If you notice acting out vivid or violent dreams, shouting, or sudden movements during sleep, it could be REM Sleep Behavior Disorder, which may signal underlying Parkinson’s disease. These episodes often happen in the later part of the night and can cause injuries. Recognizing these signs early is important, as they often precede motor symptoms. Keep exploring to understand how sleep issues connect to Parkinson’s and what steps you can take next.
Key Takeaways
- Acting out vivid dreams with physical movements and vocalizations can signal REM Sleep Behavior Disorder (RBD), an early Parkinson’s warning.
- RBD episodes often occur in the later sleep cycles and may lead to injury or sleep disruption.
- Early signs of Parkinson’s may include sleep disturbances like RBD before motor symptoms appear.
- Safe sleep environments and medical consultation are essential if violent movements or injuries occur during sleep.
- Noticing changes in sleep behavior should prompt prompt medical evaluation for early diagnosis and management.
Understanding REM Sleep Behavior Disorder and Its Symptoms

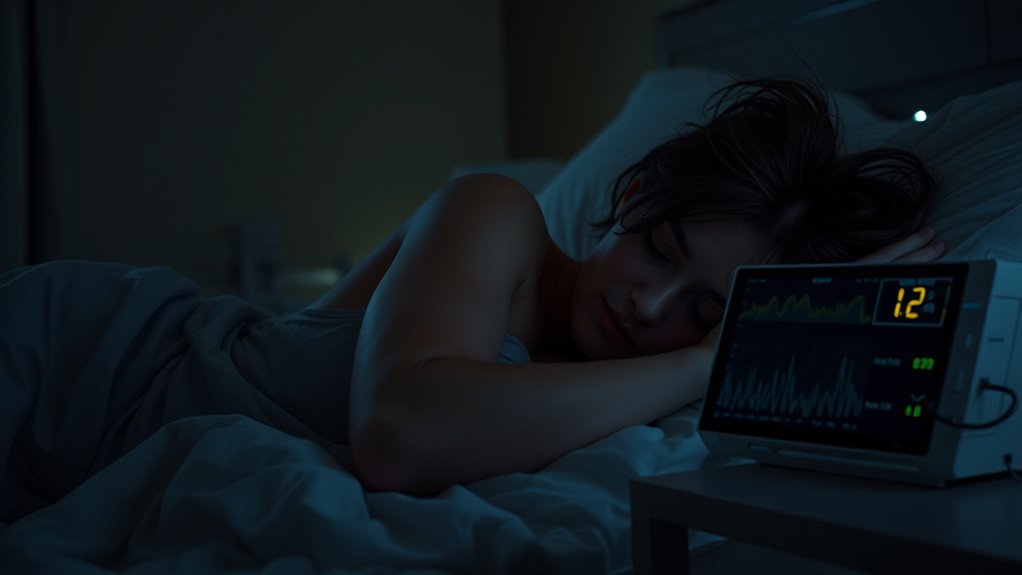
REM Sleep Behavior Disorder (RBD) is a condition where your muscles don’t stay in the usual relaxed state during REM sleep, causing you to act out your dreams. Instead of remaining still, you might move, talk, or even hit or kick while asleep. These movements often correspond to what you’re dreaming about, which can sometimes be violent or intense. You might also shout or make vocal sounds during these episodes. RBD usually occurs in the later part of the night and can lead to injuries for you or your bed partner. You might not remember these episodes in the morning, but they can be disruptive and alarming. Recognizing these symptoms early is essential for proper diagnosis and management. Some cases of RBD have been linked to underlying neurological conditions, such as neurodegenerative disorders, which require careful monitoring. Awareness of disorder symptoms can help in understanding the prevalence and impact of such conditions. A higher contrast ratio in home cinema projectors can improve the visibility of details in dark scenes, which is especially helpful for observing subtle movements during sleep studies. Additionally, understanding home sleep testing methods can facilitate earlier detection and treatment of sleep-related disorders.
How RBD Can Signal Underlying Parkinson’s Disease
Research shows that REM Sleep Behavior Disorder often appears years before the motor symptoms of Parkinson’s disease become noticeable, making it a potential early warning sign. If you notice acting out vivid dreams, it could indicate an underlying neurological change. Here’s what to keep in mind:
REM Sleep Behavior Disorder may occur years before Parkinson’s motor symptoms, serving as an early warning sign.
- RBD may precede Parkinson’s by several years, signaling early neurodegeneration.
- It involves disrupted muscle atonia during REM sleep, leading to physical activity.
- Not everyone with RBD develops Parkinson’s, but it raises your risk markedly.
- Recognizing essential oils for sleep and relaxation techniques may help manage some symptoms and improve sleep quality.
- Ongoing research emphasizes the importance of early diagnosis for better management outcomes. Additionally, understanding the diverse genres of symptoms associated with RBD can aid in distinguishing it from other sleep disorders. Recognizing the early signs of RBD can be crucial for timely intervention.
Recognizing the Connection Between Sleep and Motor Symptoms

