Our genetic makeup plays a crucial part in influencing the chances of developing osteoporosis, much like how the quality of soil affects the growth of plants in a garden.
Have you ever wondered if your family's history of fragile bones could be more than just a coincidence?
The interplay between genetics and osteoporosis is a complex web of inheritance patterns and genetic markers that hold the key to unlocking personalized prevention strategies.
Let's explore the intricate connection between our genes and bone health for a deeper understanding of osteoporosis risk factors.
Key Takeaways
- Genetic factors heavily influence osteoporosis risk.
- Family history doubles hip fracture risk.
- Genetic testing crucial for personalized prevention.
- Understanding genetic markers aids in tailored interventions.
Genetic Factors in Osteoporosis
Genetic factors significantly influence the risk of developing osteoporosis, with up to 85% of bone characteristics being determined by hereditary factors. Variants in genes such as VDR and ESR1 have been linked to a higher risk of fractures in individuals with osteoporosis. Understanding these genetic variations can help in identifying individuals predisposed to osteoporosis, allowing for early intervention and personalized treatment plans.
Genetic screening plays a crucial role in assessing an individual's risk for osteoporosis by analyzing specific genetic markers associated with low bone-mineral density. This approach enables healthcare providers to offer personalized medicine strategies tailored to each person's genetic makeup, potentially transforming fracture prevention techniques.
Family History and Osteoporosis
Family history significantly influences the risk of osteoporosis, particularly in individuals with a parental history of hip fractures. When considering the impact of family history on osteoporosis risk, several key points emerge:
- Genetic Predisposition: Having a parent who fractured a hip doubles the risk of developing osteoporosis, underscoring the strong genetic influence on the condition.
- Bone Mineral Density: Genetic predisposition from family members can contribute significantly to an individual's bone mineral density, accounting for up to 75-85% of variability in bone density.
- Fracture Risk: A positive family history of osteoporosis increases the likelihood of experiencing fractures, highlighting the importance of genetic screening and early intervention.
Understanding one's family history is crucial in identifying individuals at higher risk for osteoporosis, enabling healthcare providers to implement appropriate preventive measures. By recognizing the role of genetic factors and family history, individuals can take proactive steps to maintain bone health and reduce the risk of osteoporotic fractures.
Genetic Testing for Osteoporosis
Exploring the role of genetic testing in assessing osteoporosis susceptibility reveals valuable insights into fracture risk assessment and preventive strategies. Genetic testing can pinpoint individuals at high risk for fractures by identifying specific gene variants associated with low bone-mineral density.
Early identification of genetic risk through screening enables proactive interventions to prevent fractures. Furthermore, genetic screening plays a crucial role in tailoring personalized treatment plans for better outcomes in osteoporosis management. By understanding genetic factors through testing, healthcare providers can guide patients on lifestyle modifications and preventive measures.
This personalized approach enhances the effectiveness of interventions, leading to improved outcomes in osteoporosis prevention and treatment. Embracing genetic testing for osteoporosis empowers individuals to take control of their bone health and work towards a future with reduced fracture risk through informed decision-making and proactive management strategies.
Inheritance Patterns of Osteoporosis
Our understanding of osteoporosis inheritance patterns underscores the significant role of genetic risk factors and family history in shaping an individual's susceptibility to the condition.
Specific genes like VDR, ESR1, and COL1A1 have been identified as key players in determining osteoporosis risk, highlighting the complex interplay between genetic variations and bone health.
Genetic Risk Factors
With a strong genetic component, osteoporosis is characterized by up to 85% inheritance of bone mineral density traits. When considering genetic risk factors for osteoporosis, key genes like VDR, ESR1, ESR2, and COL1A1 play crucial roles in determining susceptibility to this condition.
Variants in these genes can significantly influence an individual's osteoporosis risk. Understanding the genetic underpinnings of osteoporosis can help identify individuals at higher risk through genetic screening.
Family history also plays a vital role in predisposing individuals to osteoporosis, further highlighting the importance of recognizing genetic influences on bone health. By examining these genetic factors, healthcare providers can offer more personalized and targeted interventions to mitigate the risk of osteoporosis and related fractures.
Family History Influences
Genetic predisposition to osteoporosis is strongly influenced by family history and specific genes associated with bone health. Family history plays a crucial role in osteoporosis heritability, with up to 85% of bone mineral density traits being hereditary.
