When it comes to bone and joint health, it is important to recognize the differences between osteoporosis and osteoarthritis in order to effectively manage these prevalent conditions.
While both impact bones and joints, the way they manifest and require treatment differs significantly. Let's explore the nuances between these two conditions and how recognizing their unique characteristics can empower us to make informed decisions about our health.
Key Takeaways
- Osteoporosis linked to bone loss, fractures, post-menopausal women.
- Osteoarthritis due to joint degeneration, pain, stiffness, aging.
- Osteoporosis prevention: bone density preservation strategies.
- Osteoarthritis treatment includes medications, joint replacements, lifestyle modifications.
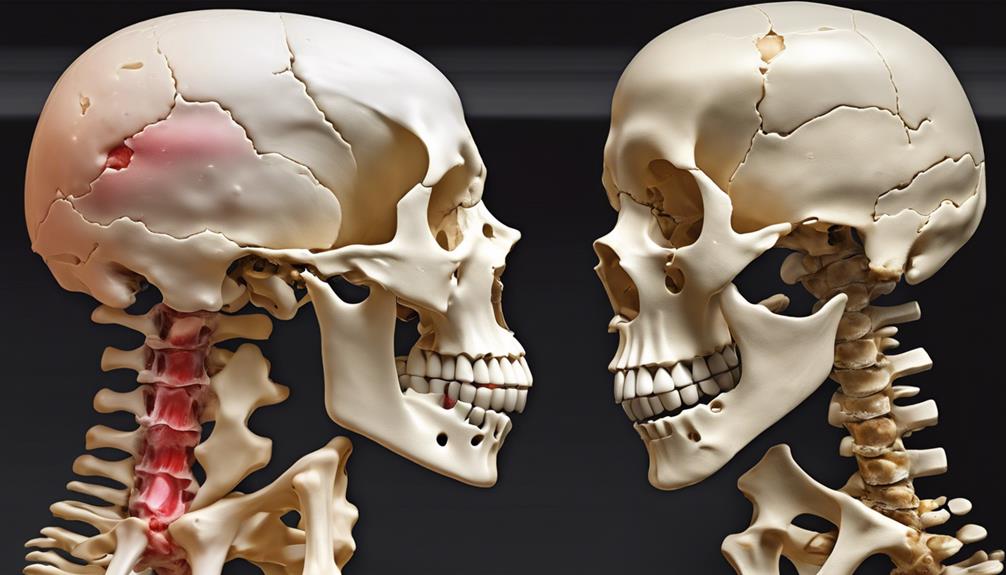
Key Differences in Causes
Comparing the causes of osteoporosis and osteoarthritis reveals distinct mechanisms underlying these prevalent musculoskeletal conditions. Osteoporosis primarily stems from bone loss and fragility, increasing the risk of fractures. Women, especially post-menopause, are more susceptible due to hormonal changes affecting bone density. On the other hand, osteoarthritis is mainly driven by degenerative joint processes, characterized by cartilage breakdown and bone spurs due to joint wear and tear. This condition is commonly linked to aging, joint overuse, or injury, affecting joint structure.
Factors contributing to osteoporosis include genetics, age, low calcium intake, and hormonal fluctuations. In contrast, osteoarthritis risk factors involve joint stress, obesity, and prior joint injuries. Understanding these distinctions is crucial for tailored prevention and management strategies. While osteoporosis focuses on preserving bone density to prevent fractures, osteoarthritis management often revolves around pain relief, improving joint function, and potentially surgical interventions to address severe joint damage. By recognizing these diverse causes, healthcare providers can offer more effective care to individuals affected by these conditions.
Symptoms of Osteoporosis

Bone density loss in osteoporosis can go unnoticed until a fracture risk increases significantly.
Back pain is a common symptom indicating potential bone weakening and fracture susceptibility.
Understanding these early signs is crucial for timely intervention and prevention of debilitating fractures.
Bone Density Loss
In osteoporosis, the loss of bone density often remains asymptomatic until a fracture occurs in critical areas such as the hip, spine, or wrist. Risk factors for osteoporosis include age, genetics, hormonal imbalances, and lifestyle choices like smoking and excessive alcohol consumption.
