Have you ever pondered whether Alzheimer’s and dementia are synonymous?
The distinction between these two conditions is crucial yet often misunderstood.
Understanding the nuances between Alzheimer’s and dementia can shed light on how we perceive and care for individuals affected by these cognitive disorders.
Let’s untangle the complexities and gain clarity on this important subject that impacts countless lives.
Key Takeaways
- Alzheimer’s is a specific form of dementia characterized by memory loss.
- Dementia encompasses a broader range of symptoms beyond memory loss.
- Understanding cognitive decline progression is vital for effective care.
- Treatment options include medications, therapy, lifestyle changes, and personalized plans.
Definition of Dementia
Dementia is a progressive neurological disorder that impairs cognitive function, including memory, reasoning, and decision-making skills. It’s crucial to understand that dementia isn’t a specific disease but rather a term used to describe a wide range of symptoms associated with a decline in mental abilities severe enough to interfere with daily life. These symptoms can vary depending on the underlying cause of dementia, which may include Alzheimer’s disease, vascular dementia, Lewy body dementia, or frontotemporal dementia.
Individuals with dementia may experience memory loss, confusion, difficulty with communication, and changes in mood or behavior. As caregivers, it’s essential to approach individuals with dementia with patience, empathy, and understanding. Providing a safe and structured environment, encouraging independence in daily activities, and promoting social engagement can help improve the quality of life for individuals living with dementia.
Being informed about the different types of dementia and their unique characteristics is crucial for offering appropriate care and support to those affected by this condition. By staying educated and remaining compassionate, we can make a positive impact on the lives of individuals living with dementia.
Characteristics of Alzheimer’s

Alzheimer’s disease manifests through a gradual onset of memory loss symptoms, primarily affecting short-term memory initially.
As the condition progresses, individuals may experience cognitive decline, impacting their ability to perform daily tasks and communicate effectively.
These characteristics are key identifiers in the diagnosis and management of Alzheimer’s disease.
Memory Loss Symptoms
In the early stages of this progressive neurodegenerative disease, individuals may experience difficulty recalling recent conversations and events. Memory loss symptoms in Alzheimer’s can progress from mild forgetfulness to severe impairment impacting daily life. Here is a table highlighting common memory loss symptoms seen in individuals with Alzheimer’s:
| Memory Loss Symptom | Description | Impact |
|---|---|---|
| Forgetfulness | Forgetting recently learned information | Difficulty in learning |
| Disorientation | Confusion about time, place, and situation | Trouble with navigation |
| Misplacing Items | Putting things in unusual spots | Disorganization |
These symptoms can be distressing for both the individual and their caregivers, highlighting the importance of early detection and support.
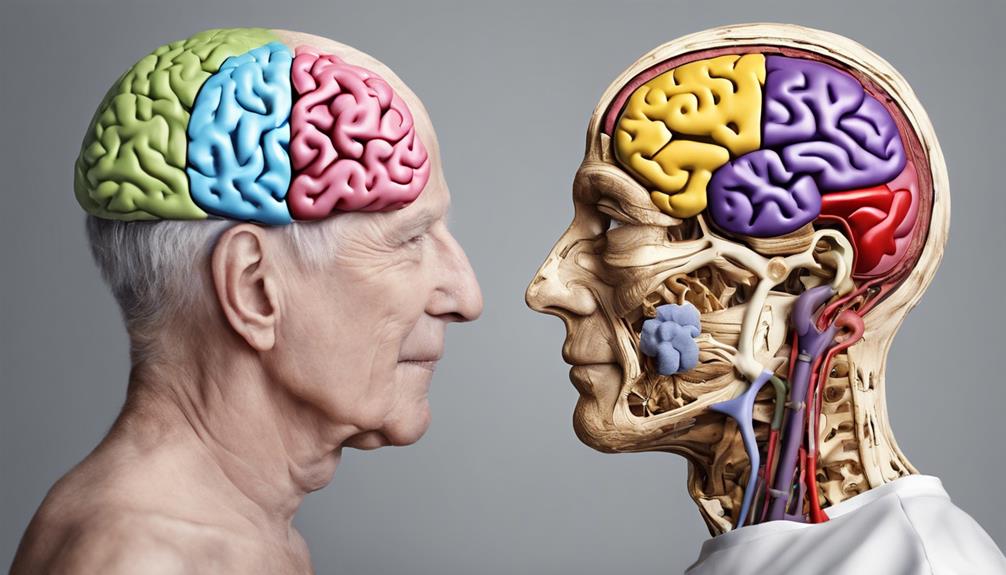
Cognitive Decline Progression
Charting the course of cognitive decline in Alzheimer’s disease reveals a complex interplay of neurobiological processes and behavioral manifestations. Initially, individuals may experience subtle memory lapses and difficulties with problem-solving.