Specific genes such as VDR, ESR1, ESR2, COL1A1, STAT1, and DAAM2 have been linked to osteoporosis, indicating a genetic predisposition to the condition. Variations in genes involved in vitamin D metabolism, collagen synthesis, and other bone health factors contribute to the genetic influence on bone density and strength, affecting the risk of developing osteoporosis based on familial genetic patterns.
Genetic testing can help uncover an individual's susceptibility to osteoporosis by analyzing their family history and specific genetic markers associated with the disease.
Genetic Markers for Osteoporosis Risk

Identifying specific gene variants associated with increased fracture risk in osteoporosis through genetic screening enhances personalized risk assessment. Genetic screening can pinpoint gene variants that are linked to a higher likelihood of fractures in individuals with osteoporosis. This knowledge enables a more targeted and individualized approach to evaluating one's risk of developing osteoporosis and experiencing bone fractures.
- Precision in Risk Assessment: Genetic screening offers a precise method to identify gene mutations that may predispose individuals to osteoporosis, aiding in the early detection of potential bone health issues.
- Tailored Interventions: Understanding the genetic factors influencing osteoporosis risk allows healthcare providers to tailor interventions and treatments based on an individual's specific genetic profile, optimizing care strategies.
- Enhanced Fracture Prediction: By uncovering genetic markers associated with osteoporosis, healthcare professionals can more accurately predict an individual's risk of experiencing fractures, leading to proactive management of bone health.
Gene-Environment Interactions in Osteoporosis
Interactions between genetic factors and environmental influences significantly contribute to the development of osteoporosis. Genetic susceptibility and gene-environment interactions play crucial roles in determining an individual's bone mineral density and fracture risk. Environmental influences such as diet, exercise, and lifestyle choices can modulate the effects of genetic variations on bone health. Understanding these complex interactions is essential for developing personalized prevention and treatment strategies for osteoporosis. Research indicates that a combination of genetic predispositions and environmental factors contributes to the multifaceted nature of osteoporosis development. By elucidating how genes and the environment interact in influencing bone health, we can better tailor interventions to individuals, ultimately improving outcomes in the prevention and management of osteoporosis.
| Genetic Susceptibility | Gene-Environment Interactions | Bone Mineral Density | Fracture Risk |
|---|---|---|---|
| High risk alleles | Lifestyle choices | Reduced density | Increased risk |
Epigenetics and Osteoporosis Risk
As we explore the role of epigenetics in osteoporosis risk, it becomes evident that epigenetic factors can exert significant influence on gene expression associated with bone health.
Key Points:
- DNA Methylation and Histone Modifications: These epigenetic mechanisms play crucial roles in bone density regulation, potentially impacting the development of osteoporosis.
- Environmental Influence: Factors such as nutrition and lifestyle choices can induce epigenetic changes that are linked to variations in osteoporosis susceptibility.
- Personalized Prevention Strategies: Studying epigenetic markers offers promising insights into tailoring personalized prevention and treatment strategies for osteoporosis, emphasizing the importance of considering individual epigenetic profiles in managing bone health.
Understanding how epigenetic alterations contribute to osteoporosis can pave the way for targeted interventions and more effective management of this condition.
Genetic Counseling for Osteoporosis
Genetic counseling for osteoporosis offers valuable insights into individual risk factors using genetic assessments. Counselors analyze family history to provide personalized strategies for prevention and management.
These sessions empower individuals to make informed decisions about their bone health based on genetic influences.
Risk Assessment Options
Risk assessment options in genetic counseling for osteoporosis involve evaluating an individual's genetic risk factors for developing the condition. Genetic counselors assess susceptibility to osteoporosis and provide personalized recommendations to reduce the risk of fractures.
During counseling sessions, lifestyle modifications, screening options, and preventive measures are discussed to empower individuals in making informed decisions about their bone health.
3 Key Points:
- Assessing genetic risk factors helps understand susceptibility to osteoporosis.
- Personalized recommendations can mitigate the risk of fractures.
- Counseling sessions cover lifestyle modifications, screening options, and preventive measures to improve bone health.