Low bone mineral density is a key indicator of osteoporosis, making bone density screenings crucial for early detection and effective management. Fractures in osteoporosis can be triggered by simple movements like bending or even sneezing due to weakened bones.
Diagnosis involves bone mineral density tests focusing on the spine and hip. Individuals with low bone mineral density face a significant risk of osteoporotic fractures, emphasizing the importance of proactive measures to prevent such occurrences.
Fracture Risk Increases
Considering the increased fracture risk associated with osteoporosis, early detection through bone mineral density testing is imperative for effective management and prevention strategies. Osteoporosis significantly raises the likelihood of fractures, particularly in weight-bearing bones like the hip, spine, and wrist.
Even minor actions such as bending or sneezing can lead to fractures due to compromised bone mass. Since osteoporosis is often asymptomatic until a fracture occurs, assessing bone density through specialized testing becomes crucial.
Fractures resulting from osteoporosis not only cause severe pain but also restrict mobility, impacting overall quality of life. Therefore, understanding and addressing fracture risk through proactive measures like bone mineral density testing are essential in combating the debilitating effects of osteoporosis.
Back Pain Common
Symptoms of osteoporosis commonly manifest as back pain, often indicating the presence of spinal fractures. This back pain is a result of weakened vertebrae due to bone loss, which can lead to sudden and severe discomfort.
Osteoporosis-related back pain may worsen with movement or certain positions, affecting daily activities. Recognizing these symptoms is crucial as early detection and treatment of osteoporosis can help prevent debilitating back pain and fractures.
Monitoring bone health through regular check-ups and lifestyle modifications can aid in reducing the risk of spinal fractures and associated back pain. Understanding the connection between bone health and back pain is essential for maintaining overall well-being and quality of life.
Symptoms of Osteoarthritis

When experiencing osteoarthritis, individuals may notice joint pain, stiffness, swelling, and a reduced range of motion as common symptoms. Osteoarthritis predominantly affects joints such as the hips, knees, fingers, feet, and spine.
The joint pain associated with osteoarthritis often worsens after physical activity or towards the end of the day. This condition can also lead to the development of bony growths or bone spurs within the affected joints, further exacerbating the discomfort experienced by individuals.
It's crucial to recognize that the symptoms of osteoarthritis can be easily overlooked or mistaken for general joint discomfort, highlighting the importance of accurate diagnosis and appropriate management strategies. By understanding these physical manifestations of osteoarthritis, individuals and healthcare providers can work together to effectively address and alleviate the challenges posed by this common joint condition.
Diagnosing Osteoporosis
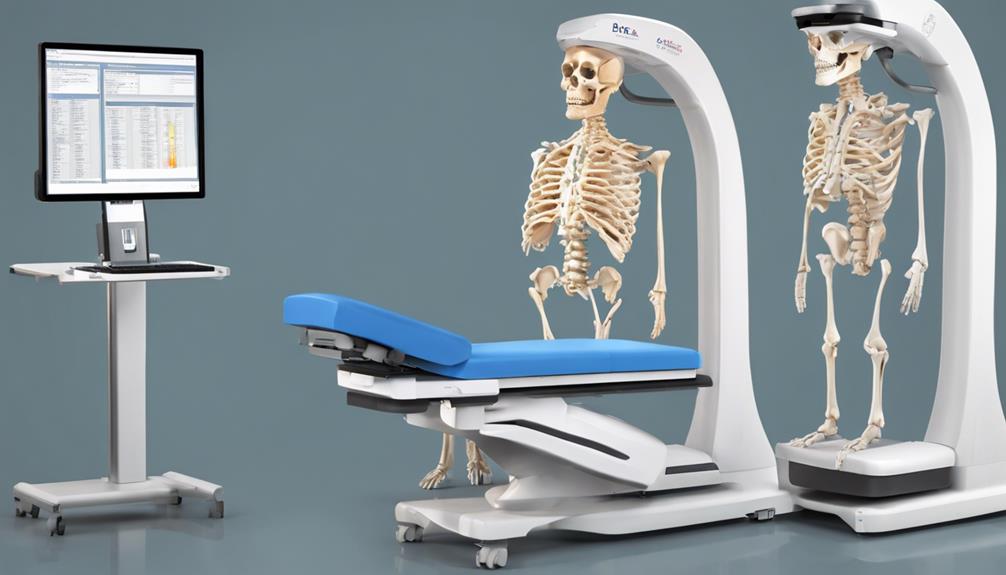
An essential component of diagnosing osteoporosis involves conducting a bone mineral density test, commonly referred to as a DXA scan, to evaluate bone density in specific areas like the spine and hip. This test helps determine the presence of low bone mineral density, a key indicator of osteoporosis.
