When discussing the progression of vascular dementia, it is common for people to categorize it into three distinct stages – mild, moderate, and severe.
But what exactly do these stages entail, and how do they impact individuals and their loved ones?
Let's explore the intricate journey through these stages and unravel the complexities of vascular dementia progression, shedding light on the challenges faced and the necessary support systems required to navigate this intricate path alongside those affected by this condition.
Key Takeaways
- Early stage: Mild confusion, memory changes, safety concerns, gradual cognitive decline
- Moderate stage: Memory loss, mood changes, need for structured support
- Severe stage: Profound loss of independence, communication difficulties, focus on comfort
- Support systems: Vigilance, structured environment, comprehensive assistance, involvement of caregivers
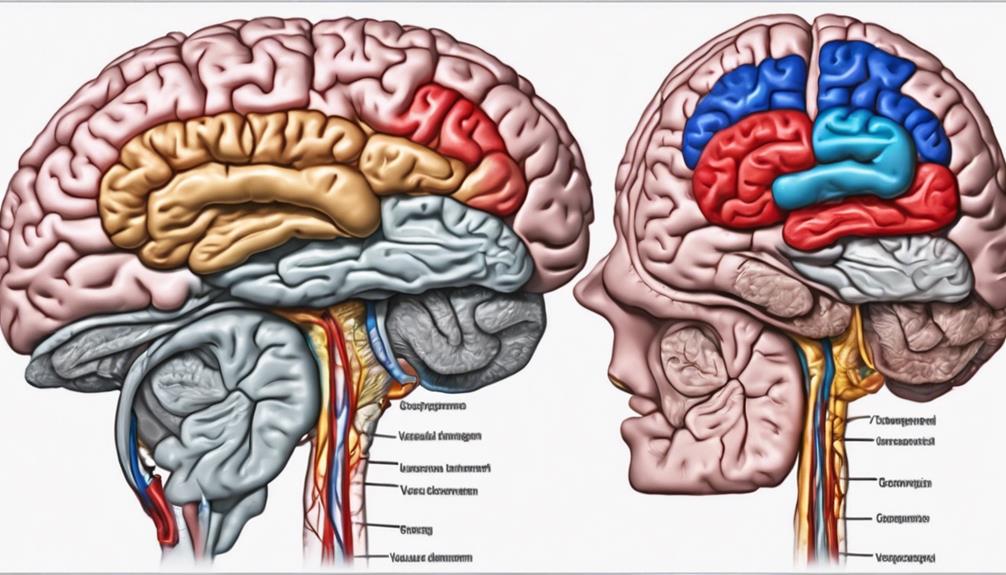
Early Mild Cognitive Impairment Stage
During the early mild cognitive impairment stage of vascular dementia, individuals may exhibit mild confusion and difficulties with problem-solving. This phase is marked by noticeable changes in memory and thinking abilities, which can significantly impact daily functioning.
Family and friends may begin to observe a gradual cognitive decline during this stage, prompting them to seek support for their loved ones. Symptoms like slowed thinking, forgetfulness, and confusion become more pronounced as individuals navigate through this initial phase of cognitive impairment.
Safety concerns may also arise as individuals in this stage may find it challenging to remember important information, make decisions, and perform cognitive tasks effectively. It's crucial for caregivers and healthcare professionals to be vigilant during this stage, offering necessary support and interventions to enhance the quality of life for those experiencing early mild cognitive impairment due to vascular dementia.
Moderate Cognitive Decline Stage
In the moderate cognitive decline stage of vascular dementia, individuals typically experience a range of prominent symptoms that significantly impact their cognitive abilities. This stage is characterized by:
- Memory Loss: Memory impairments become more evident, affecting daily functioning and increasing the need for supervision.
- Changes in Mood and Social Withdrawal: Individuals may exhibit shifts in mood and withdraw from social interactions more frequently as cognitive decline progresses.
- Cognitive Challenges: New cognitive difficulties emerge, making it challenging for individuals to perform complex tasks and maintain cognitive functions.
- Safety Concerns: Safety becomes a paramount issue due to the risk of wandering and the occurrence of sundown syndrome, necessitating increased supervision and support in daily activities.
During this stage, it's crucial to provide a structured environment, ensure safety measures are in place, and offer appropriate support to help individuals with vascular dementia cope with the cognitive decline and maintain their quality of life.
