Protein accumulation, particularly alpha-synuclein, in the brain plays a crucial role in the development of dementia with Lewy bodies. These proteins create abnormal Lewy bodies that interfere with communication among brain cells. Changes in important brain chemicals like dopamine and serotonin contribute to cognitive decline, impacting memory and behavior. Symptoms worsen over time, including cognitive fluctuations, motor difficulties, and hallucinations. Understanding these underlying causes is vital for accurate diagnosis and treatment. Personalized treatment options, targeting specific symptoms, offer comprehensive care. By understanding these concepts, we gain valuable knowledge for the management and treatment of dementia with Lewy bodies.
Key Takeaways
- Protein accumulation, especially alpha-synuclein, in the brain is a key factor.
- Abnormal Lewy bodies formation disrupts normal brain function.
- Shared pathology with Parkinson's disease suggests common underlying mechanisms.
- Uncertainty surrounds the exact cause of Lewy body formation.
- Understanding protein accumulation and Lewy bodies is crucial for treatment development.
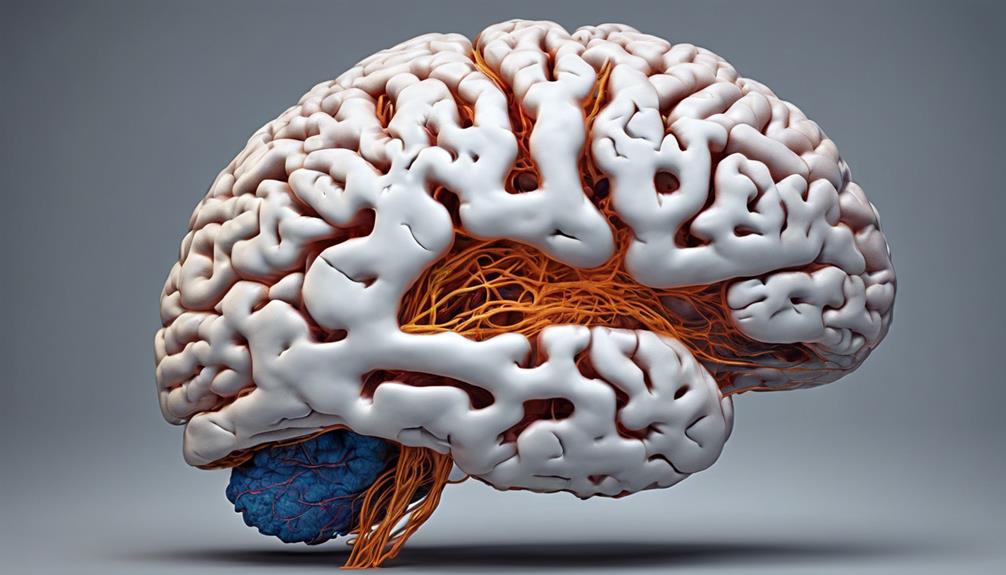
Protein Accumulation in the Brain
Protein accumulation in the brain plays a pivotal role in the development of dementia with Lewy bodies, characterized by the presence of abnormal Lewy bodies primarily composed of alpha-synuclein protein. These Lewy bodies, made up of alpha-synuclein protein, are responsible for disrupting normal brain function, leading to cognitive decline. The aggregation of alpha-synuclein in brain cells contributes importantly to the symptoms and progression of dementia with Lewy bodies. As these abnormal proteins accumulate, they interfere with the communication between brain cells, ultimately impacting memory, thinking, and behavior.
Understanding the impact of Lewy bodies and alpha-synuclein protein is important in diagnosing and managing dementia effectively. The presence of these abnormal protein deposits not only distinguishes dementia with Lewy bodies but also links it to other neurodegenerative conditions like Parkinson's disease. By recognizing the role of protein accumulation in the brain, healthcare professionals can tailor treatment plans to address the underlying causes of cognitive decline in individuals affected by this condition.