By comparing the patient's bone density to that of a young adult reference population, healthcare providers can assess the risk of fractures associated with osteoporosis. In addition to the DXA scan, blood tests may be included in the diagnostic process to rule out other conditions that could contribute to bone loss.
The World Health Organization defines osteoporosis based on bone mineral density T-scores, with values below -2.5 indicating the presence of osteoporosis. Early diagnosis plays a critical role in preventing fractures and effectively managing bone health, highlighting the importance of timely and accurate osteoporosis diagnosis.
Diagnosing Osteoarthritis

To accurately diagnose osteoarthritis, healthcare providers conduct a thorough review of the patient's medical history to evaluate joint symptoms and identify potential risk factors. Physical examinations play a crucial role in the diagnostic process, involving joint assessments and range of motion tests to assess the extent of joint damage and functional limitations.
Additionally, X-rays are commonly utilized to visualize specific changes associated with osteoarthritis, such as joint damage, bone spurs, and narrowing of joint spaces. Unlike some other conditions, blood tests are typically not necessary for diagnosing osteoarthritis, as the diagnosis primarily relies on clinical findings and imaging studies.
Risk Factors for Osteoporosis

A crucial factor in determining the susceptibility to osteoporosis fractures is low bone mineral density. Individuals with lower bone mineral density are at a higher risk of experiencing fractures due to weakened bones. Other significant risk factors for osteoporosis include older age, prior fractures, history of falls, certain medications such as corticosteroids, and a family history of fragility fractures.
Additionally, lifestyle factors like inadequate calcium or vitamin D intake, sedentary habits, and the use of certain medications can also increase the risk of developing osteoporosis.
To address these risk factors effectively, it's essential to promote bone health through adequate nutrition, regular weight-bearing exercise, and lifestyle modifications. Healthcare providers play a crucial role in educating individuals about these risks and guiding them towards preventive measures.
Understanding and addressing these risk factors are fundamental steps in the prevention and management of osteoporosis, ultimately leading to better bone health and reduced fracture risk.
Risk Factors for Osteoarthritis

In considering the risk factors for osteoarthritis, familial history emerges as a significant determinant. Understanding these risk factors is crucial in managing and preventing the development of this condition.
Here are four key factors to be aware of:
- Family History: Individuals with a family history of osteoarthritis are at a higher risk due to genetic predispositions that may affect bone mass and the health of affected joints.
- Physical Inactivity and Excess Weight: Sedentary lifestyles and obesity contribute to the risk of osteoarthritis by putting extra strain on the joints, leading to wear and tear.
- Joint Overuse: Occupations or activities that involve repetitive movements can increase the likelihood of osteoarthritis by putting stress on the affected joints over time.
- Medication Use: Certain medications, such as corticosteroids, can elevate the risk of developing osteoarthritis by impacting bone health and joint function.
Being mindful of these risk factors and taking proactive steps to address them can help in the prevention and management of osteoarthritis.
Treatment Options for Osteoporosis

Familial history, along with lifestyle modifications and pharmacological interventions, plays a significant role in the comprehensive treatment approach for osteoporosis. Treatment options for osteoporosis encompass various strategies aimed at improving bone health and reducing fracture risk.
Incorporating weight-bearing exercises into daily routines is crucial as they help strengthen bones and improve overall bone density. Additionally, medications such as Actonel, Fosamax, and Prolia are commonly prescribed to increase bone density and decrease the likelihood of fractures in individuals with osteoporosis.
Calcium and vitamin D supplementation are essential components of osteoporosis treatment to support bone health. Surgical interventions like kyphoplasty and vertebroplasty may be considered in severe cases to stabilize fractures and relieve pain.
Consulting with a specialist is highly recommended to develop personalized treatment plans tailored to individual needs and ensure ongoing management of osteoporosis. By combining lifestyle adjustments, pharmacological support, and medical guidance, individuals can effectively manage osteoporosis and reduce its impact on daily life.
