In healthcare, it is commonly believed that having knowledge is empowering.
When it comes to navigating the complexities of Alzheimer’s disease, understanding the ICD-10 code for this condition is crucial. It serves as a key that unlocks a world of information and resources, guiding us through the diagnostic criteria, common symptoms, and treatment options.
But what lies beyond just knowing the code? Stay tuned to uncover the nuances of coding challenges, reimbursement implications, and invaluable resources available for caregivers in the realm of Alzheimer’s care.
Key Takeaways
- ICD-10 coding crucial for accurate treatment decisions and compliance.
- Compliance necessary for proper compensation, financial sustainability, and ethical operations.
- Detailed documentation essential to ensure accurate code assignment and reimbursement.
- Utilize resources like Alzheimer’s Association for caregiving support and stress reduction.
Overview of Alzheimer’s Disease
Alzheimer’s disease affects millions of people worldwide, causing progressive cognitive decline and memory loss. It’s a challenging condition that not only impacts individuals but also places a significant burden on families and caregivers. As we navigate the complexities of this disease, understanding its effects is crucial in providing the best possible care and support.
Individuals with Alzheimer’s may experience a range of symptoms, including confusion, disorientation, and difficulty with everyday tasks. These challenges can lead to frustration and emotional distress for both the individual and their loved ones. Additionally, as the disease progresses, communication may become increasingly difficult, making it essential to approach interactions with patience and empathy.
Supporting those affected by Alzheimer’s requires a holistic approach that addresses physical, emotional, and social needs. By fostering a compassionate and understanding environment, we can help enhance the quality of life for individuals living with this condition. Together, we can make a difference in the lives of those impacted by Alzheimer’s disease.
Importance of ICD-10 Coding

ICD-10 coding accuracy benefits us by ensuring precise documentation of conditions, aiding in appropriate treatment decisions.
Compliance with reimbursement requirements is crucial for financial viability and ethical billing practices.
Facilitating disease tracking enhances research efforts and improves public health interventions.
Coding Accuracy Benefits
Understanding the importance of accurate ICD-10 coding is crucial for ensuring optimal healthcare outcomes and streamlined administrative processes. Precise coding helps healthcare providers in diagnosing conditions accurately, determining appropriate treatments, and tracking patient progress effectively.
With accurate ICD-10 codes, healthcare facilities can improve patient care by reducing errors in medical records and ensuring proper communication among healthcare team members. Additionally, precise coding facilitates data analysis, leading to better-informed decision-making processes and improved quality of care.
Reimbursement Compliance Requirements
Accurate ICD-10 coding plays a critical role in meeting reimbursement compliance requirements, ensuring healthcare facilities receive appropriate compensation for services rendered. Proper coding is essential for reimbursement claims to be processed efficiently and accurately.
By assigning the correct ICD-10 code for Alzheimer’s disease, healthcare providers can demonstrate the medical necessity of services provided to patients. This accurate documentation not only supports reimbursement claims but also helps in preventing claim denials or audits.
Compliance with ICD-10 coding guidelines is essential to avoid financial penalties and ensure that healthcare facilities operate ethically and within regulatory standards. Therefore, maintaining high standards of coding accuracy is vital for both financial sustainability and quality patient care.
Disease Tracking Facilitation
Maintaining precise disease tracking through effective ICD-10 coding is essential for healthcare facilities. Accurate coding allows for streamlined monitoring of diseases like Alzheimer’s, enabling healthcare providers to analyze trends, allocate resources efficiently, and improve patient outcomes.
With the right ICD-10 codes, we can track the progression of Alzheimer’s disease, assess the effectiveness of treatments, and identify any emerging patterns that may require attention.
Additionally, proper disease tracking facilitates collaboration among healthcare professionals, ensuring continuity of care and promoting evidence-based practices. By utilizing the ICD-10 coding system diligently, we uphold standards that ultimately benefit patients by enhancing the quality and coordination of healthcare services.