Family History Analysis
Analyzing familial history provides valuable insights into the potential genetic predisposition to osteoporosis. Genetic counseling for osteoporosis utilizes family history to assess the likelihood of inheriting the condition. By understanding one's family history, individuals can tailor personalized prevention strategies and intervene early if at risk. Genetic testing may be recommended for those with a family history of osteoporosis to better evaluate their susceptibility. Genetic counseling serves a critical role in educating individuals about their genetic predisposition to osteoporosis, enabling them to make informed decisions about their health.
| Family History Analysis | ||
|---|---|---|
| Identify at-risk individuals | Guide personalized prevention strategies | Determine potential inheritance |
| Assess genetic predisposition | Encourage early intervention | Recommend genetic testing |
Prevention Strategies Tailored
Understanding familial history of osteoporosis can serve as a foundational step towards tailoring personalized prevention strategies through genetic counseling. Genetic counseling for osteoporosis enables individuals to comprehend their genetic risk factors, guiding the development of personalized recommendations.
Here are three key aspects to consider:
- Identification of Genetic Risk Factors: Genetic screening can pinpoint individuals at high risk for osteoporosis, facilitating early interventions.
- Personalized Prevention Strategies: Lifestyle modifications, dietary adjustments, and exercise regimens can be tailored based on genetic predispositions to mitigate the risk of osteoporosis.
- Optimizing Bone Health: Genetic counseling offers personalized recommendations to enhance bone health and decrease fracture susceptibility.
Genetic counseling empowers individuals to proactively manage their bone health and prevent the onset of osteoporosis.
Osteoporosis Risk Assessment Through Genetics
Genetic screening plays a crucial role in identifying individuals at high risk for osteoporotic fractures based on specific gene variants. By understanding genetic factors, personalized treatment plans can be tailored to prevent osteoporotic fractures. Certain gene mutations may predispose individuals to developing osteoporosis, highlighting the importance of genetic screening in assessing osteoporosis risk. A computer algorithm has been developed to assign risk scores and identify those at high risk for osteoporosis and fractures, allowing for proactive management of osteoporosis risk and improved bone health outcomes.
| Genetic Screening | Role in Osteoporosis Risk Assessment |
|---|---|
| Identify high-risk individuals | Based on specific gene variants |
| Personalized treatment plans | Tailored to prevent fractures |
| Gene mutations | Predisposition to osteoporosis |
| Computer algorithm | Assigns risk scores for proactive management |
Future of Genetic Research in Osteoporosis

As we look ahead to the future of genetic research in osteoporosis, we anticipate exciting prospects such as:
- Gene therapy potential
- Personalized treatment options
- Improved genetic risk assessment tools
These advancements hold the promise of tailoring interventions to individual genetic profiles, enhancing the precision and effectiveness of osteoporosis management strategies. By leveraging genetic insights, we aim to optimize fracture prevention approaches and ultimately elevate bone health outcomes for all.
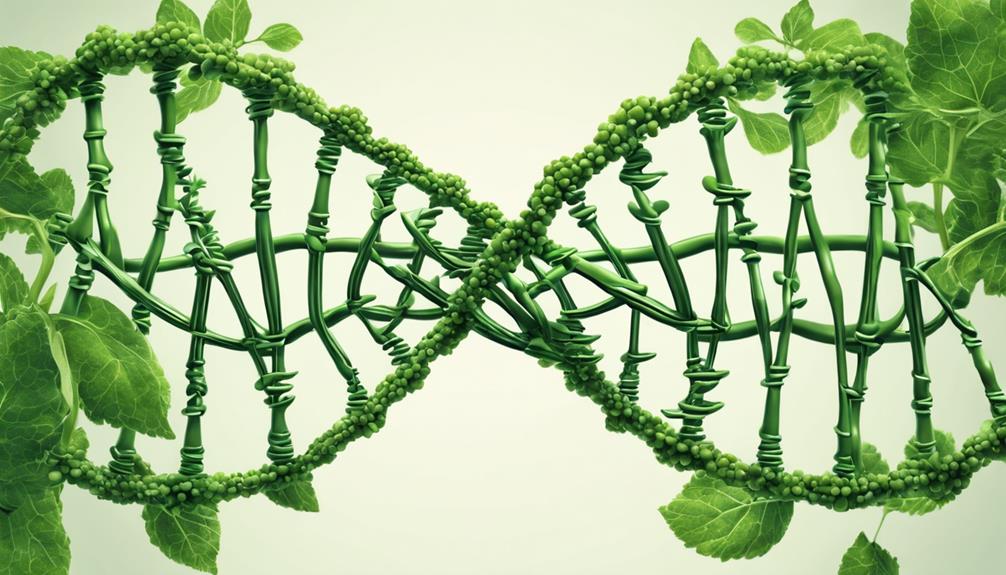
Gene Therapy Potential
How can gene therapy revolutionize the treatment of osteoporosis by targeting specific genetic factors influencing bone health?
