To identify dementia, it is crucial to look out for signs such as memory loss, poor decision-making, and confusion. Evaluations of behavior and memory, which may include memory assessments, can help pinpoint cognitive decline. Laboratory tests can measure levels of tau and beta-amyloid, while brain imaging techniques such as MRI can provide detailed scans of the brain. EEGs and lumbar punctures can also assist in diagnosis by detecting irregular brain patterns. A comprehensive evaluation involves reviewing medical history and conducting neuro assessments. Understanding these diagnostic steps is key to effectively managing dementia. Delving deeper into these processes can reveal valuable insights for comprehensive dementia care.
Key Takeaways
- Memory loss, poor judgment, confusion, and disorientation are common symptoms.
- Memory testing, behavior pattern observation, and cognitive decline indication aid diagnosis.
- Laboratory tests analyze tau and beta-amyloid levels, ruling out conditions and tracking progression.
- Brain imaging techniques like MRI and CT scans provide valuable insights for specific diagnoses.
- EEGs and lumbar punctures serve as supplementary tools for comprehensive dementia evaluation.
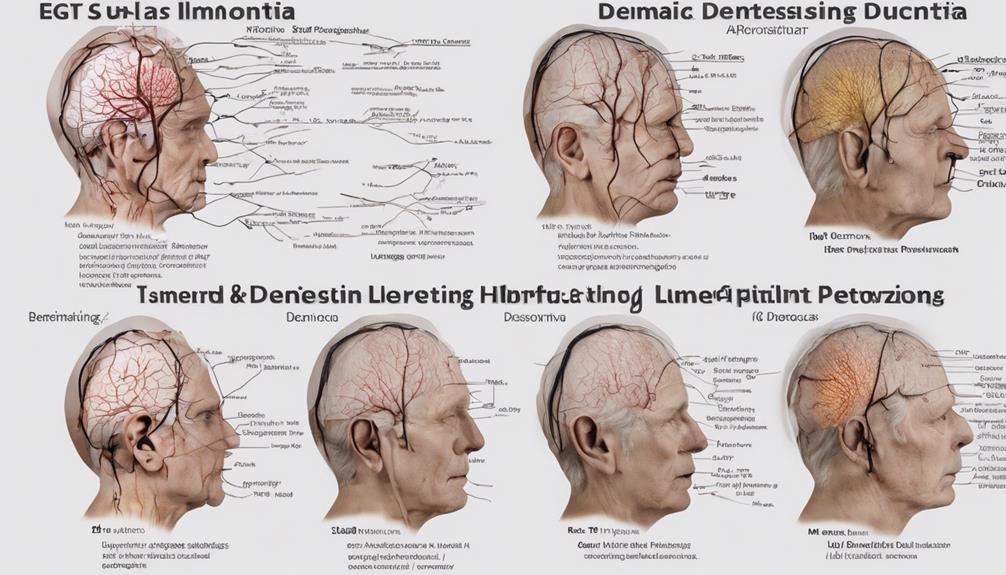
Common Symptoms of Dementia
We commonly observe memory loss as a key symptom of dementia, particularly in individuals who struggle to recall recent events or important information. Alongside memory issues, poor judgment often manifests in those with dementia, impacting their decision-making abilities.
Confusion and disorientation in familiar surroundings can also signal the presence of dementia, causing distress and uncertainty for the individual. Difficulty speaking, understanding, or expressing thoughts may indicate early cognitive decline, highlighting the progressive nature of this condition.
Additionally, symptoms like wandering, getting lost, trouble handling money, and repeating questions are typical in dementia cases, emphasizing the multifaceted challenges individuals face. Recognizing these signs early can aid in timely intervention and support for those affected by dementia, paving the way for better management and quality of life.
Behavioral and Memory Assessments

When evaluating for dementia, it's essential to concentrate on memory testing to assess cognitive function and recall abilities.
Additionally, observing behavior patterns can provide valuable insights into changes in mood, personality, and social interactions that may indicate cognitive decline.
