The progression of frontotemporal dementia spans over seven stages, highlighting significant shifts in cognitive abilities and behaviors. Starting with subtle alterations and progressing to profound cognitive deterioration, these stages depict a relentless and gradual progression.
Understanding the nuances of each stage is crucial for caregivers and healthcare professionals to navigate the complexities of this condition effectively. Let's explore the intricacies of these stages and the impact they have on individuals and their loved ones.
Key Takeaways
- Early cognitive changes include memory issues and communication challenges.
- Behavioral shifts may lead to risky choices and social inappropriateness.
- Language impairments in FTD involve difficulties with speech production and comprehension.
- Personality alterations can result in disinhibition, apathy, and loss of empathy.
Early Cognitive Changes
In the early stages of frontotemporal dementia, individuals may exhibit subtle memory issues and mild behavioral alterations, signaling the onset of cognitive changes. Memory problems can manifest as forgetfulness about recent events or difficulty recalling names. Alongside this, planning difficulties and struggles in organizing tasks become noticeable. Tasks that once seemed straightforward may now pose challenges, leading to frustration and irritability. Social behavior changes are also apparent, with some individuals showing reduced empathy or engaging in socially inappropriate actions.
Communication challenges are another hallmark of these early cognitive changes. Word-finding difficulties can make conversations disjointed, while speech issues may include hesitations or trouble articulating thoughts clearly. These disruptions in communication can be distressing for both the individual experiencing them and their loved ones.
These early cognitive changes represent the initial phase of the progressive decline seen in frontotemporal dementia, highlighting the importance of early detection and intervention to support individuals facing these challenges.
Behavioral Shifts and Alertness
Transitioning from the early cognitive changes of frontotemporal dementia, behavioral shifts and alertness become prominent factors that significantly impact the individual's social interactions and daily functioning. In individuals with frontotemporal dementia, the following aspects characterize behavioral shifts and alertness:
- Lack of Judgment: Impaired decision-making abilities leading to risky choices and inappropriate actions.
- Inappropriate Social Behaviors: Displaying socially unacceptable actions or comments due to a lack of inhibition.
- Loss of Empathy: Difficulty understanding others' emotions and reduced ability to connect emotionally.
- Impulsive Actions: Engaging in sudden, unplanned behaviors without consideration of consequences.
These changes in behavior and alertness can strain relationships, disrupt work environments, and hinder daily activities. Caregivers and healthcare professionals play a crucial role in managing these shifts by providing structured routines, implementing safety measures, and offering support tailored to the individual's needs.
Understanding the complexities of behavioral alterations and alertness fluctuations is fundamental in ensuring a compassionate and effective approach to caring for individuals experiencing frontotemporal dementia.
Language Impairments
Language impairments in frontotemporal dementia present a complex array of challenges, with primary progressive aphasia being a common manifestation affecting both speech production and comprehension. Difficulties with word retrieval, articulation, and understanding spoken language are prevalent, highlighting the diverse nature of linguistic deficits in FTD.
Variants such as semantic variant PPA, impacting word meaning, and nonfluent variant PPA, affecting speech fluency, underscore the nuanced ways in which language abilities can be compromised in this neurodegenerative condition.
Speech Difficulties in FTD
Amidst the progression of Frontotemporal Dementia (FTD), individuals often encounter significant challenges with articulating words, finding appropriate vocabulary, and maintaining speech clarity, all contributing to notable language impairments. These speech difficulties in FTD present in various ways:
- Articulation Problems: FTD can result in difficulties forming sounds and pronouncing words accurately.
- Word-Finding Challenges: Individuals may struggle to retrieve the right words to express their thoughts.
- Reduced Speech Clarity: Speech may become slurred or unclear, affecting communication.
- Impact on Social Interactions: Language impairments can lead to frustration and isolation as individuals find it challenging to engage in conversations effectively.
Speech therapy and supportive communication techniques play crucial roles in managing these language impairments for individuals with FTD.
Semantic Dementia Characteristics
Significant language impairments characterize semantic dementia, a subtype of frontotemporal dementia, manifesting in difficulties with word understanding, object recognition, and concept comprehension.
Individuals with semantic dementia often experience vocabulary loss, comprehension deficits, and struggle with recognizing familiar faces. This form of dementia primarily affects the left temporal lobe, impacting semantic memory and language processing.
One hallmark of semantic dementia is the presence of fluent but empty speech, where individuals may speak effortlessly but with little meaningful content. Naming difficulties and semantic paraphasias, where incorrect words are used unintentionally, are also common in this condition.
Understanding these language impairments is crucial for providing appropriate care and support to individuals living with semantic dementia.