Formation of Lewy Bodies

The process of Lewy bodies formation in the brain remains a vital and intriguing phenomenon under ongoing investigation. Lewy bodies are abnormal protein deposits primarily composed of alpha-synuclein. These deposits disrupt normal brain cell function and communication, contributing to conditions like Dementia with Lewy Bodies and Parkinson's disease. The exact mechanism behind the formation of Lewy bodies and their role in neurodegeneration isn't yet fully understood by researchers.
Studies suggest that the aggregation of alpha-synuclein into Lewy bodies plays a significant role in neuronal dysfunction and cell death in affected brain regions. This aggregation process leads to the formation of these abnormal protein clumps, which then interfere with the brain's ability to function correctly. Understanding how Lewy bodies form and their impact on brain health is pivotal in developing effective treatments for conditions like Dementia with Lewy Bodies. By unraveling the mysteries behind Lewy bodies formation, researchers aim to find ways to prevent or slow down the progression of these debilitating neurodegenerative diseases.
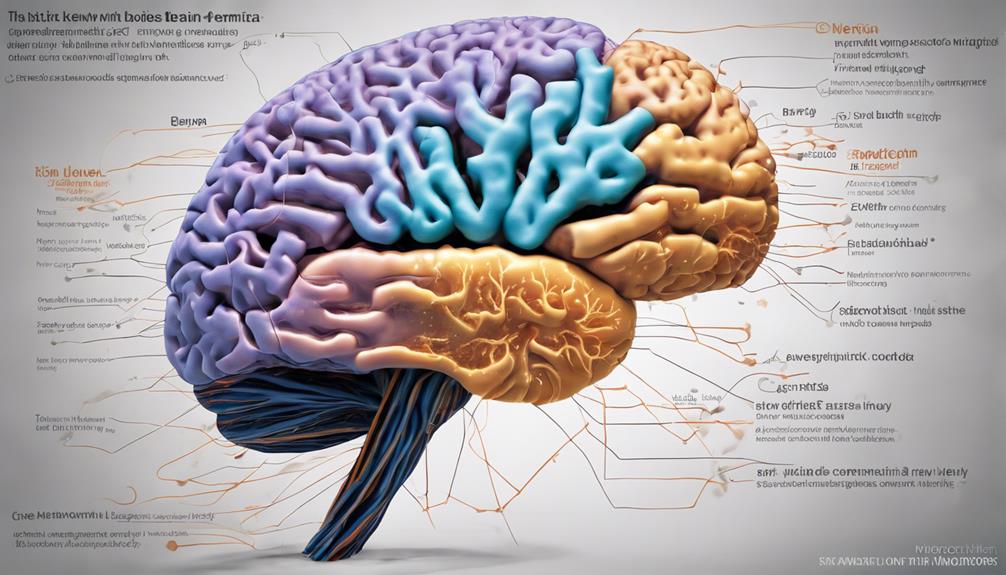
Impact on Brain Chemicals
How do abnormal protein deposits in the brain impact the levels of essential chemicals important for cognitive and motor functions in individuals with Dementia with Lewy bodies? In Dementia with Lewy bodies, the accumulation of Lewy bodies disrupts the normal function of brain chemicals critical for proper brain function. These changes in brain chemicals, including dopamine and acetylcholine, play a significant role in the cognitive impairment and motor symptoms experienced by individuals with this condition. Additionally, alterations in brain chemicals like serotonin and norepinephrine can influence mood, behavior, and cognitive functions in those affected by dementia with Lewy bodies.
To better understand this impact, let's explore a table highlighting the relationship between Lewy bodies and brain chemicals:
| Brain Chemical | Impact on Dementia with Lewy Bodies |
|---|---|
| Dopamine | Related to motor symptoms and cognition |
| Acetylcholine | Affects cognitive functions and memory |
| Serotonin | Influences mood and behavior changes |
| Norepinephrine | Impacts cognitive functions and alertness |
Abnormal Protein Deposits

Upon accumulation in the brain, Lewy bodies disrupt normal brain functions, leading to the development of cognitive and motor symptoms in individuals with Dementia with Lewy bodies. These abnormal protein deposits, known as Lewy bodies, are primarily composed of alpha-synuclein. Alpha-synuclein is a protein that normally functions in the brain to help neurons communicate. However, in Dementia with Lewy bodies, this protein becomes misfolded and starts clumping together, forming Lewy bodies. These Lewy bodies interfere with the normal signaling processes in the brain, causing damage to nerve cells and impairing cognitive abilities and motor functions.
