When navigating the complex network of blood vessels in the heart, it is crucial to take into account the effects of microvascular heart disease. This condition, which is not as well-known, poses distinct challenges that differ from those observed in typical coronary artery disease.
As we navigate through the complexities of this ailment, it becomes evident that understanding its subtle nuances is crucial for effective management.
Let's uncover the intricacies of microvascular heart disease and shed light on the latest advancements in diagnosis and treatment that are shaping the landscape of cardiovascular health.
Key Takeaways
- Critical for women, diabetics, and those with high blood pressure
- Symptoms include chest pain, fatigue, and shortness of breath
- Specialized tests like CFR and cardiac MRI essential for accurate diagnosis
- Lifestyle changes, medication, and regular monitoring key for treatment and prevention
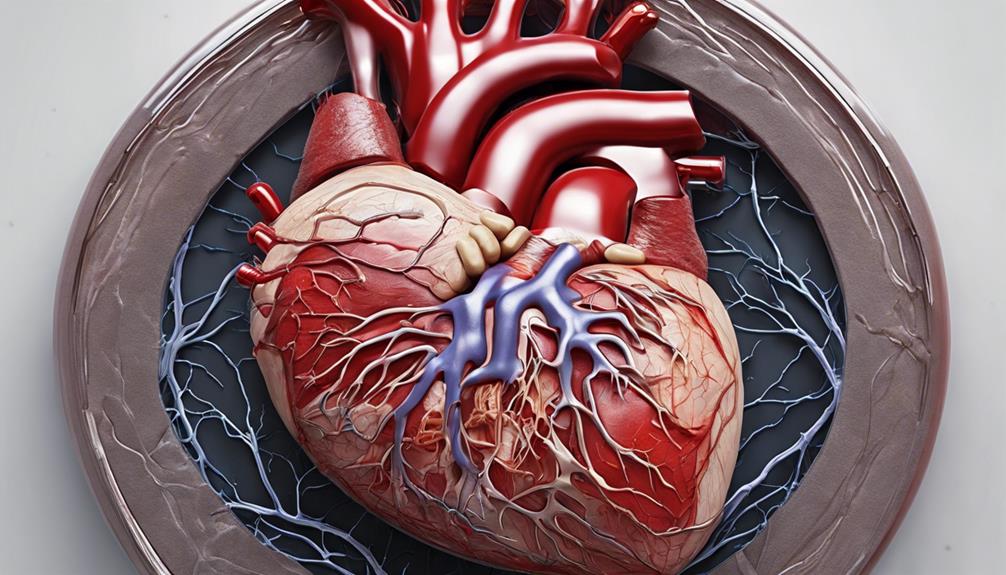
Overview of Microvascular Heart Disease
Microvascular heart disease, also referred to as coronary microvascular disease or microvascular endothelial dysfunction, impacts the microscopic blood vessels within the heart, resulting in compromised blood flow and potential complications. This condition specifically affects the small vessels of the heart, which play a crucial role in supplying oxygen and nutrients to the heart muscle. Microvascular heart disease is a significant concern in healthcare, especially for women, diabetics, and individuals with high blood pressure, as they're more prone to developing this condition. Small vessel disease not only affects the heart but can also have broader implications, such as contributing to cognitive decline and increasing the risk of strokes.
Recognizing the symptoms of microvascular heart disease is vital for timely intervention. Patients may experience chest pain, shortness of breath, fatigue, and discomfort in various areas like the left arm, jaw, neck, back, or abdomen. Understanding these signs can aid healthcare providers in offering appropriate care and management strategies tailored to each individual's needs.