Impact on Quality of Life
As individuals progress through the 'Implications of Quality of Life' stage in frontotemporal dementia, our daily living challenges intensify, impacting our ability to maintain personal hygiene, manage finances, and engage in social interactions.
The decline in cognitive and behavioral functioning during this stage significantly affects our quality of life, leading to difficulties in communication, decision-making, and emotional regulation.
Caregivers also face heightened burden and stress as they provide extensive support to meet our daily needs and well-being requirements.
Daily Living Challenges
Facing daily living challenges due to frontotemporal dementia can profoundly impact the quality of life for both individuals with the condition and their caregivers. These challenges include:
- Struggles with Daily Activities: Individuals may find it challenging to perform tasks like dressing, bathing, or cooking independently.
- Difficulty Managing Personal Care: Maintaining personal hygiene and grooming routines can become increasingly hard as cognitive decline progresses.
- Challenges in Communication: Changes in language skills can lead to difficulties in expressing thoughts and understanding others.
- Changes in Behavior: Emotional and behavioral changes such as apathy, impulsivity, or aggression can make interactions and daily living more complex.
Social Interactions Affected
Social interactions in individuals with frontotemporal dementia are markedly influenced, presenting challenges in maintaining relationships and engaging with others due to the impact on quality of life as the disease progresses. The table below highlights the key aspects affecting social interactions in frontotemporal dementia:
| Challenges | Impact on Individuals | Consequences |
|---|---|---|
| Inappropriate behaviors | Difficulty in social situations | Strained relationships |
| Reduced empathy | Lack of understanding of others' emotions | Emotional disconnection |
| Social withdrawal | Isolation from social activities | Loneliness and alienation |
These manifestations can lead to dependency on caregivers, disruptions in daily living, and significant isolation, further deteriorating the individual's quality of life.
Personality Alterations and Mood Swings
Personality alterations and mood swings are prominent features of frontotemporal dementia, characterized by disinhibition, apathy, and intense emotional fluctuations that can impact social interactions and relationships. These changes can be challenging to manage and may require specialized care. Here are some key points to consider:
- Disinhibition: Individuals with frontotemporal dementia may exhibit a lack of restraint in social situations, leading to impulsive actions or inappropriate comments.
- Apathy: Patients may show decreased interest in activities they once enjoyed, along with a general lack of motivation or initiative.
- Loss of Empathy: Empathetic responses towards others may diminish, affecting their ability to understand or share the feelings of those around them.
- Socially Inappropriate Behaviors: Due to frontal lobe dysfunction, individuals may engage in behaviors that are considered socially unacceptable or out of character.
Understanding these aspects of personality alterations and mood swings is vital for caregivers and healthcare professionals to provide effective support and enhance the quality of life for those with frontotemporal dementia.
Progressive Memory Decline
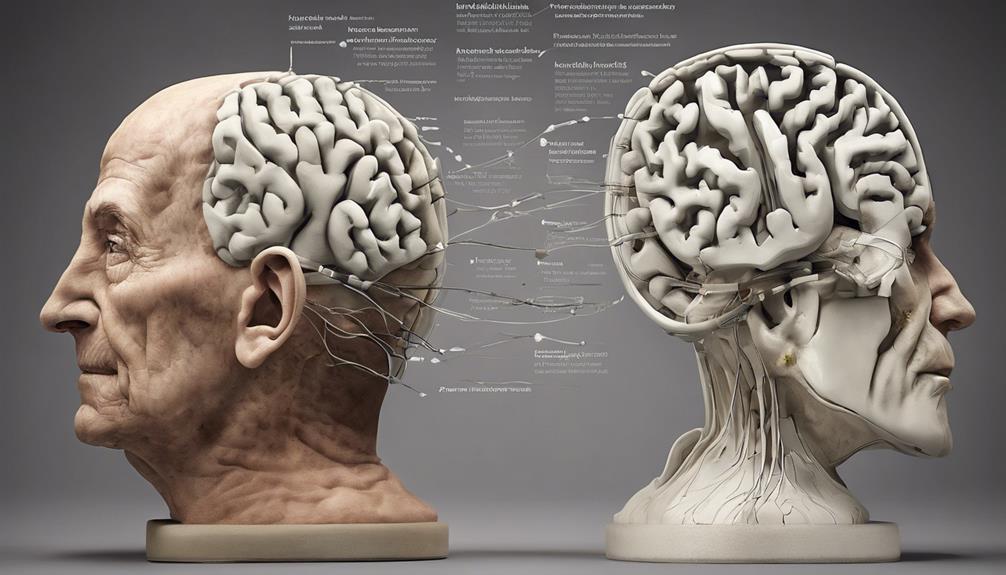
During the progression of frontotemporal dementia, the decline in memory function gradually becomes more pronounced, significantly impacting daily activities and cognitive abilities. Memory loss may not be a prominent feature in the early stages, but as the disease advances, memory deterioration becomes more noticeable. Individuals may struggle with remembering recent events, names, or important details. In the middle stages of frontotemporal dementia, memory problems worsen, requiring increased assistance and support from caregivers. Simple tasks such as following a routine or recalling familiar faces can become challenging. Memory decline in this stage significantly affects functioning, making it difficult for individuals to maintain their independence in daily activities. Severe cognitive impairment in the late stages includes profound memory loss and challenges with decision-making, further highlighting the progressive nature of the disease. Below is a table outlining the key aspects of memory decline in frontotemporal dementia:
| Memory Decline in Frontotemporal Dementia | |
|---|---|
| Early Stages | Memory loss may not be prominent |
| Middle Stages | Memory problems worsen, requiring increased assistance |
| Late Stages | Severe cognitive impairment includes significant memory loss and challenges with decision-making |
| Impact | Memory decline significantly impacts daily activities and functioning |
Severe Cognitive Deterioration
As frontotemporal dementia progresses, individuals experiencing severe cognitive deterioration exhibit profound memory loss and significant decline in cognitive function, necessitating extensive assistance and care. In this stage of the disease, several key characteristics become prominent:
- Basic Activities of Daily Living: Individuals may struggle with tasks like dressing, bathing, and eating independently.
- Communication Difficulties: Speech, language, and comprehension skills deteriorate, leading to challenges in expressing thoughts and understanding others.
- Behavioral Changes: Behavioral symptoms such as aggression, agitation, and wandering can escalate, requiring specialized interventions to manage.
- 24-Hour Care: Due to the severity of cognitive impairment, round-the-clock supervision and support become essential to ensure the individual's safety and well-being.
In this stage, the individual's cognitive abilities decline significantly, impacting their daily functioning and necessitating comprehensive care and assistance. Family members and caregivers play a crucial role in providing the necessary support and ensuring the individual's quality of life amidst the challenges posed by severe cognitive deterioration.
Frequently Asked Questions
How Fast Does Frontotemporal Dementia Progress?
Frontotemporal dementia can progress at varying rates, with some individuals experiencing rapid decline. Factors like age, overall health, and genetic predisposition influence the speed of progression.
Early stages may involve subtle changes, while later stages show severe cognitive impairment. Monitoring symptoms closely and seeking medical advice promptly are crucial in managing the disease's progression.
It's essential to understand the individualized nature of frontotemporal dementia progression to provide appropriate care and support.
What Is the Last Stage of Frontal Lobe Dementia?
In the last stage of frontotemporal dementia, severe cognitive impairment and profound memory loss are prominent. Individuals may require constant care due to mobility challenges and impaired decision-making abilities. Memory decline in this final stage mirrors symptoms observed in advanced Alzheimer's disease.
Moreover, end-stage frontotemporal dementia escalates the risk of infections like pneumonia, further complicating health issues. This stage underscores the disease's substantial impact on cognitive function, behavior, and overall quality of life.
What Are 5 Extreme Behavior Changes Found With Ftd?
In Frontotemporal Dementia (FTD), five extreme behavior changes include:
- Lack of judgment
- Decreased inhibitions
- Inappropriate social behaviors
- Loss of empathy
- Reduced interest in activities
These changes can lead to social inappropriateness, challenges in relationships, impulsive behaviors, emotional outbursts, and difficulty in understanding social cues.
Understanding and managing these behaviors are crucial to support individuals with FTD and enhance their quality of life.
How Long Does Someone With Frontal Lobe Dementia Live?
Living with frontal lobe dementia presents challenges, and the lifespan can vary. Factors such as age, health, and FTD subtype influence longevity.
Caregiver support, medical care, and a nurturing environment play key roles in enhancing well-being and lifespan. Monitoring symptoms and addressing needs promptly are crucial.
Together, we must strive to provide the best possible care to promote a fulfilling life for those with frontotemporal dementia.
Conclusion
In conclusion, the seven stages of frontotemporal dementia represent a journey through the changing landscape of cognitive decline and behavioral challenges. Like a winding road through a foggy forest, each stage presents new obstacles and twists, gradually leading towards a destination of severe cognitive impairment.
It's crucial to navigate this path with awareness and support, ensuring the best possible outcomes for individuals affected by this complex condition.