Thinking about how osteoporosis affects the hip bones, it is clear that this condition can significantly affect a person’s quality of life. Just picture the difficulties that arise when simple tasks like walking or standing become painful and difficult. Delving into the intricacies of osteoporosis and its connection to the hips involves more than just recognizing its existence; it involves exploring the essential elements necessary to enhance bone strength and enhance overall well-being.
By delving into the causes, symptoms, diagnosis, treatments, and prevention strategies, we can cultivate a deeper understanding of how to address this condition effectively.
Key Takeaways
- Hormonal changes and aging contribute to hip osteoporosis risk.
- Early recognition and accurate diagnosis are crucial for timely intervention.
- Treatment options include medications, exercises, therapy, and proper nutrition.
- Prevention involves screenings, calcium intake, exercises, and healthy lifestyle habits.
Causes of Osteoporosis in Hips
Aging, hormonal changes, and genetic predispositions are primary factors that contribute to the development of osteoporosis in the hips. As we age, our bone density naturally decreases, making the bones more susceptible to fractures and conditions like osteoporosis. Hormonal changes, such as a decline in estrogen levels in women during menopause, can also play a significant role in reducing bone density and increasing the risk of hip osteoporosis. Additionally, genetic predispositions can influence the way our bones form and remodel, affecting their strength and resilience over time.
Furthermore, lack of weight-bearing exercise can contribute to decreased bone density in the hips, making them more vulnerable to osteoporosis. Weight-bearing exercises, such as walking, running, or resistance training, help stimulate bone formation and maintain bone strength. In contrast, a sedentary lifestyle can lead to weakened bones and an increased risk of hip fractures. Therefore, incorporating regular weight-bearing exercises into our routine can help prevent or slow down the progression of osteoporosis in the hips.
Symptoms of Hip Osteoporosis
When experiencing hip osteoporosis, sudden and intense hip pain that worsens with activity can signal underlying bone weakness.
Besides pain, a limited range of motion in the hip joint and the development of a noticeable limp are common symptoms indicating hip osteoporosis.
It's crucial to recognize these signs early to prevent increased fracture risk and seek medical evaluation for appropriate diagnosis and management.
Hip Pain Indication
Experiencing sudden and worsening hip pain with activity or weight-bearing could signal the presence of hip osteoporosis, characterized by limited range of motion, a noticeable limp, and persistent discomfort in the groin or buttocks. When hip pain indicates possible osteoporosis, it's important to consider the following symptoms:
- Sudden onset of severe hip pain
- Difficulty in moving the hip joint
- Development of a noticeable limp
- Persistent discomfort in the groin or buttocks
Understanding these indicators can prompt individuals to seek timely medical evaluation for accurate diagnosis and appropriate management of hip osteoporosis, potentially preventing further complications like fractures and chronic pain.
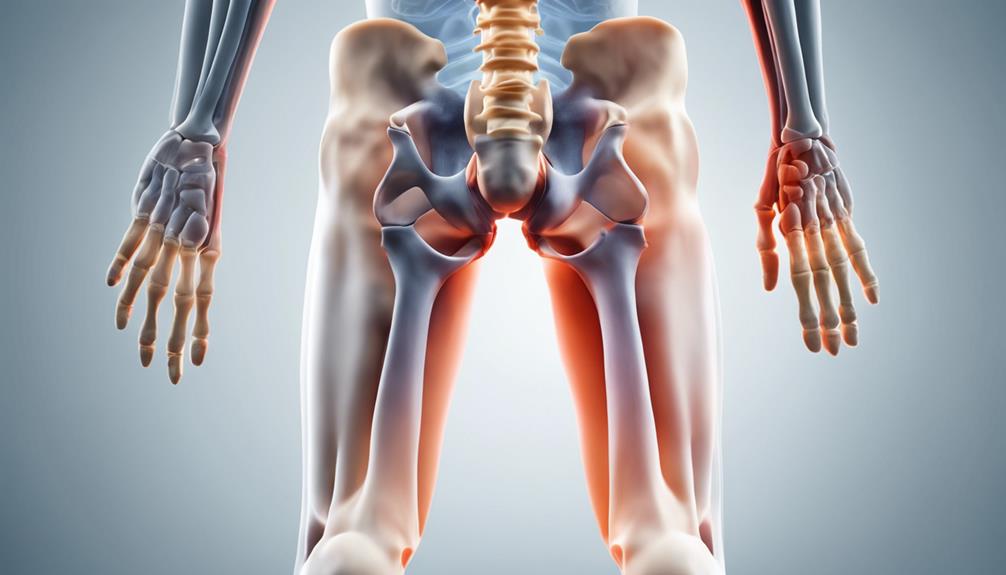
Fracture Risk Assessment
Symptoms indicative of hip osteoporosis include sudden and severe hip pain exacerbated by activity or weight-bearing, limited range of motion in the hip joint, and the development of a noticeable limp, all of which signal an increased risk of fractures in the pelvis or femur.
