When assessing the effects of Raynaud’s disease on the heart, it is crucial to comprehend the possible dangers it presents to cardiovascular well-being.
While the immediate effects may not be readily apparent, the long-term implications on heart function can be significant.
From mimicking symptoms of more serious heart conditions to potentially increasing the likelihood of cardiac events, the relationship between Raynaud's and heart health warrants a closer examination for those affected.
Key Takeaways
- Raynaud's can mimic angina symptoms.
- Heart murmurs and failure risk increased.
- Proper cardiovascular care crucial.
- Secondary Raynaud's linked to heart complications.
Understanding Raynaud's Disease
Understanding Raynaud's Disease involves delving into the intricate mechanisms that govern vascular responses in the extremities, shedding light on the episodic color changes observed in the fingers and toes due to compromised blood flow.
Raynaud's Syndrome manifests as an exaggerated vascular response to cold or emotional stress. Its primary symptoms include the skin of the fingers turning white or blue due to reduced blood flow, followed by redness as circulation improves.
While primary Raynaud's is typically benign, secondary Raynaud's can be associated with underlying conditions like autoimmune diseases. Calcium channel blockers are commonly prescribed to manage symptoms by dilating blood vessels and improving circulation.
However, individuals with Raynaud's, especially secondary Raynaud's, face an increased risk of heart-related complications. Understanding these dynamics is crucial for healthcare providers to offer comprehensive care to patients with Raynaud's Disease and mitigate potential cardiovascular risks associated with this condition.
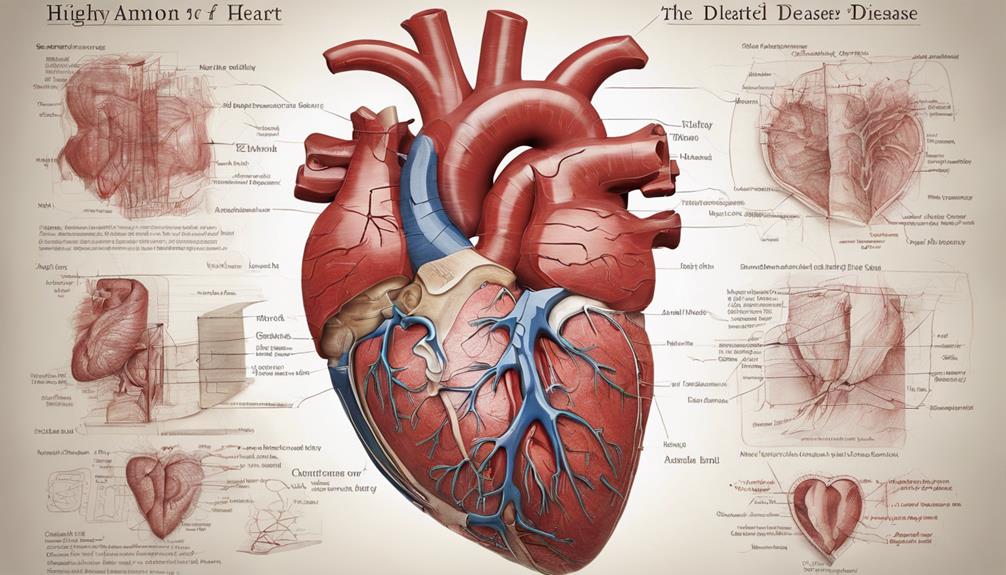
Impact on Heart Health

Raynaud's disease may present symptoms resembling angina or coronary artery disease, potentially leading to misunderstandings and delays in diagnosis. While Raynaud's disease itself doesn't directly cause high blood pressure, it's linked to underlying conditions that can impact heart health. Individuals with Raynaud's disease may face an elevated risk of developing heart murmurs, heart failure, and potentially atrial fibrillation. Understanding the implications of Raynaud's disease on the heart is critical for managing associated risks and ensuring proper cardiovascular care. Proper diagnosis and management of Raynaud's disease are essential to prevent complications that could affect heart health.
- Raynaud's disease can contribute to the development of heart murmurs.
- Individuals with Raynaud's disease may have an increased risk of heart failure.
- The condition is associated with a potential risk of atrial fibrillation.
- Proper cardiovascular care is crucial for individuals with Raynaud's disease.
- Late diagnosis and mismanagement of Raynaud's disease can lead to complications impacting heart health.
