When thinking about the complex network of factors affecting bone health, it is crucial not to ignore the mysterious nature of secondary osteoporosis.
The implications of underlying conditions and their impact on bone density are far-reaching, warranting a closer examination of this silent yet significant condition.
As we explore the complexities of secondary osteoporosis, a deeper understanding emerges, shedding light on the subtle yet profound ways it can affect individuals.
Key Takeaways
- Glucocorticoids disrupt bone remodeling, increasing fracture risk.
- Weight-bearing exercises and calcium support bone health.
- Collaboration with hematologists crucial for holistic care.
- Routine screenings and lifestyle modifications are essential for bone health.
Metabolic Bone Disease
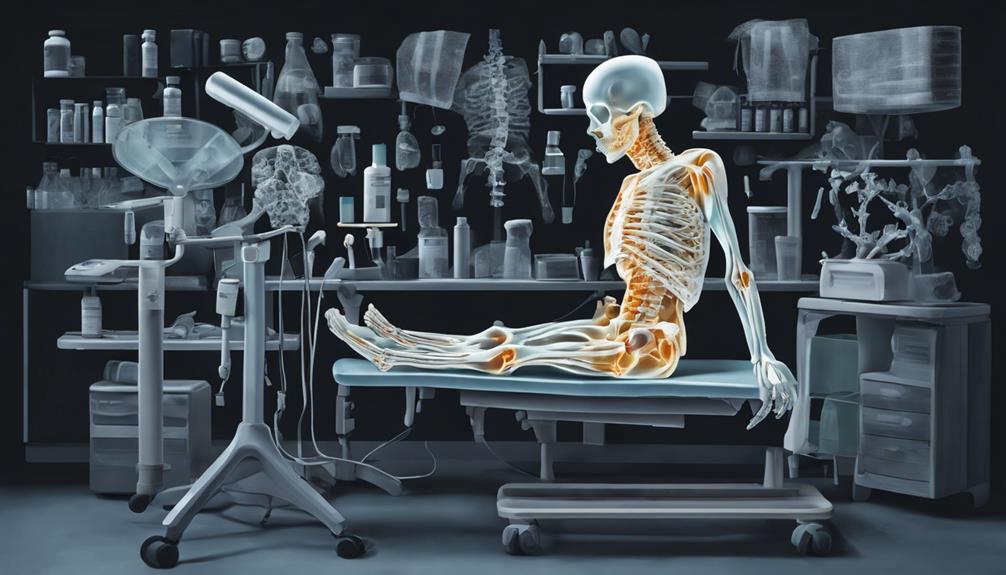
In Metabolic Bone Disease, our bones undergo structural changes due to various factors, impacting their strength and density significantly. This condition affects both bone quantity and quality, leading to an increased risk of fractures. Bone quantity refers to the amount of bone tissue present in the body, while bone quality encompasses factors like bone microarchitecture, mineralization, and collagen composition. These alterations in bone quantity and quality weaken the overall structural integrity of the bones, making them more prone to fractures even with comparable bone mineral density levels to primary osteoporosis.
Fractures are a significant concern in Metabolic Bone Disease as the compromised bone strength and density make individuals more susceptible to bone breaks, especially in weight-bearing bones such as the hips, spine, and wrists. These fractures can severely impact an individual's mobility, independence, and overall quality of life. Therefore, early detection and management of Metabolic Bone Disease are crucial to prevent the progression of bone deterioration and reduce the risk of fractures.
Glucocorticoid-Induced Osteoporosis

Glucocorticoid-induced osteoporosis poses a significant challenge due to the detrimental effects of glucocorticoids on bone health. These medications disrupt the delicate balance of bone remodeling by increasing resorption and decreasing formation, leading to an increased risk of fractures.
Understanding the mechanisms behind glucocorticoid-induced bone loss, identifying key risk factors, and implementing effective prevention strategies are crucial in managing this form of secondary osteoporosis.
