Vascular dementia advances through seven unique stages, each presenting varying degrees of cognitive deterioration. As individuals transition from the first stage of ‘No Impairment’ to the last stage of ‘Late Severe Dementia,’ the difficulties and signs they experience undergo significant changes.
Understanding these stages can provide insights into the journey individuals with vascular dementia go through, shedding light on the complexities of this condition. Stay tuned to uncover the nuanced characteristics of each stage and the implications they hold for those affected by this form of dementia.
Normal Behavior
In the first stage of vascular dementia, individuals maintain normal cognitive functioning without any impairment. This initial phase is characterized by the absence of memory issues, noticeable cognitive impairment, or confusion. During this early stage, cognitive abilities remain intact, and there are no signs of forgetfulness. Normal behavior is sustained, marking the starting point before any cognitive decline becomes evident.
It's crucial to monitor cognitive functioning closely during this period to detect any subtle changes that may indicate the progression of vascular dementia. At this stage, individuals may not exhibit any significant symptoms, but healthcare providers should conduct thorough assessments to establish a baseline for comparison as the condition advances.
Understanding the normal behavior and cognitive abilities at this point is essential for recognizing deviations from the baseline in subsequent stages of vascular dementia. By closely observing cognitive functioning in the absence of any impairments, healthcare professionals can provide appropriate support and care tailored to the individual's needs.
Very Mild Cognitive Decline
At the outset of very mild cognitive decline in vascular dementia, individuals typically maintain normal memory function and exhibit no noticeable signs of cognitive impairment. This initial stage is characterized by the absence of memory problems or confusion, allowing individuals to continue their daily activities without significant impact. Despite the subtle nature of cognitive decline at this stage, it's essential to monitor any changes in memory function or cognitive abilities over time. While memory loss may progress slowly, it's crucial to stay vigilant for any signs of advancement to the next stage of vascular dementia.
During very mild cognitive decline, individuals may not even be aware of the subtle changes happening within their cognitive abilities. Family members and caregivers play a crucial role in observing and documenting any deviations from normal behavior. By maintaining open communication with healthcare professionals and staying proactive in monitoring cognitive function, early interventions and support can be implemented to help individuals maintain their quality of life for as long as possible.
Mild Cognitive Decline
Moving from the initial stage of very mild cognitive decline, individuals entering the third stage of vascular dementia, known as mild cognitive decline, may begin to experience noticeable memory problems and cognitive issues. Symptoms of mild cognitive decline include forgetfulness, difficulty concentrating, and mild confusion. These challenges mark the early onset of cognitive decline, impacting daily activities such as managing finances or following a recipe.
In this stage, early intervention becomes crucial. Support strategies like establishing routines, using memory aids, and simplifying tasks can help individuals cope with the symptoms and maintain a certain level of independence. Encouraging regular physical exercise and social engagement may also contribute to cognitive function.
It's essential for caregivers and healthcare providers to monitor changes, provide emotional support, and adapt care plans as needed to enhance the quality of life for those experiencing mild cognitive decline.
Moderate Cognitive Decline
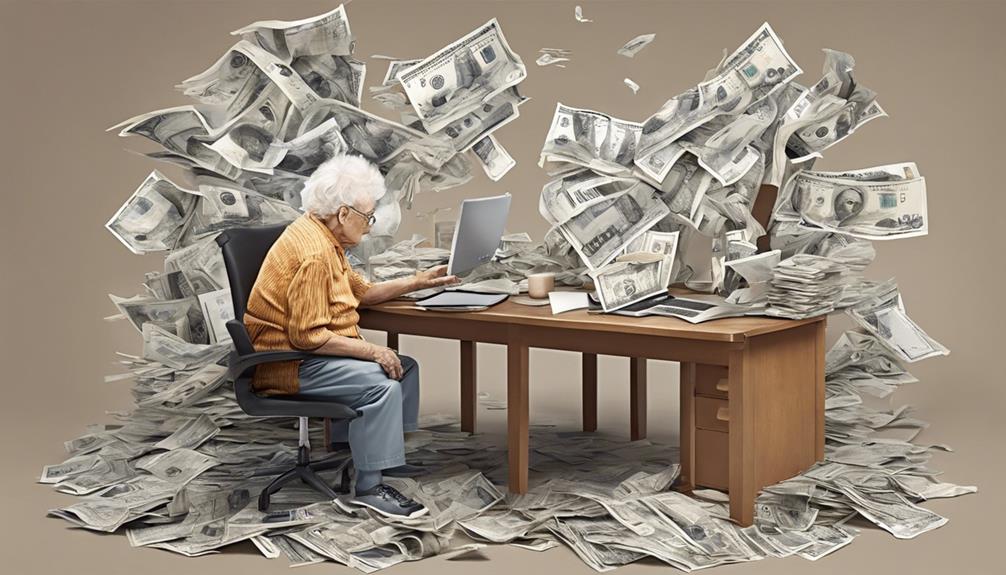
Entering the stage of moderate cognitive decline in vascular dementia, individuals undergo a notable escalation in cognitive impairment, significantly impacting their daily functioning. Memory loss, confusion, and disorientation become more pronounced, making it challenging to remember recent events or follow conversations.