Treatment Options for Osteoarthritis

Implementing a multifaceted approach that combines non-pharmacological methods, medications, and surgical interventions forms the core of treatment options for osteoarthritis. When addressing osteoarthritis, here are key strategies to consider:
- Non-Pharmacological Approaches: Exercise, weight management, and physical therapy play crucial roles in managing osteoarthritis symptoms and improving joint function.
- Medications for Symptom Relief: Commonly used medications like acetaminophen, NSAIDs, and corticosteroid injections can help alleviate pain and inflammation associated with osteoarthritis.
- Surgical Interventions: In severe cases where conservative measures fail, surgical options such as joint replacement or arthroplasty may be recommended to restore joint function.
- Hyaluronic Acid Injections: These injections can provide temporary relief by lubricating and cushioning the affected joint, offering a complementary treatment option for osteoarthritis management.
Managing Both Conditions Together

When managing both osteoporosis and osteoarthritis concurrently, it's crucial to focus on exercise for strength and maintaining joint mobility.
A balanced diet rich in calcium and vitamin D is essential to support bone health and overall well-being.
Exercise for Strength
Engaging in a diverse range of targeted exercises plays a crucial role in enhancing muscle strength, joint stability, and overall physical well-being for individuals concurrently managing osteoporosis and osteoarthritis. Here are four key exercise strategies to consider for improving strength and mobility while dealing with both conditions:
- Weight-bearing Exercises: Activities like walking, hiking, and dancing can help improve bone density and strengthen muscles.
- Resistance Training: Using light weights or resistance bands can assist in building muscle mass, supporting joint stability, and reducing the risk of falls.
- Tai Chi and Yoga: These practices enhance balance, flexibility, and coordination, which can improve joint mobility and alleviate pain.
- Water-Based Activities: Swimming or aqua aerobics provide low-impact options that support joint movement and muscle strength without straining bones.
Balanced Diet Importance
Enhancing muscle strength and joint stability through targeted exercises is foundational, and equally important is the role of a balanced diet rich in essential nutrients like calcium and vitamin D when managing both osteoporosis and osteoarthritis.
Calcium is crucial for maintaining bone mass, reducing fracture risk in osteoporosis, and supporting joint health in osteoarthritis. Vitamin D aids in calcium absorption, benefiting bone strength and joint function. Including omega-3 fatty acids, antioxidants, and anti-inflammatory foods can help alleviate inflammation and pain in osteoarthritis while supporting bone health in osteoporosis.
Additionally, maintaining a healthy weight through a balanced diet can ease pressure on arthritic joints and lower fracture risks. A well-rounded diet plays a key role in managing both conditions effectively.
Improving Bone Health

To enhance bone health effectively, incorporating weight-bearing exercises such as walking, dancing, and weightlifting into a regular routine is crucial. These activities help improve bone density and reduce the risk of osteoporosis.
To further support bone health, adequate intake of calcium and vitamin D through diet or supplements is essential. Additionally, resistance training, like using resistance bands or lifting weights, can help build muscle strength, which in turn supports bone health.
Avoiding smoking and excessive alcohol consumption is also crucial in preventing bone loss and maintaining overall bone health.
Tips for Improving Bone Health:
- Incorporate weight-bearing exercises like walking, dancing, and weightlifting into your routine.
- Ensure adequate intake of calcium and vitamin D through diet or supplements.
- Include resistance training in your workouts to build muscle strength and support bone health.
- Avoid smoking and excessive alcohol consumption to prevent bone loss.