Causes and Symptoms
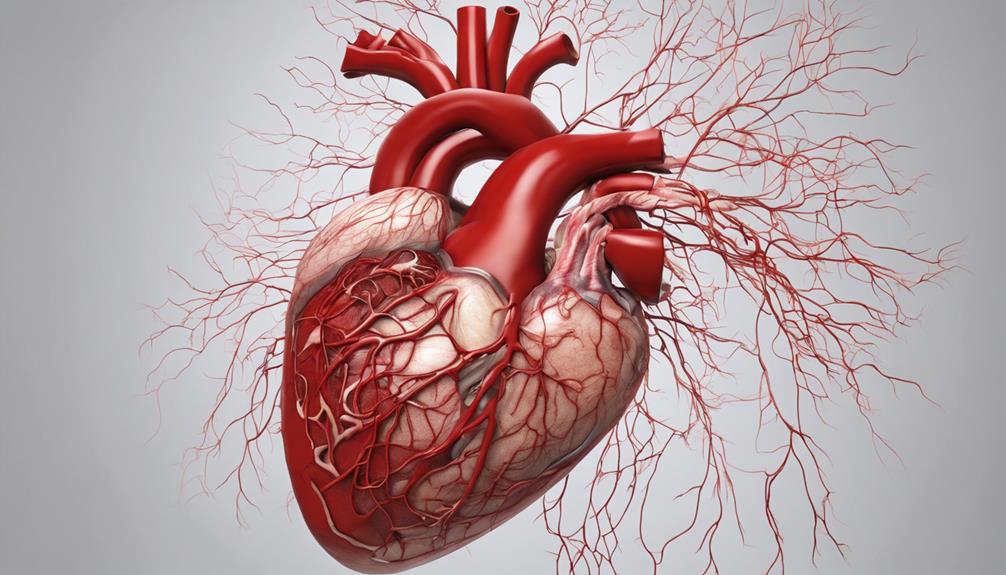
Moving from understanding the overview of microvascular heart disease, it's essential to delve into the specific causes and symptoms associated with this condition to facilitate accurate diagnosis and effective management strategies. Small vessel dysfunction in the coronary microvascular system can lead to a condition known as coronary microvascular disease. This dysfunction affects the flow of blood through the small arteries of the heart, resulting in symptoms that may be challenging to differentiate from other heart conditions.
- Causes of Microvascular Heart Disease:
- Diabetes
- High blood pressure
- High cholesterol
- Obesity
- Autoimmune diseases
- Symptoms of Microvascular Heart Disease:
- Angina lasting over 10 minutes
- Worsening chest pain with stress or exertion
- Fatigue
- Shortness of breath
- Sleep disturbances
Understanding these causes and symptoms is vital in helping individuals recognize the signs of non-obstructive coronary artery disease and seek appropriate medical help promptly to prevent complications.
Diagnosis and Testing
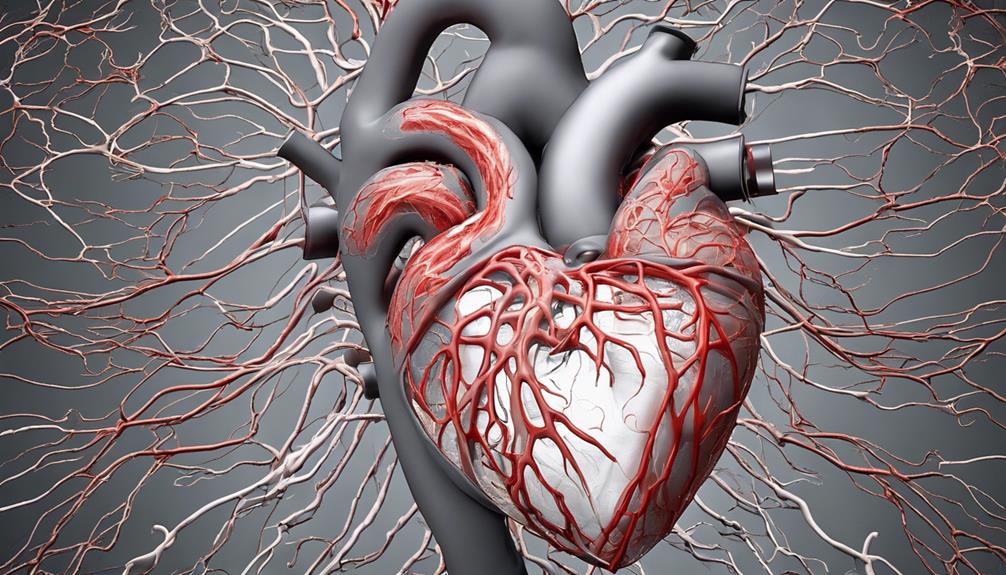
Diagnosis and testing for microvascular heart disease necessitate specialized cardiac assessments to evaluate small vessel function accurately. Utilizing diagnostic tools such as coronary flow reserve (CFR) during cardiac catheterization provides valuable insights into small vessel disease.
Additionally, nuclear cardiac stress tests and cardiac MRI with perfusion play crucial roles in assessing microvascular health. Expert interpretation of these results by a cardiologist specializing in small vessel disease is essential for an accurate diagnosis and effective treatment planning.
The intricate nature of microvessels underscores the importance of specific imaging methods to aid in diagnosis. Timely and precise evaluation through comprehensive testing is paramount for managing microvascular heart disease and enhancing outcomes.