Glucocorticoid Mechanisms Explained
Exerting their impact on bone remodeling processes, glucocorticoids disrupt the delicate balance between bone resorption and formation in individuals susceptible to glucocorticoid-induced osteoporosis. Glucocorticoid effects include inhibiting gonadal hormone production and corticotrophin secretion, leading to increased bone resorption and decreased bone formation.
Even low doses of glucocorticoids can cause reversible bone loss in young patients, significantly affecting bone health. Furthermore, glucocorticoids suppress osteoblast function and enhance osteoclast-mediated bone resorption, contributing to bone loss.
Patients with glucocorticoid-induced osteoporosis face a higher fracture risk compared to those with postmenopausal osteoporosis at similar bone mineral density levels. Understanding these mechanisms is crucial for effective management and prevention strategies in individuals affected by glucocorticoid-induced osteoporosis.
Risk Factors Overview
Understanding the risk factors associated with glucocorticoid-induced osteoporosis is essential for developing targeted prevention and management strategies in affected individuals. This condition, characterized by increased bone resorption and decreased bone formation, poses a significant risk of fractures, surpassing that of postmenopausal osteoporosis.
Here are five key risk factors to consider:
- Prolonged use of glucocorticoids at any dose can impact bone remodeling.
- Patients on glucocorticoids are at a higher risk of fractures even with comparable bone mineral density levels.
- Glucocorticoids can cause reversible bone loss, particularly in young patients.
- Even low doses of prednisone can lead to considerable bone loss, affecting bone metabolism and growth factors.
- Effective management strategies for glucocorticoid-induced osteoporosis include monitoring bone density, making lifestyle modifications, and utilizing specific FDA-approved medications.
Prevention Strategies Outlined
To effectively mitigate the impact of glucocorticoid therapy on bone health, comprehensive prevention strategies encompassing calcium and vitamin D supplementation, weight-bearing exercises, and regular bone mineral density monitoring are imperative. Calcium and vitamin D play crucial roles in supporting bone health and can help offset the bone loss associated with glucocorticoid use. Weight-bearing exercises, such as walking or strength training, are essential for enhancing bone strength and reducing fracture risk. Regular monitoring of bone mineral density is vital for early detection and intervention in glucocorticoid-induced osteoporosis. By combining these strategies with lifestyle modifications like avoiding smoking and excessive alcohol consumption, individuals can proactively manage their bone health while on glucocorticoid therapy.
| Prevention Strategies | Description |
|---|---|
| Calcium and Vitamin D | Supplementation supports bone health and counteracts bone loss from glucocorticoids. |
| Weight-Bearing Exercises | Promote bone strength and decrease fracture risk in individuals on glucocorticoid therapy. |
| Regular Monitoring | Crucial for early detection and management of glucocorticoid-induced osteoporosis. |
Heritable Connective Tissue Disorders

Heritable connective tissue disorders, such as osteogenesis imperfecta, can significantly impact bone health, leading to secondary osteoporosis characterized by specific skeletal abnormalities. Skeletal dysplasia is a common feature in these disorders, affecting bone structure and overall health.
Here are some key points related to heritable connective tissue disorders:
- Osteogenesis imperfecta can present with features like osteoporosis, bowed long bones, and compressed vertebrae.
- Skeletal dysplasia plays a crucial role in impacting bone health in individuals with heritable connective tissue disorders.
- Bone biopsies are valuable diagnostic tools, aiding in the detection of conditions such as myeloma and mastocytosis through malignant marrow infiltration assessment.
- Mastocytosis diagnosis relies on identifying excessive mast cell infiltration in tissues, contributing to bone health complications.
- Hemochromatosis diagnosis can be supported by positive iron staining in bone biopsies, highlighting its effects on bone metabolism and health.
Use of Bone Biopsies in Diagnosis

Bone biopsies play a pivotal role in accurately diagnosing secondary osteoporosis by detecting underlying conditions such as osteogenesis imperfecta, myeloma, mastocytosis, and hemochromatosis. These biopsies provide valuable insights into the specific pathology of the bone, aiding in targeted treatment strategies and management.