These evaluations play a key role in diagnosing dementia and understanding the progression of the condition.
Memory Testing Importance
Memory testing plays an essential role in diagnosing dementia by evaluating cognitive decline and memory loss. Conducting memory tests, such as the Mini-Mental State Examination (MMSE), is vital for early detection and accurate diagnosis of different types of dementia. These assessments help in identifying early signs of dementia and monitoring progression over time. Behavioral assessments complement memory testing by evaluating changes in behavior, mood swings, and personality shifts that can indicate dementia. By combining memory and behavioral assessments, healthcare professionals can gain a thorough understanding of an individual's cognitive function and provide appropriate interventions. The table below highlights the importance of memory testing in diagnosing dementia:
| Memory Testing Benefits | Description |
|---|---|
| Early Detection | Identifying cognitive decline and memory loss early on |
| Progression Monitoring | Tracking changes over time to assess disease progression |
| Accurate Diagnosis | Differentiating between various types of dementia for targeted treatment |
| Cognitive Impairment Assessment | Measuring cognitive function and memory deficits |
| Comprehensive Evaluation | Combining memory and behavioral assessments for a holistic understanding of the individual's condition |
Behavior Patterns Evaluation
Evaluation of behavior patterns and memory in dementia diagnosis provides essential insights into the individual's cognitive and emotional functioning. Behavioral assessments focus on changes in behavior patterns, social interactions, and emotional responses, aiding in understanding the impact on daily living activities and decision-making capabilities.
Memory assessments explore memory loss, including short-term memory difficulties, long-term memory recall, and recent event forgetfulness. These assessments may involve standardized tests like the Mini-Mental State Examination (MMSE) to evaluate cognitive functions such as memory, attention, and language skills.
Laboratory Tests for Dementia
When considering laboratory tests for dementia, it's essential to prioritize blood tests and brain imaging. These assessments play a pivotal role in ruling out underlying conditions that could be contributing to cognitive decline.
Blood Tests
Blood tests are essential for diagnosing dementia due to their ability to analyze markers like tau and beta-amyloid levels. They aid in ruling out conditions that mimic dementia symptoms, monitoring treatment efficacy, and tracking disease progression. Moreover, investigating blood markers supports drug development and improves the design of clinical trials. Although not standard practice in clinical settings, blood tests hold great potential for transforming dementia diagnosis.
Blood tests play a crucial role in diagnosing dementia by analyzing markers such as tau and beta-amyloid levels. These tests help in ruling out conditions mimicking dementia symptoms, track treatment effectiveness, and disease progression. Investigating blood markers supports drug development and enhances clinical trial design. While not yet routine in clinical settings, blood tests show promise for revolutionizing dementia diagnosis.
Brain Imaging
Brain imaging tests, such as MRI and CT scans, are pivotal in diagnosing dementia as they can help rule out other conditions and confirm the specific type of dementia by revealing brain abnormalities like shrinkage. MRI scans offer detailed brain images, while CT scans detect strokes or tumors mimicking dementia symptoms. SPECT and PET scans assess brain function and blood flow, aiding in specific dementia diagnoses. EEG tests, though uncommon, detect unusual brain activity linked to conditions like epilepsy. In in some cases, a lumbar puncture analyzes cerebrospinal fluid for dementia markers. These imaging techniques play an important role in accurately diagnosing dementia by providing valuable insights into brain structure and function.