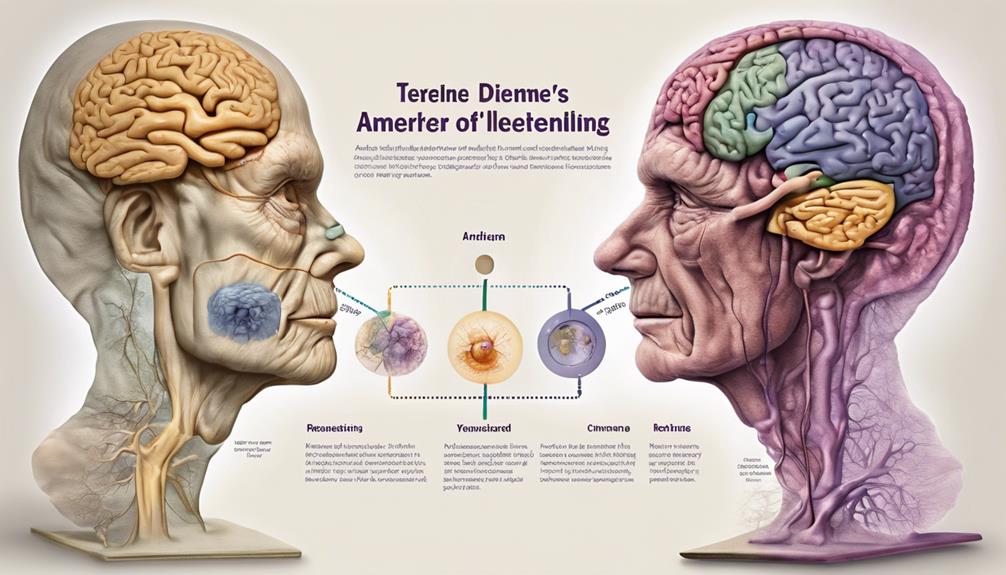
Diagnostic Criteria for Alzheimer’s
We’ll explore the early signs of Alzheimer’s, the role of neuroimaging in diagnosis, and the significance of biomarkers in identifying Alzheimer’s disease.
These points are crucial in understanding the diagnostic criteria for Alzheimer’s and can aid in early detection and intervention.
Early Signs of Alzheimer
Identifying early signs of Alzheimer’s through specific diagnostic criteria is crucial for timely intervention and management of the disease. Memory loss that disrupts daily life, challenges in planning or solving problems, difficulty completing familiar tasks, confusion with time or place, and changes in mood or personality are common early symptoms. These signs may be subtle initially, but over time, they can progress and impact a person’s quality of life significantly.
It’s essential to pay attention to these early indicators and seek medical evaluation if concerns arise. Early detection allows for early intervention, access to appropriate support services, and the opportunity to plan for the future. By recognizing these signs promptly, individuals can receive the necessary care and support to help manage the progression of Alzheimer’s disease.
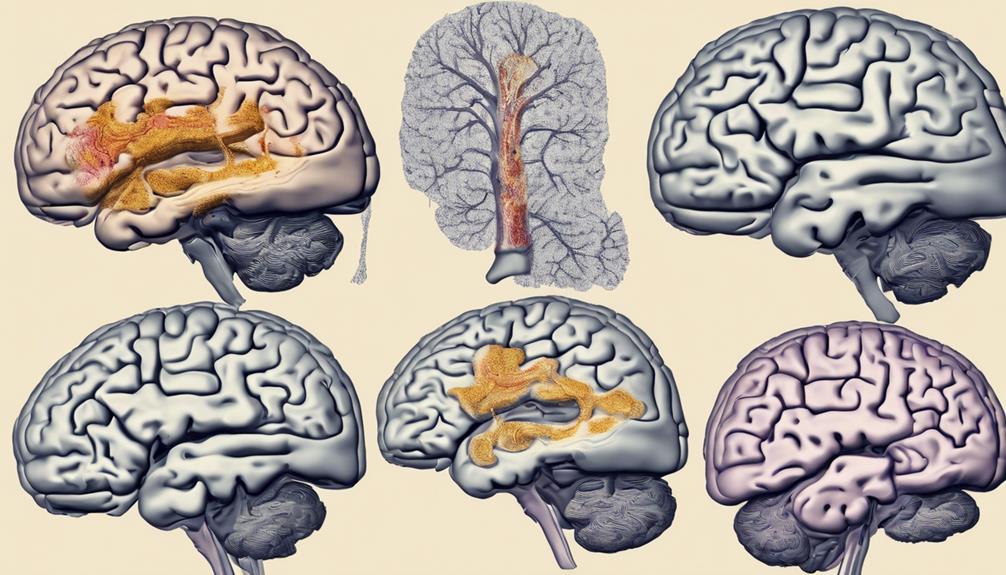
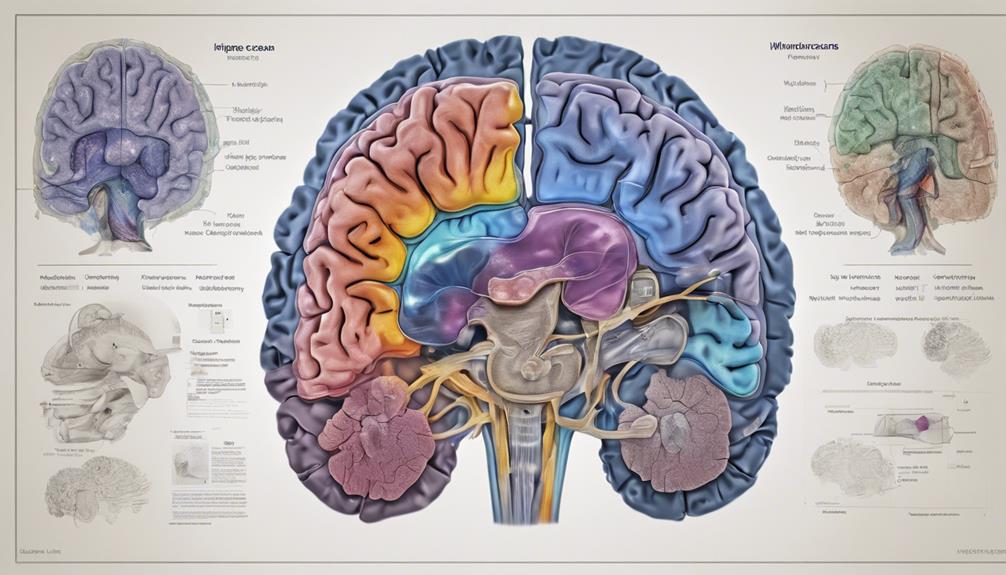
Neuroimaging in Diagnosis