The presence of Lewy bodies filled with alpha-synuclein is a characteristic feature not only of Dementia with Lewy bodies but also of Parkinson's disease. The exact reasons why these abnormal protein deposits form and how they contribute to the progression of Dementia with Lewy bodies are still areas of active research. Understanding the role of alpha-synuclein in the development of Lewy bodies is vital for developing effective treatments to target these abnormal protein deposits and potentially slow down the progression of the disease.
Disease Development and Progression
As dementia with Lewy bodies progresses, individuals may experience a range of symptoms that evolve over time.
These symptoms include cognitive fluctuations, where mental abilities vary throughout the day, impacting focus and attention.
Motor and behavior changes can also occur, affecting movement coordination and leading to alterations in mood and personality.
Symptoms Over Time
Symptoms in dementia with Lewy bodies gradually progress over years, starting with mild cognitive impairments. As time passes, various changes become apparent in individuals with this condition. Here are some symptoms that develop and change over the course of the disease: Symptoms such as fluctuations in attention and alertness, visual hallucinations, and motor difficulties often emerge as the disease advances. Over time, lewy body dementia deterioration can lead to increased difficulty with movement, severe cognitive impairment, and challenges in managing day-to-day activities. These worsening symptoms significantly impact both quality of life and the ability to live independently.
- Memory Issues: Initially mild, memory problems worsen as the disease advances.
- Visual Hallucinations: Individuals may start experiencing seeing things that aren't there.
- Fluctuations in Alertness: The level of alertness and attention can vary throughout the day.
- Movement Symptoms: Slowed movement, tremors, and muscle stiffness tend to become more pronounced over time.
Understanding these evolving symptoms can help in recognizing and managing the progression of Lewy body dementia effectively.
Cognitive Fluctuations
Considering the dynamic nature of cognitive fluctuations in Dementia with Lewy Bodies, these unpredictable changes play a vital role in the disease's progression and impact on daily functioning. Cognitive fluctuations refer to rapid shifts in alertness, attention, and thinking abilities that can vary throughout the day.
These fluctuations are a hallmark feature of Dementia with Lewy Bodies, distinguishing it from other types of dementia. The severity and frequency of these fluctuations can greatly affect daily activities and quality of life.
Understanding and managing cognitive fluctuations are essential in providing appropriate care and support for individuals with this condition. Monitoring changes in alertness and thinking abilities, and adapting activities accordingly, can help improve the overall well-being of individuals living with Dementia with Lewy Bodies.
Motor and Behavior Changes
Motor and behavior changes are pivotal indicators of disease development and progression in dementia with Lewy bodies. These changes manifest through slowed movements, limb stiffness, tremors, agitation, aggression, and depression, ultimately leading to increased functional impairment over time. These changes have a profound impact on daily activities and quality of life for individuals with dementia and can be distressing for both the affected individual and their caregivers. Understanding these motor and behavior changes is essential for providing appropriate care and support. By recognizing and addressing these symptoms early on, healthcare providers and caregivers can better manage the progression of the disease and improve the overall well-being of those living with dementia with Lewy bodies.
Let's explore further the details of these changes:
- Motor changes can include slowed movements, limb stiffness, and tremors.
- Behavioral changes often involve agitation, aggression, and depression.
- These changes can lead to increased functional impairment over time.
- Symptoms are usually more pronounced in later stages of the disease.
Cognitive Symptoms Manifestation

Memory and attention are vital aspects affected by dementia with Lewy bodies, leading to difficulties in recalling recent events and staying focused.
Visual-spatial skills, which help us perceive and interact with our environment, may also decline, impacting tasks like reading maps or finding our way through spaces.
These cognitive symptoms can vary in severity and progression, influencing daily life and relationships greatly.
Memory and Attention
Experiencing difficulties with memory recall and attention is a common cognitive symptom observed in individuals with dementia with Lewy bodies. When dealing with memory problems and attention deficits, it's important to grasp how these issues can impact daily life.