| Imaging Test | Purpose | Use in Dementia Diagnosis |
|---|---|---|
| MRI | Detailed brain images | Confirms brain abnormalities |
| CT scan | Detects strokes and tumors | Rules out conditions resembling dementia |
| SPECT scan | Evaluates brain function | Helps in specific dementia diagnoses |
| PET scan | Assesses blood flow | Provides additional insights for diagnosis |
Imaging Techniques in Diagnosis
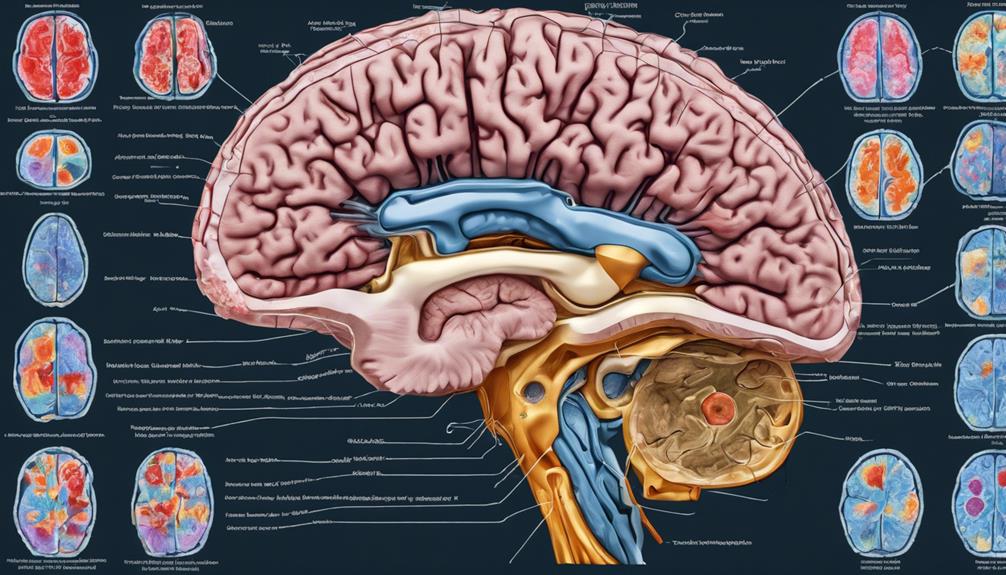
Utilizing advanced imaging techniques is essential in diagnosing dementia as they provide detailed insights into brain structure and function. When it comes to brain imaging for dementia diagnosis, CT scans and MRI scans play an important role in identifying structural changes that may indicate the presence of the condition. Additionally, SPECT and PET scans are valuable tools for evaluating brain function and detecting any abnormalities in blood flow, aiding in the accurate diagnosis of specific types of dementia.
MRI scans are particularly effective in confirming the type of dementia and revealing patterns of brain shrinkage associated with conditions like Alzheimer's disease. By using these imaging techniques, healthcare professionals can improve the accuracy of dementia diagnoses, ruling out other conditions such as brain tumors or strokes that may present similar symptoms. This ensures that individuals receive appropriate treatment tailored to their specific condition.
Additional Diagnostic Procedures

When exploring further diagnostic procedures for dementia, additional scans beyond MRI and CT scans can provide more detailed information about brain function. Tests like SPECT and PET scans are recommended when initial imaging results are inconclusive, offering insights into brain blood flow abnormalities. These scans play an important role in evaluating brain function, aiding in the early diagnosis of diseases like Alzheimer's. While EEG tests are rare, they can detect unusual brain activity in specific cases, especially when epilepsy is suspected. Additionally, lumbar punctures, also known as spinal taps, involve analyzing spinal fluid to diagnose certain types of dementia. These procedures are essential in understanding the mental processes and memory functions affected by various brain conditions. Autopsy post-death is sometimes necessary for definitive identification of the underlying causes of dementia. Below is a table summarizing the key additional diagnostic procedures for evaluating dementia:
| Diagnostic Procedure | Purpose |
|---|---|
| SPECT and PET Scans | Evaluate brain function and blood flow |
| EEG | Detect unusual brain activity |
| Lumbar Puncture | Analyze spinal fluid for diagnosis |
| Autopsy | Definitive identification post-death |
Role of EEGs and Lumbar Punctures
Exploring further diagnostic tools beyond standard imaging scans, EEGs and lumbar punctures play a pivotal role in evaluating brain function and detecting specific abnormalities related to dementia.
EEGs, or electroencephalograms, measure brain activity, aiding in distinguishing dementia from delirium and identifying abnormal brain patterns. This tool provides valuable insights into brain function and can pinpoint specific abnormalities associated with various forms of dementia.