Primary Vs Secondary Raynaud's
Differentiating between primary and secondary Raynaud's involves understanding distinct triggers and underlying conditions associated with each variant. Primary Raynaud's disease, more common and often genetically linked, primarily affects women aged 15-40. On the other hand, secondary Raynaud's is associated with underlying conditions such as atherosclerosis, cryoglobulinemia, or autoimmune disorders. While primary Raynaud's is typically triggered by exposure to cold or strong emotions, secondary Raynaud's can be exacerbated by medications or existing diseases. Secondary Raynaud's is also associated with complications like migraines, variant angina, and pulmonary hypertension. Treatment for secondary Raynaud's focuses on managing the underlying disorder to alleviate symptoms and prevent potential heart complications.
| Primary Raynaud's | Secondary Raynaud's |
|---|---|
| More common | Associated with underlying conditions |
| Genetic component | Exacerbated by medications or diseases |
| Triggered by cold or strong emotions | Linked to atherosclerosis, cryoglobulinemia, or autoimmune disorders |
Heart-related Symptoms and Complications

Exploring the impact of Raynaud's disease on the heart unveils a spectrum of symptoms and complications that warrant careful monitoring and management. Individuals with Raynaud's disease may experience symptoms similar to angina, such as chest discomfort or pain. Moreover, they could be at an increased risk of heart murmurs and heart failure. While Raynaud's disease itself doesn't directly cause high blood pressure, it's linked to conditions that can impact heart health. Additionally, there's a heightened risk of developing atrial fibrillation in individuals with Raynaud's disease. Therefore, monitoring heart health and promptly seeking medical attention for any concerning symptoms are crucial, especially for those with secondary Raynaud's.
- Symptoms similar to angina (chest discomfort or pain)
- Increased risk of heart murmurs and heart failure
- Association with conditions affecting heart health
- Elevated risk of atrial fibrillation
- Importance of monitoring heart health, especially for secondary Raynaud's
Diagnosis and Management
To effectively diagnose and manage Raynaud disease's impact on the heart, physicians rely on a combination of clinical assessments and specialized tests. When assessing patients with Raynaud's for potential heart conditions such as angina or coronary artery disease, doctors may perform various tests to evaluate heart health and monitor cardiovascular risks. These tests can help in early diagnosis and appropriate management of heart-related complications associated with Raynaud's. It's crucial for healthcare providers to be vigilant in monitoring individuals with Raynaud's, especially those with secondary Raynaud's linked to underlying disorders. Regular check-ups and screenings can aid in detecting any abnormalities in heart function, such as heart murmurs or atrial fibrillation, allowing for timely intervention and management.
| Diagnostic Tests | Purpose | Frequency |
|---|---|---|
| Echocardiogram | Evaluate heart structure and function | Periodic |
| Electrocardiogram | Monitor heart's electrical activity | As needed |
| Stress Test | Assess heart's response to exertion | As recommended |
Frequently Asked Questions
What Organ System Does Raynaud's Disease Affect?
Raynaud's disease primarily affects the peripheral vascular system, causing arterial constriction in the fingers and toes. It doesn't directly impact the heart muscle.
However, individuals with Raynaud's may have an increased risk of developing cardiovascular conditions like hypertension, coronary artery disease, and heart failure.
Monitoring heart health is crucial for those with Raynaud's, especially with secondary Raynaud's, to prevent heart-related complications.
What Is the Life Expectancy of Someone With Raynaud's Syndrome?
Our research indicates that the life expectancy of individuals with Raynaud's Syndrome is typically normal.
While the syndrome itself doesn't directly impact life expectancy, severe cases can lead to complications like digital ulcers or gangrene, affecting quality of life.
Proper management and regular monitoring can improve health outcomes.
It's essential to address any cardiovascular complications promptly to maintain heart health in individuals with Raynaud's Syndrome.
How Bad Can Raynaud's Disease Get?
Raynaud's disease can get pretty severe, causing intense episodes of blood vessel constriction in response to cold or stress. These episodes can lead to tissue damage, ulcers, and even gangrene in extreme cases.
Severe Raynaud's can significantly impact a person's quality of life, making simple tasks challenging and painful. Seeking proper medical advice and treatment is crucial to manage the symptoms and prevent complications.
What Medications Should Be Avoided With Raynaud's Syndrome?
We must avoid beta-blockers, clonidine, and ergot preparations in Raynaud's syndrome. These drugs can worsen vasoconstriction and exacerbate symptoms.
Opting for calcium channel blockers or prazosin is more suitable for managing symptoms effectively. It's crucial to consult a healthcare provider for proper medication management in individuals with Raynaud's syndrome.
Preventing the triggering or worsening of Raynaud's episodes is paramount, and choosing appropriate medications is key.
Conclusion
In conclusion, Raynaud's disease can have a significant impact on heart health, akin to a turbulent storm on a fragile ship. Individuals with Raynaud's, especially those with secondary Raynaud's, are at a higher risk of heart-related complications.
It's essential to monitor heart health, manage shared risk factors, and seek appropriate medical care to mitigate the potential risks associated with this condition. Further research is necessary to fully understand the intricate relationship between Raynaud's disease and cardiovascular well-being.