Understanding how sleep symptoms relate to motor signs can help you identify early signs of Parkinson’s disease. Sleep disturbances often precede visible motor symptoms, serving as early warning signs. For example, REM sleep behavior disorder (RBD) involves acting out dreams, which can hint at underlying neurodegeneration. Recognizing these patterns can prompt earlier medical evaluation and intervention. Additionally, being aware of the emotional support needs of individuals experiencing sleep disturbances can improve overall well-being. Research indicates that addressing sleep quality early may help manage or delay the progression of motor symptoms associated with Parkinson’s. Incorporating tuning strategies from related fields may also offer insights into optimizing sleep health. Furthermore, understanding the underlying neurodegeneration processes can provide deeper insights into diagnosis and treatment options.
Strategies for Managing RBD in Parkinson’s Patients

Managing RBD in Parkinson’s patients requires a combination of behavioral strategies and medical interventions. First, create a safe sleep environment by removing sharp or dangerous objects and padding furniture to prevent injuries during episodes. Second, establish a consistent bedtime routine and sleep schedule to promote regular sleep patterns. Third, discuss medication adjustments with your healthcare provider; some drugs may reduce RBD symptoms or improve sleep quality. Additionally, using a bed alarm can alert you or a caregiver if violent movements occur, enabling quick intervention. Regularly monitoring symptoms and communicating with your healthcare team ensures the most effective management plan. Incorporating Volkswagen Tuning principles, such as optimizing sleep conditions and environment, can enhance overall safety and effectiveness. Exploring evidence-based approaches can further improve safety and treatment outcomes. Understanding self-watering plant pots might seem unrelated, but the consistent moisture control they provide can be an analogy for maintaining stable sleep environments. Maintaining a safe environment is crucial to prevent injuries during episodes. While these strategies help minimize risks and improve sleep, always consult your doctor for personalized treatment options.
When to Seek Medical Advice for Sleep-Related Symptoms

You should seek medical advice promptly if you notice new or worsening sleep-related symptoms, such as vivid dreams, violent movements during sleep, or sudden awakenings. These signs could indicate REM Sleep Behavior Disorder or other sleep disturbances linked to Parkinson’s. Early evaluation by a healthcare professional is essential to determine the cause and develop an appropriate treatment plan. Don’t ignore symptoms that disrupt your sleep or put you or your bed partner at risk. Keep track of the frequency, intensity, and any associated behaviors. If you experience injuries, persistent sleep disruptions, or increased daytime fatigue, seek medical attention immediately. Addressing these symptoms early can improve your sleep quality and overall safety, and help manage underlying neurological conditions effectively.
Frequently Asked Questions
Can RBD Be Reversed or Cured in Parkinson’S Patients?
You might wonder if RBD can be reversed or cured. While there’s no guaranteed cure, treatments like medication and safety measures can markedly reduce symptoms and risks. Managing underlying conditions, such as Parkinson’s, can help improve sleep quality. Staying proactive with your healthcare team, following prescribed therapies, and making lifestyle adjustments can make a noticeable difference, even if complete reversal isn’t currently possible.
Are There Specific Medications to Prevent Injury During RBD Episodes?
Picture yourself safely tucked in bed, yet during an RBD episode, your body acts out vivid dreams, risking injury. To prevent harm, your doctor may recommend medications like clonazepam or melatonin, which calm muscle activity and reduce episodes. These medications act like gentle guardians, helping you stay safe while you sleep. Always talk to your healthcare provider about the best options to protect yourself during these episodes.
How Does RBD Impact the Progression of Parkinson’S Disease?
You might wonder if your sleep behaviors could influence your disease progression. REM Sleep Behavior Disorder (RBD) can increase injury risk and disrupt your quality of life, but current evidence doesn’t show it directly accelerates Parkinson’s progression. However, managing RBD effectively may help you maintain better overall health and safety. Staying vigilant and working with your healthcare team guarantees you address symptoms early, supporting your well-being as your condition evolves.
Are Sleep Disturbances an Early Sign of Parkinson’S Before Motor Symptoms?
Imagine your nights as a delicate dance, where sleep disturbances act as the first whisper of an upcoming storm. You might notice changes like vivid dreams or restless nights before motor signs appear. These early signs are like warning bells, signaling your body to pay closer attention. If you observe these shifts, consider consulting a healthcare professional, as early detection can help manage potential underlying issues more effectively.
What Lifestyle Changes Can Help Reduce RBD Episodes?
To reduce RBD episodes, you can make several lifestyle changes. Create a calming bedtime routine, avoid alcohol and caffeine before sleep, and keep your sleep environment safe by removing sharp objects. Regular exercise during the day can improve sleep quality, but avoid vigorous activity close to bedtime. Managing stress through relaxation techniques like meditation also helps. Consistent sleep schedules and ensuring enough sleep each night support overall sleep health and may lessen episodes.
Conclusion
If you notice unusual movements or vivid dreams disrupting your sleep, don’t delay diagnosing and dealing with RBD. Early evaluation empowers you to address sleep symptoms and potentially uncover Parkinson’s early. Pay attention, pursue proper treatment, and prioritize your peace of mind. Remember, recognizing restless nights and rapid movements can be your first step toward better sleep and better health—because proactive action can prevent problems before they progress. Stay vigilant, seek support, and sleep soundly.