Neuroimaging plays a pivotal role in the diagnostic criteria for Alzheimer’s disease, providing valuable insights into the structural and functional changes in the brain associated with this condition. Techniques such as magnetic resonance imaging (MRI), positron emission tomography (PET), and computed tomography (CT) scans can help detect brain atrophy, abnormal protein deposits, and changes in brain activity.
These imaging tools aid in ruling out other possible causes of cognitive decline and assist in making a more accurate diagnosis of Alzheimer’s. By visualizing the brain’s changes, neuroimaging contributes to the early detection and monitoring of the disease progression, allowing for timely interventions and personalized treatment plans to improve the quality of life for individuals affected by Alzheimer’s.
Biomarkers for Alzheimer’s
Alzheimer’s disease diagnostic criteria now incorporate biomarkers to enhance accuracy in early detection and monitoring of the condition. These biomarkers include beta-amyloid and tau proteins in cerebrospinal fluid, as well as amyloid PET imaging and tau PET imaging. By analyzing these biomarkers, healthcare providers can identify Alzheimer’s disease in its early stages, even before symptoms manifest.
This early detection allows for timely intervention and personalized treatment plans, ultimately improving patient outcomes. Biomarkers also play a crucial role in monitoring disease progression and response to treatment over time. Incorporating biomarkers into the diagnostic criteria for Alzheimer’s represents a significant advancement in the field, offering hope for better management of this challenging condition.