Biopsy Accuracy in Diagnosis
How accurately can bone biopsies detect conditions contributing to secondary osteoporosis such as myeloma, mastocytosis, and hemochromatosis?
Bone biopsies are pivotal in diagnosing underlying conditions that lead to secondary osteoporosis. Here are some key points to consider:
- Bone biopsies can accurately identify myeloma infiltration in the bone marrow.
- Mastocytosis diagnosis relies on detecting excessive mast cell infiltration in bone tissue through biopsies.
- Positive iron staining results from bone biopsies are crucial for diagnosing hemochromatosis.
- Lymphocytosis, revealed through bone biopsies, can be associated with osteoporosis in specific cases.
- Biopsies play a significant role in confirming the presence of malignant marrow infiltration in conditions affecting bone health.
Biopsy Procedure Benefits
In understanding the benefits of bone biopsies, it becomes evident that these procedures are instrumental in accurately diagnosing and managing conditions that contribute to secondary osteoporosis. Bone biopsies play a significant role in detecting malignant marrow infiltration seen in conditions such as myeloma and mastocytosis.
They're particularly useful in mastocytosis, where excessive mast cell infiltration aids in diagnosis. Furthermore, bone biopsies are crucial in diagnosing hemochromatosis as they rely on positive iron staining. Conditions like lymphocytosis, associated with osteoporosis, can also be identified through bone biopsies.
Hematologic Disease
Understanding the hematologic implications in secondary osteoporosis is essential for thorough diagnostic assessments and effective treatment strategies. Hematologic diseases such as myeloma and mastocytosis can significantly impact bone health, leading to secondary osteoporosis. Here are some key points to consider:
- Bone biopsies play a crucial role in detecting malignant marrow infiltration in hematologic diseases affecting bone health.
- The diagnosis of mastocytosis relies on identifying excessive mast cell infiltration, while myeloma diagnosis involves specific bone biopsy findings.
- Conditions like lymphocytosis can also be associated with osteoporosis due to their detrimental effects on bone health.
Comprehensive understanding of the hematologic aspects of secondary osteoporosis is vital for accurate diagnosis and effective management. Collaborating with hematologists and other specialists is important in cases where hematologic diseases contribute to secondary osteoporosis, ensuring a holistic approach to patient care.
Corticosteroids and Vitamin D Metabolism

Corticosteroid administration has been shown to disrupt calcium absorption, induce hypercalciuria, and impact vitamin D metabolism and bone cell function. The effects of corticosteroids on bone health are multifaceted, with implications for bone remodeling and overall skeletal integrity.
Glucocorticoids, a common type of corticosteroid, have been linked to decreased bone remodeling and altered osteoblast function, potentially leading to bone loss. Despite some conflicting findings regarding vitamin D levels in corticosteroid-treated individuals, it's evident that even low doses of glucocorticoids can influence bone remodeling processes.
This impact is particularly concerning in younger individuals, where bone loss may be reversible upon discontinuation of corticosteroid therapy. Understanding the complexities of corticosteroid effects on vitamin D metabolism and bone remodeling is crucial for effective management of secondary osteoporosis.
Further research is needed to clarify the mechanisms underlying these interactions and to develop targeted interventions to mitigate bone-related complications associated with corticosteroid use.
Mechanisms of Glucocorticoid Osteoporosis

Glucocorticoid-induced osteoporosis disrupts the delicate balance of bone remodeling by enhancing bone resorption while simultaneously decreasing bone formation.
This imbalance is primarily driven by glucocorticoids' suppressive effects on osteoblast function and their promotion of osteoclast-mediated bone resorption.
The intricate mechanisms through which glucocorticoids exert their detrimental effects on bone metabolism warrant a closer examination to devise targeted therapeutic interventions.
