We were intrigued to discover that between 25 to 50% of individuals with dementia encounter confabulation. As we delve further into this cognitive phenomenon, we are exploring its complex facets and implications for those affected.
The interplay between memory, perception, and reality in confabulation dementia presents a unique challenge that demands a nuanced approach. Join us as we unravel the intricacies of confabulation in dementia and delve into strategies for compassionate care and support.
Understanding Confabulation Dementia
Confabulation dementia, a phenomenon observed in various neurocognitive disorders, involves the inadvertent fabrication of false memories as a compensatory mechanism for cognitive deficits. False memories created through confabulation can be spontaneous and often reflect a blending of real past experiences with current perceptions. In conditions like Alzheimer's disease, frontotemporal dementia, and Korsakoff syndrome, where cognitive decline is prominent, individuals may resort to confabulations to maintain a sense of reality amidst memory loss.
Brain damage, particularly in regions like the frontal lobe or basal forebrain, is strongly associated with the occurrence of confabulation in dementia. These neural impairments disrupt the ability to distinguish between actual memories and fabricated ones, leading to the unintentional construction of false narratives. Understanding the underlying mechanisms of confabulation in dementia is crucial for providing appropriate care and support to affected individuals. By acknowledging the role of confabulation as a coping strategy for cognitive deficits, caregivers can adopt tailored approaches that validate the individual's experiences while maintaining a grounding in reality.
Causes and Risk Factors
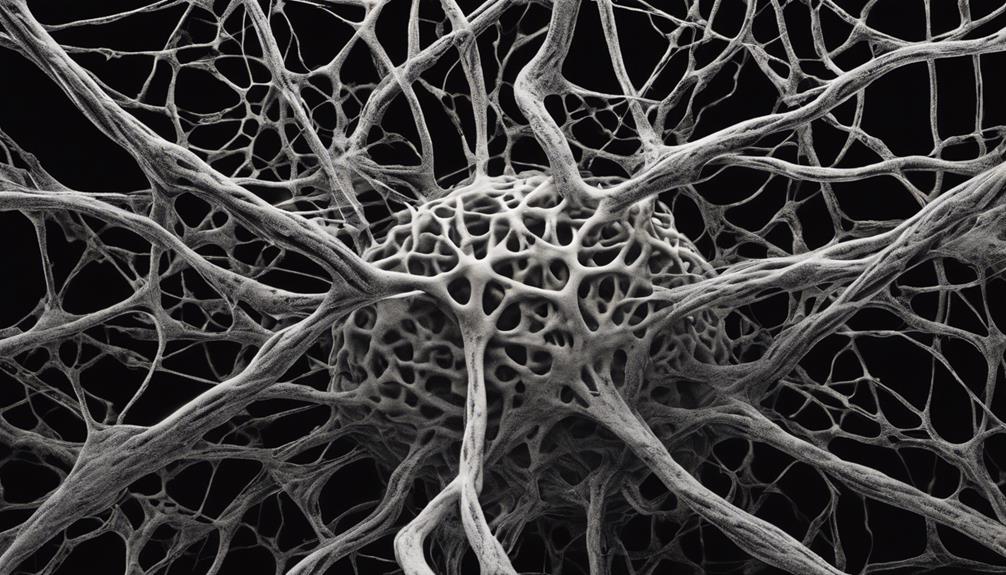
Brain damage in specific regions, such as the frontal and medial temporal lobes, commonly underlies the occurrence of confabulation in individuals with dementia. These regions play crucial roles in memory formation and retrieval. Memory gaps, often prevalent in dementia, can prompt the brain to fill in missing information, leading to the creation of false memories or confabulations. In Alzheimer's disease, over-learned information may dominate recall processes, further exacerbating confabulation. Additionally, the impaired function of the hippocampus, a brain region vital for memory consolidation, can increase the likelihood of confabulation in dementia patients.
Moreover, factors like delusions and aggression commonly seen in dementia can contribute to the development of confabulations. Distractions or difficulties in encoding new information can also prompt the generation of false memories in individuals with dementia. Understanding these causes and risk factors is crucial for caregivers and healthcare providers to effectively manage and support individuals experiencing confabulation in the context of dementia.
Differentiating Confabulation and Deception
In distinguishing between confabulation and deception, it is essential to recognize the fundamental disparities in the origins and nature of false memories versus intentional falsehoods. Confabulation arises from memory disturbances in conditions like dementia, leading to unintentional false memories that individuals genuinely believe. On the other hand, deception involves deliberate misrepresentation with conscious intent to mislead others, indicating a deliberate act of lying.