Additionally, lumbar punctures, also known as spinal taps, involve collecting cerebrospinal fluid to analyze protein levels and biomarkers linked to dementia. By evaluating biomarkers like tau and beta-amyloid, lumbar punctures can indicate the presence of Alzheimer's disease or other types of dementia.
Both EEGs and lumbar punctures serve as essential supplementary diagnostic tools that, when combined with imaging tests and cognitive assessments, contribute significantly to the thorough evaluation of dementia.
Comprehensive Dementia Evaluation

In a thorough dementia evaluation, detailed medical history review plays a significant role in identifying symptoms and potential causes. Neuropsychological tests are conducted to evaluate cognitive function, memory, language skills, and orientation levels. These tests provide valuable insights into the individual's cognitive abilities and help in determining the presence and severity of dementia.
Additionally, neurological evaluations aid in identifying abnormalities in reflexes, coordination, muscle strength, and eye movements, which can further contribute to the diagnostic process. Brain imaging scans, such as MRI and CT scans, are essential for visualizing brain structure and ruling out other potential conditions that may mimic dementia symptoms.
Laboratory tests, including blood tests, CSF analysis, and genetic testing, may also be included to provide additional information for diagnosing and evaluating dementia. A thorough evaluation that incorporates these various tests is essential in accurately understanding and grasping the complexities of dementia, guiding healthcare professionals towards appropriate management and care strategies.
Frequently Asked Questions
What Tests Are Done to Confirm Dementia?
When confirming dementia, various tests are typically conducted. These include cognitive assessments and brain imaging scans like MRI or CT, which help identify memory issues and brain abnormalities, while also ruling out other potential causes. Laboratory tests may also be performed to check for underlying medical conditions. Additional tests like PET scans or EEGs can offer more detailed information. In some rare cases, autopsy post-mortem may be necessary for a definitive diagnosis.
What Assessment Is Used to Diagnose Dementia?
When diagnosing dementia, a variety of assessments is employed to evaluate cognitive functions, memory, language skills, and orientation. Neurological examinations help pinpoint physical abnormalities that may indicate dementia.
Brain imaging techniques like MRI and CT scans are essential for confirming dementia type and ruling out other conditions. EEG tests measure brain activity, aiding in distinguishing dementia from delirium.
These evaluations, along with spinal fluid analysis and post-mortem examinations, provide a thorough diagnostic picture.
What Is the 12 Question Test for Dementia?
The 12 Question Test for Dementia, also known as the General Practitioner Assessment of Cognition (GPCOG), is a brief screening tool that evaluates cognitive function and memory.
It includes questions on memory, orientation, and language skills. GPCOG scores can be influenced by factors like education level.
While this test can't diagnose dementia directly, it can signal potential memory issues.
It's an essential tool in the initial assessment of cognitive function.
What Is the Diagnostic Exam for Dementia?
When diagnosing dementia, a thorough medical history review and mental status exam are essential.
Lab tests like thyroid hormone and Vitamin B12 levels help rule out other conditions.
Imaging tests like CT scans identify brain abnormalities.
Additional tests like EEG measure brain activity.
Combining these evaluations gives a detailed view for an accurate diagnosis.
Proper assessment is key for early intervention and management of dementia.
Conclusion
In diagnosing dementia, it's essential to recognize the common symptoms. This includes conducting behavioral and memory assessments and utilizing laboratory tests and imaging techniques. Additional diagnostic procedures such as EEGs and lumbar punctures may also be necessary for a thorough evaluation. Early detection is crucial, as recognizing common dementia warning signs can help initiate timely interventions and support. These warning signs often include memory loss, difficulty with problem-solving, and changes in mood or behavior. By combining clinical evaluations with the latest diagnostic tools, healthcare professionals can develop personalized care plans to address the unique needs of each patient.
By addressing these steps systematically, healthcare professionals can provide a clearer picture of the condition and guide appropriate treatment plans. Remember, early detection and intervention are key in managing dementia effectively.