Here are some key points to take into account:
- Memory recall may be challenging, affecting the ability to recollect recent events or conversations.
- Attention deficits can lead to difficulty concentrating on tasks or becoming easily sidetracked.
- Executive function changes may result in difficulties with planning, organizing, and multitasking.
- These cognitive symptoms can impact decision-making and problem-solving abilities, making it vital to seek support and understanding for individuals affected by dementia with Lewy bodies.
Visual-Spatial Skills
Moving through spatial environments and judging distances can pose significant challenges for individuals with dementia with Lewy bodies due to impaired visual-spatial skills. In Lewy body dementia, these skills refer to understanding and interpreting the spatial relationships between objects. People with this condition may find tasks like finding their way in unfamiliar places or estimating distances challenging. Recognizing shapes, sizes, and understanding spatial orientations can also be difficult.
Evaluating visual-spatial skills is essential in diagnosing and tracking the cognitive decline linked to dementia with Lewy bodies. Difficulties in activities such as driving, reading maps, or assembling objects may indicate a decline in these abilities. Understanding and supporting individuals with impaired visual-spatial skills is crucial in providing appropriate care for those affected by Lewy body dementia.
Motor Symptoms Onset
At the early stages of Dementia with Lewy Bodies, individuals may notice the onset of motor symptoms characterized by slowed movement, tremors, limb stiffness, and postural instability. These symptoms, linked to the presence of Lewy bodies in the brain, play an important role in affecting movement control.
Here are some essential points to help you understand the motor symptoms onset in Dementia with Lewy Bodies:
- Early Appearance: Motor symptoms often manifest early in the disease progression of Dementia with Lewy Bodies.
- Specific Symptoms: These can include slowed movement, tremors, stiffness in limbs, and difficulties with maintaining balance.
- Distinguishing Factor: The onset of motor symptoms in DLB can differentiate it from Alzheimer's disease, where such symptoms typically emerge later.
- Importance of Recognition: Early recognition and management of these motor symptoms are crucial for providing timely care and support to individuals with Dementia with Lewy Bodies.
Behavioral Symptoms Emergence

Behavioral symptoms often surface early in the progression of dementia with Lewy bodies, impacting various aspects of individuals' daily lives. These symptoms, such as agitation, aggression, anxiety, and hallucinations, can greatly affect the quality of life for those with Lewy body dementia. It's important to recognize that these behavioral changes may appear before or along with cognitive decline in some instances. Managing these symptoms effectively requires a thorough approach involving healthcare professionals and caregivers working together.
Understanding and addressing behavioral symptoms promptly can help enhance the well-being of individuals living with dementia with Lewy bodies. By providing appropriate support and interventions, we can improve the overall quality of life for those experiencing these challenges. It's essential to approach these symptoms with empathy, patience, and a willingness to adapt strategies as needed. Together, we can help individuals navigate the complexities of dementia with Lewy bodies and work to maintain their dignity and comfort.
Underlying Causes Exploration
Exploring the underlying causes of dementia with Lewy bodies reveals a complex interplay of factors contributing to the formation of abnormal protein deposits in the brain. Understanding these causes is vital in developing effective treatment strategies for individuals affected by this condition. Here are some key points to ponder:
- Accumulation of Protein: The buildup of abnormal protein deposits, known as Lewy bodies, in the brain is a hallmark feature of dementia with Lewy bodies. These deposits disrupt normal brain functions, leading to cognitive decline and other symptoms of dementia.
- Brain Functions Disruption: The presence of Lewy bodies interferes with essential brain functions, such as memory, reasoning, and perception. This disruption contributes to the cognitive impairment seen in individuals with dementia with Lewy bodies.
- Unclear Development Cause: While the exact cause of Lewy body formation in the brain is still unclear, ongoing research aims to unravel the underlying mechanisms involved in this process.
- Shared Pathology: The presence of Lewy bodies in both dementia with Lewy bodies and Parkinson's disease suggests a shared pathology between these conditions, highlighting the complexity of neurodegenerative disorders.
Tailored Treatment Approaches
When addressing Dementia with Lewy Bodies, our focus is on tailoring treatment to manage specific symptoms like cognitive decline, visual hallucinations, and movement issues.