Common Symptoms and Progression
As symptoms of Alzheimer’s disease progress, individuals may experience a range of common cognitive and behavioral changes. These changes can be challenging for both the individual with Alzheimer’s and their caregivers. Here are some common symptoms and their progression that we may encounter:
- Memory Loss: Witnessing a loved one forget cherished memories can be heartbreaking.
- Confusion and Disorientation: Seeing someone you care for become confused about time or place can evoke feelings of helplessness.
- Personality Changes: Watching a once familiar personality shift due to Alzheimer’s can be emotionally taxing.
Navigating these symptoms and their progression requires patience, empathy, and understanding. It’s essential to provide support not only for the individual with Alzheimer’s but also for their caregivers who may find themselves overwhelmed. By raising awareness and offering assistance, we can help those affected by Alzheimer’s disease cope with these challenging changes.
Impact of Alzheimer’s on Patients

Throughout the progression of Alzheimer’s disease, patients often experience a profound impact on their daily functioning and quality of life. Simple tasks like remembering appointments or familiar faces can become increasingly challenging. As the disease advances, individuals may struggle with basic self-care activities such as dressing, bathing, or eating independently. This decline in cognitive abilities can lead to feelings of frustration, confusion, and fear in patients.
Alzheimer’s not only affects the individual diagnosed but also places a significant burden on their caregivers and loved ones. Family members may find themselves taking on more responsibilities to ensure the safety and well-being of the person with Alzheimer’s. The emotional toll of witnessing a loved one’s cognitive decline can be overwhelming and exhausting.
Furthermore, the financial impact of Alzheimer’s shouldn’t be underestimated. The cost of medical care, medications, home modifications, and long-term care services can quickly escalate, putting a strain on families and resources. Overall, Alzheimer’s disease profoundly impacts patients, their families, and the broader community, emphasizing the importance of early detection and compassionate care.
Treatment Options and Management
Progressing from the impact of Alzheimer’s on patients, exploring treatment options and management is essential in enhancing the quality of life for individuals affected by the disease. When it comes to addressing Alzheimer’s, we understand the importance of providing comprehensive care that caters to both the physical and emotional well-being of those impacted.
Here are a few key approaches that can make a significant difference:
- Person-Centered Care: Tailoring treatment plans to the individual’s unique needs and preferences fosters a sense of dignity and respect, promoting a more positive experience for both the individual and their caregivers.
- Support Networks: Building a strong support system that includes family, friends, and healthcare professionals can provide invaluable assistance and comfort throughout the journey.
- Holistic Approaches: Incorporating activities such as music therapy, art therapy, and mindfulness techniques can offer therapeutic benefits, improving quality of life and overall well-being.
Coding Challenges and Considerations
Navigating the complexities of assigning ICD-10 codes for Alzheimer’s disease presents several challenges and considerations. One significant challenge is the need for precise documentation to ensure accurate code assignment. Clinicians must thoroughly document the type and stage of Alzheimer’s, any associated behavioral symptoms, and any other relevant comorbidities. Another consideration is the importance of regular updates and reviews of the patient’s condition to reflect any changes in coding requirements.
Additionally, distinguishing between Alzheimer’s disease and other forms of dementia can be challenging but is crucial for proper coding. It’s essential to carefully review the diagnostic criteria and documentation to accurately assign the correct code. Another key consideration is the specificity required by ICD-10 coding guidelines. Using nonspecific codes can lead to claim denials or improper reimbursement, emphasizing the need for detailed and accurate coding.
Reimbursement and Insurance Coverage
To ensure appropriate reimbursement and insurance coverage for patients with Alzheimer’s disease, thorough documentation and accurate ICD-10 coding are essential. When dealing with reimbursement and insurance for Alzheimer’s care, the following key points should be considered:
- Advocacy: Engaging with insurance companies on behalf of patients to ensure they receive the coverage they deserve can be emotionally taxing but ultimately rewarding.
- Empathy: Understanding the financial burden Alzheimer’s care can place on families fosters a compassionate approach to navigating insurance complexities.