Treatment Options

Exploring various treatment options is crucial for effectively managing microvascular heart disease and improving patient outcomes. When addressing this condition, a multidimensional approach is often necessary. Here are some key components of the treatment plan:
- Prescription Medications: These can be used to help open small blood vessels, improve coronary blood flow, and alleviate chest pain associated with microvascular heart disease.
- Lifestyle Modifications: Making lifestyle changes such as adopting a healthier diet and incorporating stress reduction techniques can play a significant role in managing symptoms and preventing further complications.
- Exercise Counseling: Recommendations for exercise tailored to individual needs can aid in symptom management and overall health improvement.
- Behavioral Support: Working with behavioral psychologists and specialists can assist in implementing lifestyle modifications and coping strategies to deal with the challenges of the condition.
- Regular Check-ins: Scheduled check-ins with healthcare providers are essential for monitoring progress, adjusting treatment plans as needed, and ensuring the effective management of microvascular heart disease.
Prevention and Outlook
Implementing lifestyle modifications and monitoring key risk factors are crucial steps in preventing microvascular heart disease and improving long-term outcomes. Lifestyle changes such as engaging in regular physical activity and following a heart-healthy diet can play a significant role in lowering the risk of developing microvascular heart disease. Additionally, keeping a close check on high blood pressure, high cholesterol levels, and managing diabetes through proper monitoring are essential in preventing the progression of this condition. Early intervention by healthcare professionals, along with regular medical screenings, can help identify any emerging risk factors promptly, allowing for timely management and prevention of complications. Smoking cessation and stress management techniques are also vital components in the prevention and control of microvascular heart disease. By adopting these preventive measures and addressing risk factors proactively, individuals can enhance their overall outlook, leading to an improved quality of life and reduced risk of adverse outcomes.
| Prevention | Risk Factors | Early Intervention |
|---|---|---|
| Lifestyle modifications | High blood pressure | Regular medical check-ups |
| Monitoring | High cholesterol | Timely management |
| Smoking cessation | Diabetes | Healthcare screenings |
Frequently Asked Questions
How Do You Treat Microvascular Disease in the Heart?
When treating heart disease, we tailor medication regimens to improve blood vessel function and reduce complications. Common medications include ACE inhibitors, anticoagulants, beta-blockers, calcium channel blockers, diuretics, and statins.
Specialized centers like Cleveland Clinic can provide personalized treatment plans. Effective management enhances symptom control and quality of life.
Regular follow-up care is crucial for monitoring treatment effectiveness and adjusting the plan as needed.
Can You Live Normal Life With Microvascular Angina?
Yes, we can live a normal life with microvascular angina. Proper management, including lifestyle adjustments, medication adherence, and regular medical follow-ups, can effectively control symptoms and enhance our quality of life.
Identifying triggers, managing risk factors, engaging in cardiac rehab programs, and following prescribed treatments are crucial steps for symptom relief and preventing complications.
With the right care and support, individuals can maintain an active and fulfilling lifestyle despite microvascular angina.
What Does Microvascular Angina Feel Like?
We feel microvascular angina as persistent chest pain triggered by stress or exertion. Symptoms include chest pressure, tightness, burning, or squeezing, often radiating to the neck, jaw, back, or arms.
Unlike traditional angina, it stems from small heart vessel dysfunction. People may also experience fatigue, shortness of breath, and sleep disturbances alongside chest pain. Accurate diagnosis via specialized tests is crucial to differentiate microvascular angina from other heart conditions and guide treatment.
What Are the New Treatments for Coronary Microvascular Disease?
We explore new treatments for coronary microvascular disease, including medications like endothelin receptor antagonists and ranolazine to enhance blood vessel function.
Angiotensin receptor-neprilysin inhibitors show promise in symptom management. Research delves into drugs targeting specific pathways to improve treatment efficacy.
Enhanced external counterpulsation is being studied for non-invasive blood flow enhancement.
Tailored medication and lifestyle changes are pivotal in addressing the unique needs of patients with microvascular heart disease.
Conclusion
In conclusion, microvascular heart disease poses a unique challenge due to its impact on the small blood vessels of the heart.
By understanding the causes, symptoms, and treatment options, individuals can take proactive steps towards managing this condition effectively.
Through lifestyle modifications, regular monitoring, and working closely with healthcare professionals, it's possible to navigate the complexities of microvascular heart disease and strive for a healthier heart.