To aid in understanding the variances between confabulation and deception, the table below outlines key variations between these phenomena:
| Aspect | Confabulation | Deception |
|---|---|---|
| Intent | Unintentional | Deliberate misrepresentation |
| Awareness | Lack of awareness; belief in false memories | Conscious awareness of falsehoods |
| Origin | Memory disturbances in dementia | Conscious intent to mislead |
| Cognitive Implications | Symptom of cognitive impairment | Behavior driven by conscious decision-making |
| Belief in Falsehoods | Genuine belief in fabricated memories | Awareness of the falsehoods presented |
Understanding these distinctions is crucial for providing appropriate care and support for individuals experiencing confabulation in the context of dementia.
Managing Confabulation in Dementia

When managing confabulation in dementia, utilizing the validation method to address underlying emotions is a key strategy for providing effective care and support. The validation method acknowledges the individual's feelings and experiences, fostering a sense of understanding and respect.
Caregivers should prioritize creating a supportive environment where individuals feel heard and validated, avoiding the temptation to argue or disprove false memories. Instead, after validating emotions, redirecting or distracting conversations can help manage confabulation episodes effectively. This approach helps individuals feel valued and supported, reducing distress and confusion associated with false memories.
Emotional List:
- Demonstrating empathy and understanding can help individuals feel validated and respected.
- Creating a safe and supportive environment is crucial for managing confabulation with sensitivity.
- Using individualized approaches tailored to the person's needs shows a commitment to providing personalized care.
Supportive Care Strategies
To effectively support individuals experiencing confabulation in dementia, implementing tailored and empathetic care strategies is paramount in addressing their emotional needs. The validation method proves crucial in acknowledging and attending to the feelings of those struggling with confabulation. By validating their false memories and then gently shifting conversations or providing distractions, individuals can be guided to focus on the present moment, reducing distress.
Engaging individuals in activities they enjoy can redirect their attention away from confabulated memories, promoting a sense of well-being and fulfillment. Demonstrating patience and understanding during episodes of confabulation is essential in creating a supportive environment that fosters trust and comfort. Seeking guidance from healthcare professionals for personalized strategies ensures that the care provided is effective and tailored to the individual's specific needs.
Frequently Asked Questions
What Are Signs That Dementia Is Getting Worse?
As dementia progresses, signs indicating worsening may include increased forgetfulness, declined cognitive abilities, mood and behavioral changes, and difficulties with daily tasks.
Physical symptoms like mobility issues and coordination problems can also become more pronounced.
These indicators serve as important checkpoints for monitoring the progression of dementia and can guide caregivers and healthcare professionals in adjusting care plans and support strategies for individuals experiencing these changes.
What Stage of Dementia Is Sundowning?
In the middle to late stages of dementia, such as Alzheimer's disease, sundowning typically occurs. It's characterized by increased confusion, agitation, and behavioral disturbances in the late afternoon or evening.
Factors like fatigue, reduced lighting, and increased shadows can trigger or worsen sundowning episodes. Managing sundowning involves creating a calming environment, maintaining a consistent routine, and ensuring proper sleep hygiene.
What Are 3 Things to Never Do With Your Loved One With Dementia?
When caring for a loved one with dementia, it's essential to approach the situation with empathy and understanding. This means refraining from arguing or belittling their false memories, dismissing their confabulations, or challenging their reality. Instead, we should focus on validating their emotions, acknowledging their feelings, and providing comfort. By creating a supportive and understanding environment, we can help our loved ones feel respected and cared for during their difficult journey with dementia.
What Are the End Stages of Dementia?
In the end stages of dementia, individuals experience severe cognitive decline, loss of independence, and increased physical frailty. Communication becomes extremely challenging, and basic daily tasks are no longer manageable.
Behavioral symptoms may escalate, leading to agitation and aggression. Caregivers are essential during this time, providing comfort, pain management, and support.
Hospice and palliative care services become crucial to ensure the best possible quality of life for those nearing the end of their dementia journey.
Is Confabulation a Common Symptom of Dementia-Related Seizures?
Yes, confabulation is a common symptom of dementia-related seizures according to a managing dementiarelated seizures article. Confabulation is the production of fabricated, distorted, or misinterpreted memories about oneself or the world, without the conscious intention to deceive. This symptom can be quite challenging to manage for caregivers.
Conclusion
In conclusion, navigating the complexities of confabulation dementia requires a nuanced approach that prioritizes empathy and understanding.
By embracing the idiom 'walking a mile in someone else's shoes,' we can better appreciate the subjective experiences of individuals with this condition.
Through tailored supportive care strategies and a compassionate mindset, we can enhance the quality of life for those affected by confabulation dementia.