Gene therapy offers a promising avenue for addressing osteoporosis by pinpointing and correcting key genetic factors that contribute to the disease. Through personalized treatments tailored to individual genetic profiles, researchers aim to enhance bone density and reduce fracture risk in susceptible individuals.
Techniques like CRISPR-Cas9 provide precise tools for editing genetic mutations associated with osteoporosis, paving the way for innovative approaches in precision medicine. Understanding the genetic basis of osteoporosis is crucial for developing effective gene therapies that could potentially transform the future of osteoporosis treatment.
Personalized Treatment Options
Exploring the potential of personalized treatment options in osteoporosis based on genetic factors presents a promising avenue for enhancing interventions tailored to individual needs and genetic profiles. Understanding individual genetic profiles allows for targeted preventive measures to reduce fracture risk in high-risk individuals. Genetic screening may revolutionize osteoporosis management by providing personalized strategies for improving bone density. Future genetic research in osteoporosis could pave the way for customized therapies that address specific genetic vulnerabilities to enhance bone strength.
| Genetic Factors | Personalized Treatment | Bone Health Outcomes |
|---|---|---|
| Individual genetic profiles | Tailored interventions | Optimize bone health outcomes |
| Fracture risk | Targeted preventive measures | Reduce fracture risk |
| Genetic screening | Personalized strategies | Improve bone density |
| Customized therapies | Specific genetic vulnerabilities | Enhance bone strength |
Genetic Risk Assessment
Genetic risk assessment in osteoporosis entails the identification of individuals at high risk for fractures through genetic screening. This approach is crucial for enhancing personalized medicine strategies in osteoporosis care. By uncovering more risk markers through genetic research, we aim to target high-risk individuals for interventions effectively.
Genetic screening has the potential to revolutionize fracture prevention by allowing us to tailor prevention and treatment plans to each person's unique genetic makeup. Understanding the genetic influences on bone health not only guides individualized care but also informs broader public health policies for osteoporosis prevention.
The development of genetic algorithms holds promise in predicting osteoporosis risk accurately, further advancing the field of bone health management.
Frequently Asked Questions
Can Osteoporosis Run in the Family?
Osteoporosis can definitely run in families due to a strong genetic component influencing bone health. Understanding this link is crucial for predicting and managing the condition.
Genetic markers like BMP2, VDR, ESR1, and others can impact susceptibility. Screening for these genes can help identify those at higher risk.
This knowledge allows us to take proactive steps to mitigate the effects of osteoporosis within families.
What Percent of Osteoporosis Is Genetic?
We understand the importance of genetic factors in osteoporosis. Just like a finely tuned orchestra, our genes play a critical role in determining bone health.
Up to 85% of bone mineral density and fracture risk variability is linked to genetics. Family history can increase susceptibility, with specific genes like VDR and ESR1 influencing bone strength.
Recognizing these genetic components empowers us to predict, prevent, and manage osteoporosis more effectively.
What Age Does Osteoporosis Start?
Osteoporosis typically starts around age 30 when bone mass plateaus. As we age, especially after 50, the risk of developing osteoporosis significantly rises.
It's crucial to prioritize early detection through bone density testing from age 50 onwards to prevent complications. Factors like diet, exercise, and sun exposure are pivotal in reducing the risk of osteoporosis.
Taking proactive steps early can help safeguard bone health for the future.
Who Is Most Prone to Osteoporosis?
We're more prone to osteoporosis as women, especially after menopause, due to hormonal changes that decrease bone density. Factors like family history, aging, low calcium intake, and a sedentary lifestyle also play a role.
Postmenopausal women face increased bone loss due to decreased estrogen levels, raising fracture risks. Engaging in healthy habits and monitoring bone health can help reduce the likelihood of developing osteoporosis.
Conclusion
In conclusion, our understanding of the genetic factors influencing osteoporosis is crucial for personalized prevention and treatment strategies.
Did you know that up to 85% of the variation in bone mineral density is determined by genetic factors?
By identifying genetic markers and inheritance patterns, we can better assess osteoporosis risk and provide tailored care for improved bone health outcomes.
The future of genetic research in osteoporosis holds promise for advancing fracture prevention and personalized patient care.