Migraine auras can result in temporary visual disturbances and may require medical consultation.
- Schizophrenia is a chronic mental disorder characterized by hallucinations and delusions.
Sleep Deprivation
Sleep deprivation disrupts normal brain functioning, leading to open eye hallucinations. When we don't get enough sleep, the brain's ability to process information and regulate emotions is compromised. This can result in visual hallucinations, where we see things that aren't actually there. These hallucinations happen because the brain is overactive and starts generating images that aren't based on real stimuli. It's important to recognize that open eye hallucinations due to sleep deprivation are typically brief and transient, disappearing once we catch up on rest.
Addressing sleep deprivation is crucial as it can be a root cause of visual hallucinations. By improving our sleep hygiene and ensuring we get an adequate amount of sleep, we can help prevent these disruptions in brain function. Various factors, such as insomnia, sleep apnea, or lifestyle choices, can contribute to sleep deprivation. Recognizing the impact of sleep on our mental health is essential in promoting overall well-being and preventing potential long-term consequences of chronic sleep deprivation.
Drug Use

In the realm of substance consumption that alters mental states, drug use encompasses various substances like alcohol, tobacco, prescription drugs, and illicit drugs. Drug use refers to the consumption of substances that can alter brain function and behavior.
When it comes to visual hallucinations caused by drug use, it's essential to understand how the brain gets affected by these substances. Here are some key points to consider:
- Different drugs can trigger visual hallucinations by influencing neurotransmitter levels in the brain.
- The misuse of certain substances can exacerbate underlying mental illness, potentially leading to hallucinations.
- Drug-induced hallucinations may vary in intensity and duration depending on the type and amount of substance consumed.
- Individuals with a history of mental health issues may be more susceptible to experiencing visual disturbances from drug use.
- Seeking professional help is crucial for addressing both the substance abuse problem and any resulting mental health concerns.
Migraine Auras
When considering the impact of drug use on visual hallucinations, it's essential to shift focus to the realm of migraine auras, which are characterized by visual disturbances preceding or accompanying migraine headaches.
Migraine auras present as temporary, but often unsettling, visual phenomena such as flashing lights, zigzag lines, or blind spots in the field of vision. These hallucinations are believed to stem from alterations in brain activity and blood flow patterns.
While migraine auras are typically harmless and resolve on their own, they can sometimes be indicative of underlying health issues. Notably, individuals experiencing frequent or severe migraine auras may find solace in consulting a healthcare provider to explore management strategies.
It's important to distinguish migraine auras from other forms of visual hallucinations, such as those seen in Charles Bonnet Syndrome (CBS), which are unrelated to migraines and stem from visual pathway issues rather than brain activity changes.
Understanding the distinct nature of migraine auras can aid in appropriate diagnosis and management strategies for individuals experiencing these visual disturbances.
Schizophrenia
Schizophrenia, a chronic mental disorder, manifests through symptoms such as hallucinations, delusions, disorganized thinking, and abnormal behaviors. When considering hallucinations in the context of eye conditions and vision loss, it's crucial to differentiate between conditions like Charles Bonnet Syndrome and schizophrenia.
Here are some key points regarding schizophrenia and its relation to visual hallucinations in individuals with vision loss:
- Individuals with schizophrenia may experience visual hallucinations that are unrelated to eye conditions or vision loss.
- Schizophrenia is primarily characterized by disturbances in thought processes, perception, and emotional responsiveness.
- While Charles Bonnet Syndrome is linked to eye conditions and vision loss, schizophrenia isn't solely attributed to these factors.
- Treatment for schizophrenia typically involves a multidisciplinary approach, including medications, therapy, and support networks.
- It's important to seek professional help and guidance for individuals experiencing hallucinations, especially when associated with conditions like schizophrenia.
Neurological Conditions
Considering the intricate interplay between mental health and neurological function, our focus now shifts to exploring the realm of Neurological Conditions, encompassing disorders affecting the brain, spinal cord, and nerves.
Within this domain, a notable condition that sheds light on open eye hallucinations is Charles Bonnet Syndrome (CBS). CBS is often seen in individuals with visual impairments such as macular degeneration, highlighting the intricate relationship between the visual system and neurological processes.
The hallucinations experienced in CBS aren't psychiatric in nature but rather stem from neurological mechanisms due to sensory deprivation. Understanding the visual system's role in CBS can aid in developing targeted interventions to alleviate hallucinations and improve quality of life for affected individuals.
Research into the underlying mechanisms of CBS is ongoing, emphasizing the need for further exploration in the field of neurology to enhance our comprehension of how neurological conditions manifest and impact individuals. This knowledge can guide healthcare providers in offering tailored support and treatments to those navigating neurological challenges.
Frequently Asked Questions
What Triggers Visual Hallucinations?
When talking about visual hallucinations, it's crucial to delve into what triggers these experiences. Various factors, such as medical conditions, medications, or neurological changes, can lead to the manifestation of visual hallucinations.
Understanding these triggers is essential in effectively managing and treating individuals experiencing such phenomena. By identifying the root causes, healthcare providers can tailor interventions to address the underlying issues and support those affected.
What Are Open Eye Hallucinations?
We see visions that dance before our eyes, beckoning from the shadows of perception. Open eye hallucinations, intricate illusions born from a quiet mind's whisper.
These visual mirages, though vivid and captivating, are mere phantoms of reality. They come and go like fleeting dreams, leaving no lasting trace.
In our quest to understand the mind's mysteries, we ponder the enigma of open eye hallucinations, seeking to unravel their elusive nature.
How Do You Get Rid of Eye Hallucinations?
To get rid of eye hallucinations, we may suggest strategies like moving the eyes or altering environmental factors to help dissipate the hallucinations. Treating the underlying eye condition can also be beneficial in reducing hallucinations for some individuals.
Additionally, support groups, counseling, and new treatments such as transcranial direct current stimulation may offer relief. Regular eye examinations, monitoring, and using low vision aids are vital for managing and mitigating eye hallucinations.
What Eye Problems Cause Hallucinations?
Eye problems that can cause hallucinations include Charles Bonnet Syndrome and macular degeneration. These conditions lead to visual hallucinations due to the brain cells firing spontaneously.
While medication and rehabilitation can help manage symptoms, education, distraction techniques, and emotional support play crucial roles in coping.
Understanding the causes of these hallucinations is essential for effective treatment and support for individuals experiencing them.
Conclusion
In conclusion, the intricate web of factors contributing to open eye hallucinations resembles a complex puzzle waiting to be solved.
Just as each piece fits together to create a cohesive picture, understanding the underlying causes of these hallucinations requires a systematic and methodical approach.
By unraveling the mysteries behind these phenomena, we can shed light on the enigmatic world of perception and pave the way for innovative treatments and interventions.