- Persistence: Continuously advocating for improved coverage and reimbursement policies helps in breaking down barriers that patients with Alzheimer’s face in accessing necessary care.
Resources for Alzheimer’s Caregivers

For caregivers of individuals with Alzheimer’s disease, accessing reliable and supportive resources is crucial for providing effective care and managing the challenges associated with the condition. It’s essential to have a strong support system in place to ensure the well-being of both the individual with Alzheimer’s and the caregiver. One valuable resource is the Alzheimer’s Association, which offers a range of services including support groups, educational materials, and a 24/7 helpline for immediate assistance.
Additionally, local community centers, hospitals, and senior care facilities often provide resources such as respite care programs, caregiver training workshops, and counseling services. These resources can help caregivers navigate the complexities of caring for someone with Alzheimer’s and prevent burnout.
Online platforms like the Family Caregiver Alliance and the National Institute on Aging also offer a wealth of information and tools to assist caregivers in understanding the disease, managing symptoms, and planning for the future. By utilizing these resources, caregivers can enhance their caregiving skills, reduce stress, and improve the quality of life for both themselves and their loved ones with Alzheimer’s.
Frequently Asked Questions
Are There Any Specific Genetic Tests or Screenings Recommended for Individuals at Risk for Alzheimer’s Disease?
Yes, there are specific genetic tests or screenings recommended for individuals at risk for Alzheimer’s disease. These tests can help identify genetic mutations associated with the disease and assess an individual’s risk level.
Early detection through genetic testing can provide valuable information for personalized healthcare planning and interventions. It’s important to consult with healthcare professionals to determine the most appropriate testing and screening options based on individual risk factors and family history.
How Does Alzheimer’s Disease Affect Different Age Groups, Such as Younger Onset Cases?
Alzheimer’s disease impacts various age groups differently, including younger onset cases. It can manifest in individuals under 65 and progress more rapidly in some cases.
Younger individuals may experience challenges in obtaining a timely diagnosis due to the misconception that Alzheimer’s only affects older adults. Early-onset cases often face unique emotional and financial burdens, highlighting the importance of raising awareness and providing support for individuals of all ages affected by this condition.
Are There Any Alternative or Complementary Therapies That Have Shown Promise in Managing Alzheimer’s Symptoms?
Absolutely, some alternative therapies like aromatherapy and music therapy have shown promise in managing Alzheimer’s symptoms. One fascinating statistic is that a study found that aromatherapy using essential oils like lavender can reduce agitation in individuals with Alzheimer’s.
These therapies can complement traditional treatments and improve quality of life. It’s essential to consult healthcare professionals before incorporating alternative therapies into a loved one’s care plan.
What Are Some Ways in Which Caregivers Can Cope With the Emotional and Physical Challenges of Caring for Someone With Alzheimer’s?
When caring for someone with Alzheimer’s, it is vital to prioritize self-care.
Engage in stress-relieving activities, seek support from community resources, and educate yourself about the disease.
Establish routines, communicate clearly, and maintain patience during challenging moments.
Delegate tasks, if possible, and remember to take breaks.
Additionally, staying organized and seeking respite care can provide much-needed relief.
How Does the Presence of Other Medical Conditions or Comorbidities Impact the Treatment and Management of Alzheimer’s Disease?
When other medical conditions or comorbidities are present, the treatment and management of Alzheimer’s disease can become more complex. These additional health issues may require adjustments to the treatment plan or medications used for Alzheimer’s.
Caregivers must work closely with healthcare providers to address all aspects of the individual’s health and ensure a comprehensive approach to managing Alzheimer’s alongside other conditions.
Conclusion
In conclusion, understanding the ICD-10 code for Alzheimer’s is crucial in accurately documenting and treating this complex disease.
As caregivers, we must navigate the challenges of coding and reimbursement to ensure proper care for our loved ones.
Just as Alzheimer’s slowly steals memories, let’s be vigilant in our efforts to fight back against its grasp with knowledge and compassion.