As the disease progresses, these cognitive impairments worsen, impacting language, spatial awareness, and executive functions. Patients may struggle with daily activities, exhibit personality changes, and face challenges in recognizing loved ones.
Neurologically, the brain undergoes significant structural changes, with the accumulation of amyloid plaques and tau tangles contributing to cell death and synaptic dysfunction. Functional imaging studies show reduced brain metabolism and atrophy in key regions involved in memory and cognition.
Understanding this trajectory is crucial for providing appropriate care and support to individuals with Alzheimer’s disease.
Cognitive Decline in Dementia
Cognitive decline in dementia primarily manifests as a progressive deterioration in various mental processes, including memory, reasoning, and language skills. As dementia advances, individuals may experience difficulties in performing daily tasks, communicating effectively, and maintaining their independence. Below is a table illustrating the key cognitive changes seen in dementia:
| Cognitive Process | Description |
|---|---|
| Memory | Impairment in short-term and long-term memory retention |
| Reasoning | Challenges in problem-solving and decision-making |
| Language Skills | Difficulty in finding words, forming coherent sentences |
These cognitive impairments can significantly impact an individual’s quality of life, leading to increased dependency on caregivers and affecting social interactions. Understanding these cognitive changes is crucial for providing appropriate support and care to individuals living with dementia. By recognizing and addressing these challenges early on, healthcare professionals can help enhance the overall well-being of those affected by dementia.
Memory Loss in Alzheimer’s
Memory loss in Alzheimer’s disease presents as a gradual and persistent decline in both short-term and long-term memory capabilities. This deterioration in memory function can significantly impact daily life and cognitive abilities.
Here are three key points to consider:
- Progressive Nature: Alzheimer’s memory loss worsens over time, starting with mild forgetfulness and advancing to severe memory impairment. The decline is relentless and irreversible, affecting various aspects of memory retention and recall.
- Disorientation: Individuals with Alzheimer’s may struggle with orientation to time, place, and people due to memory loss. This disorientation can lead to confusion, agitation, and difficulty in recognizing familiar surroundings or faces.
- Memory Retrieval Issues: Retrieving stored memories becomes increasingly challenging as Alzheimer’s progresses. This difficulty extends beyond forgetting recent events to struggling with recalling past memories and information, causing frustration and distress.
Understanding these aspects of memory loss in Alzheimer’s disease is crucial for caregivers, healthcare professionals, and individuals affected by the condition. By recognizing the patterns and challenges associated with memory decline, appropriate support and interventions can be implemented to enhance the quality of life for those impacted by Alzheimer’s.
Behavioral Changes in Alzheimer’s

Consistently observed in individuals with Alzheimer’s disease, behavioral changes manifest as alterations in actions, emotions, and interactions, reflecting the progression of the condition. These changes often include agitation, irritability, apathy, anxiety, and in some cases, aggression. Individuals may exhibit repetitive behaviors, such as pacing or hand-wringing, and experience disturbances in sleep patterns. Social interactions can also be affected, leading to withdrawal from previously enjoyed activities and relationships. Additionally, individuals with Alzheimer’s may demonstrate changes in eating habits, showing preferences for certain foods or exhibiting a lack of interest in eating altogether.
Understanding and managing these behavioral changes is crucial in providing quality care for individuals with Alzheimer’s. Approaches such as maintaining a consistent routine, creating a calming environment, and engaging in meaningful activities can help alleviate some of these behaviors. It’s essential for caregivers and healthcare professionals to monitor these changes closely, as they can have a significant impact on the individual’s quality of life and overall well-being.
Causes of Dementia

One of the primary factors underlying the development of dementia is the progressive damage to brain cells that impairs cognitive function and memory retention. Dementia can have various causes, each affecting the brain in different ways.
Here are three key factors contributing to the onset of dementia:
- Neurodegenerative Diseases: Conditions like Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease can lead to the degeneration of brain cells, resulting in cognitive decline and memory loss.
- Vascular Issues: Stroke or small vessel disease can disrupt blood flow to the brain, depriving it of essential nutrients and oxygen, leading to cognitive impairment.
- Traumatic Brain Injury: Severe head injuries from accidents or falls can cause long-term damage to the brain, increasing the risk of developing dementia later in life.
Understanding these causes is crucial in diagnosing and managing dementia effectively, highlighting the importance of early intervention and preventive measures to mitigate its impact on individuals and their families.