As bone mass decreases in the hip joint, the risk of hip fractures rises significantly. Diagnosis of transient or persistent hip pain coupled with limited mobility can aid in early detection of osteoporosis and prevent further complications.
Fracture risk assessment is crucial in managing hip osteoporosis to prevent fractures in the fragile bones of the pelvis or femur. Early diagnosis and intervention are essential in maintaining bone health and preventing debilitating hip fractures that can severely impact an individual's quality of life.
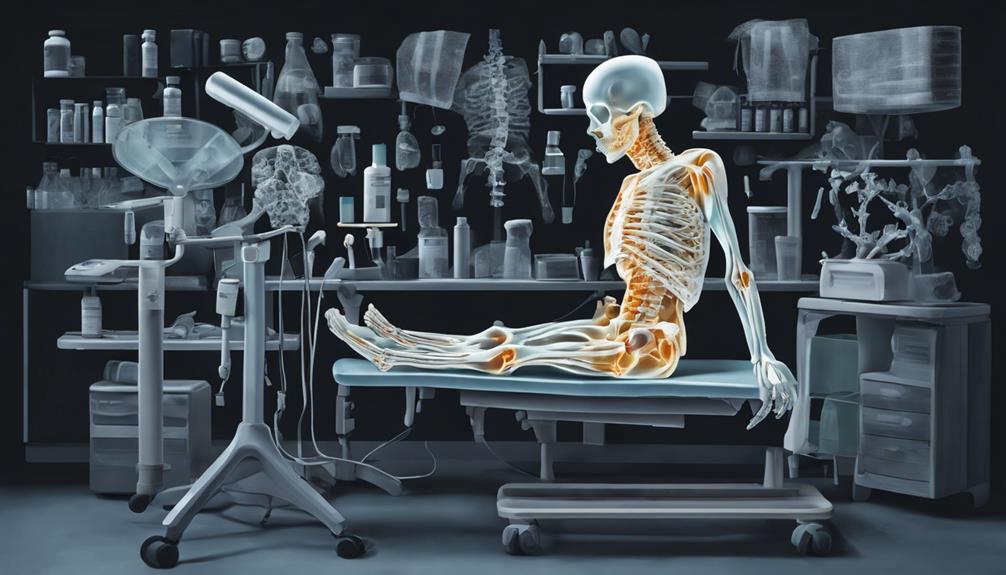
Diagnosis of Hip Osteoporosis
In diagnosing hip osteoporosis, a combination of physical exams, X-rays, bone density scans, and MRIs are utilized to evaluate bone health and density in the hip joint. Specific imaging tests like dual-energy X-ray absorptiometry (DEXA) scans are commonly used to measure bone mineral density in the hip.
Here are key points regarding the diagnosis of hip osteoporosis:
- Physical exams play a crucial role in assessing the risk factors and symptoms associated with hip osteoporosis.
- X-rays provide detailed images of the hip joint, helping identify fractures and bone density changes.
- Bone density scans offer precise measurements of bone mineral density, aiding in the confirmation and severity assessment of osteoporosis.
- MRIs can detect early signs of osteoporosis in the hip, such as bone marrow edema, contributing to an accurate diagnosis and treatment planning.
Early and accurate diagnosis of hip osteoporosis is essential for implementing timely interventions to prevent fractures and effectively manage bone health.
Available Treatments for Hip Osteoporosis
We'll explore the efficacy of medications such as bisphosphonates and calcitonin in strengthening bones affected by hip osteoporosis.
Additionally, we'll analyze the importance of physical therapy for enhancing hip strength, flexibility, and function.
Furthermore, we'll address the significance of weight-bearing exercises, proper nutrition, calcium intake, and vitamin D supplementation in managing hip osteoporosis.
Medication Options
Among the available treatments for hip osteoporosis, medications like bisphosphonates, teriparatide, denosumab, calcitonin nasal spray, and strontium ranelate play crucial roles in managing bone density and fracture risks.
Bisphosphonates, such as alendronate and risedronate, increase bone density and decrease fracture risk.
Teriparatide stimulates new bone formation, particularly beneficial for severe hip osteoporosis.
Denosumab inhibits bone breakdown, providing an alternative treatment option.
Calcitonin nasal spray helps prevent bone loss in the hip by reducing osteoclast activity, though its usage has declined due to limited efficacy.
Strontium ranelate promotes bone formation and reduces bone resorption; however, its use is restricted in some regions due to safety concerns.
These medications offer diverse approaches to address the complexities of managing hip osteoporosis.
Exercise Recommendations
Weight-bearing exercises such as walking, dancing, and stair climbing are essential for strengthening hip bones and preventing fractures related to osteoporosis.
In addition to these activities, incorporating resistance training into your exercise routine can improve bone density and muscle strength in the hips.
Balance exercises like yoga, tai chi, and pilates are crucial for reducing the risk of falls and fractures in individuals with hip osteoporosis.