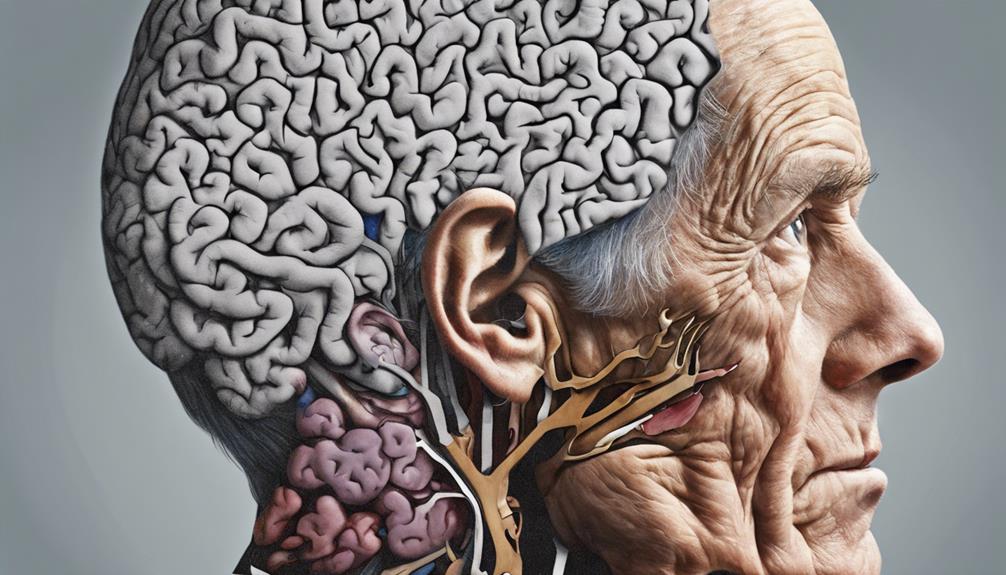
Severe Daily Functional Impairment Stage
Transitioning from the moderate cognitive decline stage, individuals in the severe daily functional impairment stage of vascular dementia exhibit a profound loss of independence in performing essential daily activities. At this advanced stage, severe cognitive decline leads to significant daily functional impairment, necessitating constant supervision and assistance with basic tasks such as grooming, eating, and mobility.
Communication difficulties become more pronounced, complicating interactions with caregivers and healthcare providers. Behavioral changes, including agitation and aggression, may surface, adding to the complexity of care. Ensuring the quality of life for individuals in this stage becomes paramount, with a focus on providing comfort, safety, and dignity.
Caregivers and healthcare professionals play a crucial role in supporting individuals with vascular dementia through this challenging phase, offering comprehensive assistance and compassionate care to maintain the highest possible level of functioning and well-being.
Frequently Asked Questions
What Stage Is Vascular Dementia Severe?
In vascular dementia, the severe stage is typically categorized as stage 6 or 7 in the progression. This stage signifies a significant cognitive decline, memory loss, and challenges with daily activities. Individuals may experience symptoms like agitation, personality changes, and an increased need for supervision and care.
Speech, mobility, and basic self-care tasks become increasingly difficult, requiring extensive support. Late severe vascular dementia entails severe limitations in communication, mobility, and cognitive function, necessitating comprehensive care and specialized interventions.
What Is the Longest You Can Live With Vascular Dementia?
Living with vascular dementia can vary in duration, influenced by factors like overall health and treatment response. It's crucial to address risk factors and provide effective care to potentially extend life expectancy.
Some individuals may live over a decade with vascular dementia, but progression impacts outcomes. Complications such as strokes or heart attacks can affect longevity.
Quality care, lifestyle adjustments, and treating health issues can significantly impact how long individuals survive with vascular dementia.
What Are the Signs That Vascular Dementia Is Getting Worse?
As signs of vascular dementia worsen, increased memory loss, difficulty with daily tasks, changes in behavior, decline in communication, and physical symptoms like poor coordination can indicate progression.
These symptoms may suggest an escalation in the severity of the condition and the need for additional support and care.
Recognizing these signs promptly and seeking appropriate medical guidance is crucial in managing the challenges associated with worsening vascular dementia.
Can Vascular Dementia Deteriorate Quickly?
Yes, vascular dementia can deteriorate quickly. The speed of decline varies based on factors like the extent of brain damage and overall health. Early detection and proper care can help slow down this progression.
Monitoring cognitive changes, lifestyle adjustments, and appropriate interventions are crucial for managing and potentially slowing down rapid deterioration in vascular dementia. Early intervention is key in mitigating the quick decline associated with this condition.
Conclusion
In conclusion, the three stages of vascular dementia progression – mild, moderate, and severe – each present unique challenges and require tailored care.
It's important to note that vascular dementia is the second most common type of dementia after Alzheimer's disease, accounting for approximately 10% of cases.
Understanding the progression of this condition is crucial in providing appropriate support and improving quality of life for individuals affected by vascular dementia.