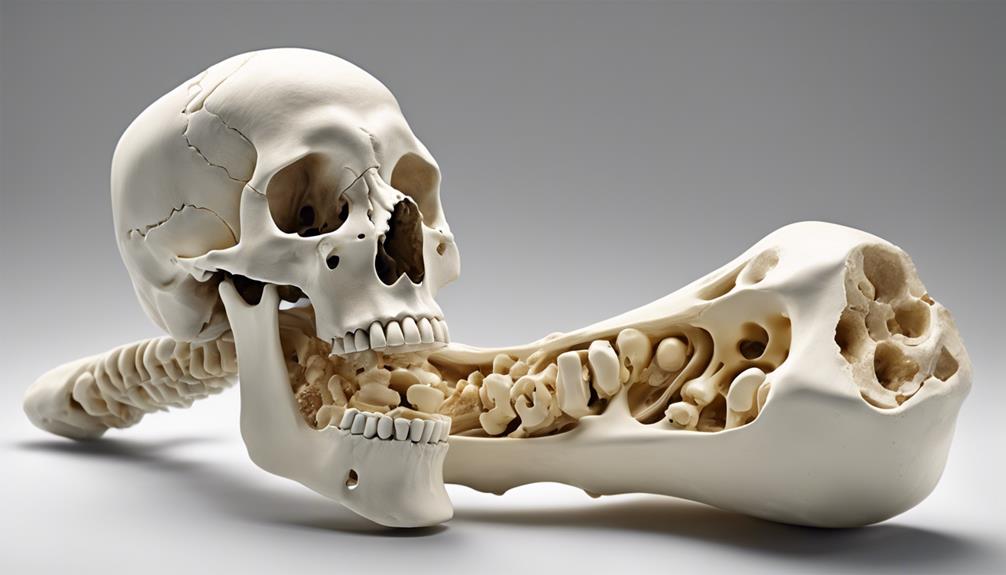
Understanding Joint and Cartilage Problems

Understanding joint and cartilage problems involves delving into the complexities of osteoarthritis, which encompasses joint deterioration and bone-on-bone issues in various areas such as fingers, knees, hips, spine, neck, and shoulders. Osteoarthritis is linked to the loss of bone mass and affects millions worldwide. The relationship between osteoarthritis and bone health is crucial, as the condition leads to a gradual breakdown of cartilage, causing pain, stiffness, and reduced function in the affected joints. Excess body weight can exacerbate osteoarthritis, making it essential to manage weight to alleviate symptoms. Diagnosis includes a comprehensive evaluation, including medical history, physical examination, and imaging studies. X-rays often reveal joint narrowing and bone spurs, characteristic of osteoarthritis. Treatment focuses on symptom management through weight management, exercise, pain relief strategies, and in severe cases, surgical interventions like joint replacement. By understanding these joint and cartilage problems, individuals can take proactive steps to address and alleviate the impact of osteoarthritis on their daily lives.
| Key Points | Details | Importance |
|---|---|---|
| Joint Deterioration | Gradual breakdown of cartilage in joints | Manage symptoms |
| Bone-on-Bone Issues | Direct contact between bone ends | Pain and reduced mobility |
| Excess Body Weight | Exacerbates osteoarthritis symptoms | Weight management crucial |
Effective Bone Health Treatments
Effective treatments for osteoporosis encompass a range of strategies, including lifestyle adjustments, medication options like Actonel and Fosamax, and surgical interventions such as kyphoplasty and vertebroplasty. When managing osteoporosis, it's essential to prioritize bone health through weight-bearing exercises and proper nutrition. Here are four key components of effective bone health treatments:
- Lifestyle Adjustments: Incorporating weight-bearing exercises into daily routines can help strengthen bones and reduce the risk of fractures associated with osteoporosis.
- Medication Options: Medications like Actonel and Fosamax are prescribed to slow down bone loss and improve bone density in individuals with osteoporosis.
- Calcium and Vitamin D Supplementation: Adequate calcium and vitamin D intake is crucial for maintaining bone health and supporting the effectiveness of other osteoporosis treatments.
- Surgical Interventions: Procedures such as kyphoplasty and vertebroplasty may be recommended to stabilize fractures and relieve pain in individuals with severe osteoporosis.
Consulting with a specialist can help tailor a treatment plan that addresses individual needs and ensures optimal management of osteoporosis.
Protecting Joints and Bones
Weight-bearing and strength training exercises play a crucial role in safeguarding bones and joints in both osteoporosis and osteoarthritis. Maintaining a healthy weight is essential to reduce joint stress and prevent bone loss in these conditions.
Implementing joint protection techniques and avoiding overuse can help alleviate symptoms and preserve joint function.
Bone Density Importance
Maintaining optimal bone density is a critical factor in safeguarding joint health and preventing the risks associated with osteoporosis and osteoarthritis. Here are four essential points to consider:
- Monitoring bone density is crucial for protecting joints and bones from the risks of osteoporosis and osteoarthritis.