Aerobic exercises, when done regularly, can enhance overall bone health and well-being.
It's important to consult with a healthcare provider or physical therapist to develop a personalized exercise plan tailored to your specific needs and abilities.
Dietary Considerations
In managing hip osteoporosis, ensuring adequate calcium intake from various sources such as dairy, leafy greens, and soy products is crucial for maintaining bone strength in the hips. To support bone health effectively, consider incorporating the following dietary considerations:
- Proper nutrition plays a key role in hip osteoporosis management.
- Vitamin D supplements aid in calcium absorption, essential for bone density.
- Including calcium-rich foods in your diet can help meet daily requirements for bone strength.
- Paying attention to dietary sources that promote calcium absorption is vital for hip health.
Managing Hip Osteoporosis

To effectively manage hip osteoporosis, a tailored treatment plan is essential, focusing on accurate diagnosis to alleviate discomfort and restore normal functionality. When addressing hip osteoporosis, a combination of interventions can be beneficial. Below is a table summarizing key strategies for managing hip osteoporosis:
| Intervention | Description | Benefits |
|---|---|---|
| Bone Scan | Diagnostic tool to assess bone density and strength | Identify areas of weakness in the hip bones |
| Physical Therapy | Customized exercises to improve hip strength and mobility | Enhance range of motion and reduce pain |
| Anti-inflammatory Meds | Medications to decrease inflammation and alleviate pain | Manage discomfort and improve quality of life |
Utilizing these interventions in conjunction with assistive devices, nutritional changes, and professional guidance can help prevent fractures, support rehabilitation, and enhance the effectiveness of strengthening exercises for individuals managing hip osteoporosis.
Prevention of Hip Osteoporosis

Regular bone density screenings and discussions with healthcare providers are crucial for the early detection and prevention of hip bone loss, aiding in the proactive management of osteoporosis risk factors.
To enhance hip bone health and prevent osteoporosis, consider the following:
- Maintain Adequate Calcium Intake: Consuming around 1,000mg of calcium daily for adults aged 18-50 is essential for optimal bone health in the hips.
- Engage in Weight-Bearing Exercises: Incorporate activities like walking, jogging, or dancing into your routine to strengthen hip bones and reduce the risk of osteoporosis.
- Ensure Sufficient Vitamin D Levels: Obtain sunlight exposure or take supplements to support calcium absorption, promoting strong hip bones and preventing osteoporosis.
- Adopt Healthy Lifestyle Habits: Quit smoking, moderate alcohol intake, and maintain a healthy body weight to prevent hip osteoporosis.
Frequently Asked Questions
How Serious Is Osteoporosis in Hips?
Osteoporosis is a serious condition that weakens bones, increasing fracture risk. The impact of osteoporosis extends beyond bones, affecting overall health.
Prevention strategies like adequate calcium intake and weight-bearing exercise can help mitigate risks. Early detection through bone density scans is crucial for timely intervention.
Managing osteoporosis involves a comprehensive approach, including lifestyle modifications and possibly medication. Education and awareness are vital in combating the effects of osteoporosis.
What Is the Best Treatment for Hip Osteoporosis?
When it comes to treating hip osteoporosis, a comprehensive approach is vital. Incorporating bisphosphonates and calcitonin can bolster bone strength and decrease fracture risk. Physical therapy is also crucial in enhancing hip strength, mobility, and overall function. Additionally, weight-bearing restrictions and walking aids may be recommended to alleviate stress on the affected hip. NSAIDs can help manage pain, facilitating improved daily activities and quality of life. Monitoring bone density and treatment adherence are essential for long-term management.
Is Walking Good for Osteoporosis of the Hips?
Walking is excellent for individuals with osteoporosis, including the hips. It benefits bone density, growth, and strength, reducing fracture risks.
Regular walking improves balance, coordination, flexibility, and muscle strength in the lower body, supporting hip joints and overall stability.
Consulting with healthcare providers or physical therapists is crucial to determine the appropriate walking routine based on individual needs and osteoporosis severity.
Can Osteoporosis of the Hip Be Reversed?
Absolutely, osteoporosis of the hip can be reversed with a multifaceted approach. Through medication, exercise, and nutrition, bone density can improve, reducing the risk of fractures.
Consistent monitoring and adherence to treatment plans are crucial in slowing down or even halting the progression of osteoporosis.
Early intervention and a comprehensive management strategy can effectively enhance bone health and potentially reverse the effects of osteoporosis.
Conclusion
In conclusion, managing osteoporosis in hips requires early detection, personalized treatment plans, and a focus on prevention strategies.
Just as a strong foundation is essential for a sturdy building, maintaining bone health is crucial for a healthy and active lifestyle.
By taking proactive steps to address hip osteoporosis, individuals can reduce the risk of fractures and improve overall quality of life. Remember, prevention is always better than cure when it comes to bone health.