Diagnosis of Alzheimer’s

Alzheimer’s disease diagnosis typically involves a comprehensive evaluation of cognitive function, medical history, and neurological assessments. The process aims to rule out other possible causes of symptoms and to provide an accurate diagnosis. A key aspect of diagnosing Alzheimer’s is the exclusion of reversible conditions that may mimic the disease. Below is an outline of the diagnostic criteria commonly used by healthcare professionals:
| Diagnostic Criteria | Description |
|---|---|
| Cognitive Assessment | Evaluates memory, language, problem-solving skills, and attention span. |
| Medical History | Reviews past and current medical conditions, medications, and family history of neurological diseases. |
| Neurological Examinations | Involves tests to assess reflexes, muscle strength, coordination, and sensory function. |
| Brain Imaging Studies | MRI or CT scans can help identify brain changes characteristic of Alzheimer’s disease. |
| Blood Tests | Checks for genetic markers, thyroid function, and vitamin deficiencies that could contribute to cognitive decline. |
These diagnostic tools, when used together, assist in accurately identifying Alzheimer’s disease and differentiating it from other forms of dementia. Early diagnosis is crucial for implementing appropriate care and support for individuals and their families.
Treatment Options for Dementia
After accurately identifying Alzheimer’s disease through comprehensive evaluation and diagnostic criteria, it’s essential to explore the various treatment options available for managing dementia.
- Medication: Prescription drugs such as cholinesterase inhibitors (donepezil, rivastigmine, galantamine) and memantine are commonly used to help manage symptoms and slow down the progression of dementia.
- Therapy: Cognitive stimulation therapy and reminiscence therapy have shown to be beneficial in improving cognitive function, memory, and overall quality of life for individuals with dementia.
- Lifestyle Changes: Encouraging physical exercise, a balanced diet, social engagement, and mental stimulation can significantly impact the progression of dementia and improve overall well-being.
It is crucial to work closely with healthcare professionals to create a personalized treatment plan tailored to the individual’s needs and stage of dementia. Regular monitoring and adjustments to the treatment plan may be necessary to ensure the best possible outcomes for those living with dementia.
Frequently Asked Questions
Can Dementia Be Prevented or Reversed?
Dementia prevention and reversal strategies focus on lifestyle modifications like:
- Regular physical exercise
- A balanced diet
- Cognitive stimulation
- Social engagement
These factors contribute to brain health and may help reduce the risk or slow the progression of dementia.
However, the effectiveness of these measures can vary depending on individual factors. Consult with healthcare professionals for personalized recommendations and interventions to support brain health and potentially mitigate the risk of developing dementia.
How Does Alzheimer’s Disease Affect a Person’s Emotional Well-Being?
Alzheimer’s disease impacts emotional well-being by causing mood swings, agitation, and changes in behavior. Individuals may experience confusion, anxiety, and frustration due to memory loss and cognitive decline.
As the disease progresses, feelings of sadness and isolation can worsen. Our understanding of these emotional challenges helps us provide compassionate care and support to those affected by Alzheimer’s, enhancing their quality of life and promoting emotional well-being.
Are There Any Alternative Treatments for Alzheimer’s Disease?
There are several alternative treatments being explored for Alzheimer’s disease. Some focus on reducing inflammation in the brain, while others aim to target abnormal protein build-up. Cognitive training, physical exercise, and dietary changes have shown promise in improving symptoms.
Clinical trials are also testing new medications that could potentially slow down the progression of the disease. Research in this field is ongoing, offering hope for the future of Alzheimer’s treatment.
Can Traumatic Brain Injury Increase the Risk of Developing Dementia?
Yes, traumatic brain injury can increase the risk of developing dementia. Research shows that individuals who’ve experienced a traumatic brain injury are more likely to develop various types of dementia, including Alzheimer’s disease.
The injury disrupts normal brain function and can lead to cognitive decline over time. Understanding this link is crucial for early detection and intervention strategies to mitigate the risk of dementia following a traumatic brain injury.
How Does Dementia Affect a Person’s Ability to Perform Daily Tasks Independently?
When dementia impairs daily tasks, we may struggle with basic activities like dressing, eating, and bathing. This decline in independence stems from cognitive and physical limitations.
Memory loss can hinder our ability to follow routines, while reduced coordination may make tasks like cooking hazardous. With dementia, maintaining independence becomes a challenge, requiring support and adaptations to ensure safety and quality of life.
Conclusion
In conclusion, while Alzheimer’s and dementia share similarities in symptoms and progression, the distinction lies in the underlying causes and specific cognitive impairments.
It’s ironic that despite advancements in medical research, the exact mechanisms of these conditions remain elusive.
As we continue to unravel the complexities of neurodegenerative diseases, it’s crucial to recognize the unique challenges each individual faces in their battle against memory loss and cognitive decline.