- Low bone density can increase the likelihood of fractures in individuals with osteoporosis, impacting joint health.
- Bone density tests such as DXA scans offer vital information on bone strength and density, guiding preventive measures.
- Optimal bone density maintenance supports joint function and minimizes the effects of degenerative joint diseases.
Understanding bone density levels facilitates early detection and interventions for managing risks associated with osteoporosis and osteoarthritis.
Joint Mobility Exercises
Monitoring bone density is crucial for protecting joints and bones from the risks of osteoporosis and osteoarthritis. Incorporating joint mobility exercises is a key strategy in maintaining optimal joint health and function. Joint mobility exercises play a vital role in enhancing flexibility, reducing stiffness, and preserving range of motion, essential for managing osteoarthritis and osteoporosis.
Engaging in weight-bearing activities such as walking, dancing, or stair climbing can effectively strengthen bones and support overall joint health. Furthermore, gentle stretches and low-impact exercises like yoga or tai chi can improve balance and coordination, reducing the risk of falls and injuries.
Regular physical activity is imperative for sustaining joint function and preventing bone loss in individuals with osteoarthritis and osteoporosis.
Tips for Better Bone Health
To optimize bone health, it's crucial to prioritize a balanced diet rich in calcium and vitamin D to support bone strength and density. Here are four tips for better bone health:
- Ensure Adequate Calcium and Vitamin D Intake: Incorporate dairy products, leafy greens, and fortified cereals into your diet to support bone density and reduce the risk of hip fractures.
- Engage in Weight-Bearing Exercises: Activities like walking, dancing, or weightlifting can help strengthen bones and lower the chances of developing osteoporosis.
- Avoid Smoking and Limit Alcohol: These habits can weaken bones, increasing the risk of fractures. By cutting down on smoking and moderating alcohol intake, you can maintain bone health.
- Incorporate Resistance and Balance Training: Including resistance exercises and balance training in your routine can enhance muscle strength and stability, reducing the likelihood of falls and fractures.
Frequently Asked Questions
What Is Difference Between Osteoarthritis and Osteoporosis?
When comparing osteoarthritis and osteoporosis, it's crucial to note that osteoarthritis primarily affects joints, leading to pain and reduced mobility, while osteoporosis is characterized by low bone mass, increasing fracture risk.
This distinction is vital in understanding the differing impacts these conditions have on the body. By recognizing these differences, healthcare providers can tailor treatments to address each condition effectively.
What Are the 4 Stages of Osteoarthritis?
In the realm of osteoarthritis, the progression unfolds through four distinct stages: mild, moderate, severe, and end-stage. Each stage showcases varying degrees of joint cartilage degradation, resulting in escalating levels of pain, stiffness, and reduced mobility.
From the initial mild discomfort to the debilitating end-stage symptoms necessitating surgical remedies, the journey through these phases underscores the impactful nature of osteoarthritis on joint health.
What Are 5 Symptoms of Osteoporosis?
We can't stress enough the importance of recognizing the symptoms of osteoporosis. These signs can include back pain, height loss, a stooped posture, and bone fractures from minor stress.
Fractures often affect the spine, hip, or wrist. As bone fragility increases, so does the risk of fractures. Osteoporosis is stealthy; it may hide until a sudden break shows its presence.
Early detection is key for managing this condition.
What Is the Difference Between Osteoporosis and Degenerative Bone Disease?
When comparing osteoporosis to degenerative bone diseases, the key difference lies in the areas they affect. Osteoporosis primarily impacts bone strength and density, leading to increased fracture risk.
In contrast, degenerative bone diseases like osteoarthritis target joint function and mobility, resulting in pain and stiffness.
Understanding these distinctions is crucial for accurate diagnosis and appropriate treatment interventions to improve patient outcomes and quality of life.
Conclusion
In conclusion, the stark contrast between osteoporosis and osteoarthritis is undeniable. While osteoporosis threatens to turn our bones into fragile, brittle shells waiting to shatter at the slightest touch, osteoarthritis mercilessly attacks our joints, causing excruciating pain and stiffness.
Understanding the nuances of these conditions is crucial in managing and treating them effectively. Let's arm ourselves with knowledge and take proactive steps to protect our bones and joints for a healthier future.