Glucocorticoid Effects on Bone
In the context of bone health, the impact of glucocorticoids on bone remodeling mechanisms is profound, characterized by increased bone resorption and decreased bone formation disrupting the delicate balance of bone turnover.
- Glucocorticoids increase bone resorption and decrease bone formation, exacerbating the risk of fractures.
- They inhibit gonadal hormone production and corticotrophin secretion, further compromising bone health.
- Even low doses of glucocorticoids can result in reversible bone loss in young patients.
- The risk of fractures is higher in glucocorticoid-induced osteoporosis compared to postmenopausal osteoporosis at similar bone mineral density levels.
- Glucocorticoids influence osteoblast function and collagen synthesis, contributing to altered bone remodeling processes.
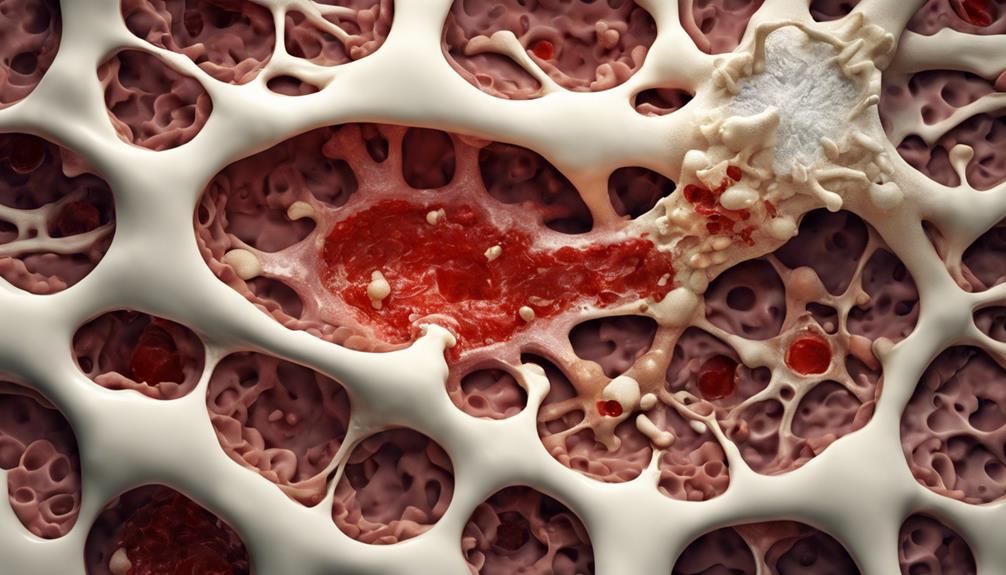
Increased Bone Resorption
How do glucocorticoids specifically contribute to the increased bone resorption observed in osteoporosis associated with their use?
Glucocorticoid-induced osteoporosis accelerates bone resorption by impairing osteoblast function and promoting osteoclast activity, leading to net bone loss. By inhibiting bone formation and reducing bone mineral density, corticosteroids elevate the risk of fractures in affected individuals.
Furthermore, glucocorticoids disrupt bone remodeling processes by interfering with gonadal hormone production and corticotrophin secretion, exacerbating bone resorption. Even at low doses, these medications can induce reversible bone loss in younger patients by perturbing normal bone metabolism.
The heightened fracture susceptibility seen in individuals on glucocorticoid therapy underscores the significant impact of bone resorption in this population compared to postmenopausal osteoporosis.
Epidemiology of Secondary Osteoporosis

The epidemiology of secondary osteoporosis reveals a significant global burden, with over 8 million fractures attributed to this condition worldwide annually. Here are five key points to consider regarding the epidemiology of secondary osteoporosis:
- The World Health Organization reports that osteoporosis affects 6% of men and 21% of women over 50 years old.
- Approximately 500 million individuals globally are impacted by osteoporosis, emphasizing the widespread reach of this condition.
- Endocrine disorders such as primary hyperparathyroidism and hyperthyroidism are known contributors to secondary osteoporosis.