Tasks that were once routine now pose difficulties, and individuals may struggle to manage their personal care and household responsibilities. Communication difficulties intensify, hindering the ability to express thoughts clearly and engage in meaningful interactions with others. Behavioral changes, such as increased irritability, anxiety, or agitation, may surface, affecting relationships and social interactions.
At this stage, individuals may require assistance with various activities of daily living, including meal preparation, medication management, and personal hygiene. It's crucial for caregivers and healthcare professionals to provide support and understanding to help navigate the challenges associated with moderate cognitive decline in vascular dementia.
Moderately Severe Cognitive Decline
During the moderately severe stage of vascular dementia, individuals confront a significant decline in cognitive function that profoundly impacts their daily activities. Memory loss, confusion, and disorientation become more pronounced, making it challenging for individuals to remember recent events or recognize familiar faces.
Communication difficulties worsen, leading to struggles in expressing thoughts and needs clearly. As cognitive abilities deteriorate, individuals may require assistance with basic tasks like dressing, eating, and personal hygiene to ensure their well-being.
Moreover, behavioral changes such as agitation, aggression, and wandering can manifest in this stage, requiring careful management and support from caregivers. These challenges highlight the critical need for a compassionate and patient approach when assisting individuals with moderately severe cognitive decline in vascular dementia.
Severe Cognitive Decline
As individuals progress into the severe cognitive decline stage of vascular dementia, their memory loss and cognitive impairment reach significant levels, necessitating extensive assistance for daily living activities. In this stage, individuals experience challenges in performing basic tasks independently, such as dressing, grooming, and eating.
Communication difficulties become more pronounced, leading to limited verbal expression and understanding of language. Behavioral changes, including aggression or agitation, may escalate, requiring specialized approaches for managing these symptoms.
Due to the severity of cognitive impairment in the severe cognitive decline stage, individuals often require 24-hour care and supervision to ensure their safety and well-being. Caregivers must be vigilant in providing support with all activities, including medication management and mobility assistance.
It's crucial to create a structured and safe environment that meets the unique needs of individuals in this stage of vascular dementia. Supporting their cognitive function and addressing behavioral challenges with empathy and patience is essential in providing quality care during this critical phase of the disease.
Very Severe Cognitive Decline
In the very severe cognitive decline stage of vascular dementia, constant supervision and care are imperative due to the profound limitations in communication and independence experienced by individuals at this advanced phase. At this stage:
- 24-Hour Care: Individuals require round-the-clock assistance and monitoring to ensure their safety and well-being.
- Limited Communication: Communication abilities are severely impacted, making it challenging for individuals to express their needs and thoughts effectively.
- Recognition of Loved Ones: While some individuals may still recognize familiar faces, cognitive impairments significantly hinder interactions and connections.
It is crucial to understand that reaching the very severe cognitive decline stage in vascular dementia progression is relatively rare. This advanced stage is often influenced by the exacerbation of cognitive decline due to other underlying health conditions.
Providing compassionate care and support tailored to the individual's needs is essential in managing the challenges associated with very severe cognitive decline in vascular dementia.
Frequently Asked Questions
How Quickly Does Vascular Dementia Progress?
Vascular dementia progression can vary in speed, influenced by factors like overall health, age, and brain damage extent. Rapid decline may occur due to multiple strokes or severe brain damage, leading to faster progression.
Monitoring cognitive and physical changes is crucial to assess the speed of progression accurately. Understanding these factors helps us provide better care and support to individuals affected by vascular dementia.
What Are the End Signs of Vascular Dementia?
In the final stages of vascular dementia, individuals may exhibit severe cognitive decline. Symptoms include incontinence, swallowing issues, intermittent recognition of loved ones, aggression, and heightened infection risk.
In very severe cognitive decline, recognizing loved ones might still be possible, but most individuals don't reach this stage. Care and supervision needs escalate significantly in the late stages of vascular dementia.
It's essential to provide compassionate and specialized support during this challenging period.
What Is the Longest You Can Live With Vascular Dementia?
We've seen cases where individuals with vascular dementia have lived up to 25 years, but this is quite rare and mostly involves those with milder forms. Factors like overall health, age at diagnosis, and symptom management effectiveness play a crucial role in life expectancy.
Quality care, symptom control, and healthy lifestyle choices can enhance quality of life and potentially extend the lifespan of individuals battling vascular dementia.
Do Vascular Dementia Patients Sleep a Lot?
Yes, vascular dementia patients may experience changes in sleep patterns. Increased daytime napping or excessive sleepiness is common, impacting cognitive function and quality of life.
Monitoring sleep habits and seeking guidance from healthcare providers is crucial for managing symptoms. Addressing sleep disturbances can lead to improved daily functioning and overall well-being for individuals with vascular dementia.
Conclusion
As we journey through the seven stages of vascular dementia, we witness the gradual decline in cognitive function and the challenges it brings. Like a ship navigating through rough waters, each stage presents its own set of obstacles that require careful navigation and support.
Just as a captain relies on a compass to guide their vessel, individuals with vascular dementia rely on the love and support of their caregivers to help them through the turbulent seas of this disease.