Personalized medication plans, individual therapy options, and targeted symptom management are key components of these customized approaches.
It's important to work closely with specialists, like neurologists and therapists, to create a thorough care plan that meets the unique needs of individuals with DLB.
Personalized Medication Plans
In personalized medication plans for dementia with Lewy bodies, treatments are tailored to address individual symptoms and needs. When creating personalized medication plans for Lewy body dementia, it's vital to take into account the unique challenges each person faces.
Here are some key points to understand about personalized medication plans:
- Medications are prescribed based on specific symptoms like cognitive impairment, movement difficulties, or hallucinations.
- Tailored treatment approaches aim to optimize symptom management and improve the quality of life for individuals with Lewy body dementia.
- The effectiveness of personalized medication plans may vary among patients, highlighting the importance of ongoing monitoring and adjustments.
- Customized medication plans play a pivotal role in providing individualized care and support for those living with dementia with Lewy bodies.
Individual Therapy Options
Personalized medication plans tailored to address the specific symptoms of dementia with Lewy bodies may smoothly shift into individual therapy options, focusing on personalized approaches to enhance cognitive, behavioral, and emotional well-being.
Individual therapy for Lewy body dementia involves tailored treatment plans that can include cognitive behavioral therapy (CBT) to manage anxiety, depression, and agitation. Psychotherapy is also beneficial in helping individuals cope with the emotional impact of the disease, improve communication skills, and enhance their quality of life.
Counseling sessions within individual therapy offer support, guidance, and strategies for both patients and caregivers to navigate the challenges associated with living with Lewy body dementia. The goal of individual therapy is to empower patients to develop coping mechanisms, enhance self-awareness, and improve overall well-being through personalized interventions.
Targeted Symptom Management
Tailored treatment approaches for dementia with Lewy bodies aim to address specific symptoms such as cognitive fluctuations, visual hallucinations, and movement difficulties. To effectively manage these symptoms, the following targeted approaches can be considered:
- Cholinesterase Inhibitors: These medications can help improve cognitive function and thinking abilities in individuals with Lewy body dementia.
- Antipsychotic Medications: Caution is advised when using these drugs to prevent worsening symptoms like hallucinations and confusion in individuals with dementia with Lewy bodies.
- Behavioral Therapies: Incorporating behavioral interventions can help address mood changes and agitation commonly seen in individuals with Lewy body dementia.
- Interdisciplinary Approach: Tailored treatment plans often involve a team of healthcare professionals, including neurologists, psychiatrists, therapists, and caregivers, to provide all-encompassing care and support for individuals with dementia with Lewy bodies.
Frequently Asked Questions
What Are the Most Common Causes of Dementia With Lewy Bodies?
We believe the most common causes of dementia with Lewy bodies include abnormal protein deposits in the brain known as Lewy bodies. These deposits disrupt brain function, leading to neuron loss and neurotransmitter imbalances, impacting cognitive abilities.
Can You Prevent Lewy Body Dementia?
We cannot prevent Lewy body dementia, but early detection and healthy habits can support brain health. While no guarantees exist, understanding risk factors and symptoms aids in timely management. Our focus is on enhancing quality of life.
Who Is Most Likely to Get Lewy Body Dementia?
We, as a group, understand that individuals over 60, especially men, are more likely to develop Lewy body dementia. Factors like family history of this condition or Parkinson's disease can increase one's risk.
What Are 3 Signs of Lewy Body Dementia?
Fluctuating alertness, visual hallucinations, and movement difficulties are three key signs of Lewy body dementia. These symptoms can vary in intensity and frequency, impacting daily life immensely. Seeking medical advice for proper evaluation and management is vital.
Conclusion
To summarize, grasping the reasons behind dementia with Lewy bodies is essential in crafting personalized treatment approaches.
By delving into the fundamental factors such as protein buildup in the brain and irregular protein deposits, we can gain a better understanding of the disease's development and progression.
Identifying the onset of motor symptoms and emergence of behavioral symptoms allows for early intervention.
By addressing these key elements, we can enhance the quality of life for individuals impacted by this condition.