- Chronic conditions like Cushing's syndrome, diabetes mellitus, and inflammatory diseases significantly increase the risk of fractures associated with secondary osteoporosis.
- Secondary osteoporosis poses a substantial public health concern due to its prevalence and the diverse range of underlying conditions that can lead to its development.
Understanding these aspects of the epidemiology of secondary osteoporosis is crucial for healthcare providers in effectively managing and preventing fractures in at-risk populations.
Secondary Causes of Osteoporosis
Secondary osteoporosis, stemming from various medical conditions or medications that disrupt new bone tissue formation, presents a complex interplay of factors contributing to decreased bone density. An imbalance between old bone loss and new bone production leads to this condition, increasing the risk of fractures. Immune system-affecting medications like antiretrovirals, central nervous system medications like anticonvulsants, and gastrointestinal medications like proton pump inhibitors can all contribute to secondary osteoporosis. Risk factors such as smoking, excessive alcohol consumption, hyperthyroidism, and malabsorption can exacerbate bone loss in individuals with secondary osteoporosis. Early diagnosis and management of underlying causes are crucial in addressing this condition to prevent complications like fractures.
| Factors Contributing to Secondary Osteoporosis | Examples |
|---|---|
| Medications disrupting bone tissue formation | Antiretrovirals, Anticonvulsants, Proton Pump Inhibitors |
| Medical conditions exacerbating bone loss | Hyperthyroidism, Malabsorption, Smoking, Excessive Alcohol Consumption |
Prevention and Management Strategies

To effectively address secondary osteoporosis, a comprehensive approach focusing on prevention and management strategies is essential. When considering prevention and management of secondary osteoporosis, several key strategies should be implemented:
- Maintaining Adequate Calcium and Vitamin D Intake: Ensuring sufficient calcium and vitamin D through diet or supplements is crucial for bone health and reducing the risk of osteoporosis.
- Addressing Underlying Medical Conditions: Managing underlying medical issues or adjusting medication regimens can help prevent further bone loss associated with secondary osteoporosis.
- Regular Bone Density Screenings: Routine screenings are vital for early detection and effective management of secondary osteoporosis by monitoring bone health status.
- Engaging in Weight-Bearing Exercises: Weight-bearing exercises help strengthen bones and improve bone density, reducing the likelihood of fractures in individuals with secondary osteoporosis.
- Avoiding Smoking and Excessive Alcohol Consumption: These lifestyle factors can contribute to bone loss and fracture risk, making it essential to avoid them for optimal bone health and osteoporosis prevention.
Frequently Asked Questions
How Long Is Life Expectancy With Spinal Osteoporosis?
Life expectancy with spinal osteoporosis can vary based on factors like disease severity, treatment efficacy, and individual health. Vertebral fractures from osteoporosis may impact mobility and quality of life, affecting longevity. Early detection and proper management can improve outcomes.
Treatment strategies aim to prevent fractures, manage pain, and maintain bone health for a better quality of life. Regular monitoring and adherence to treatment plans may support a longer life expectancy.
Can Vitamin D Reverse Osteoporosis?
Yes, vitamin D can play a crucial role in managing osteoporosis by aiding in calcium absorption and bone mineralization. Adequate levels of vitamin D are essential for maintaining bone density and reducing the risk of fractures.
While vitamin D supplementation can help improve bone density, it may not completely reverse established osteoporosis.
Consulting with a healthcare provider is recommended to determine the appropriate vitamin D supplementation for effective osteoporosis management.
What 3 Bones Are Most Affected by Osteoporosis?
The three bones most commonly affected by osteoporosis are the vertebrae of the spine, the hips, and the wrists. Osteoporosis can lead to compression fractures in the vertebrae, increasing the risk of height loss.
Hip bones are susceptible to fractures, with severe consequences.
Wrist bones, especially the distal radius, are prone to fractures, impacting daily activities.
These sites underscore the importance of prevention and treatment strategies.
Can You Have Osteoporosis and Never Break a Bone?
Absolutely, one can have osteoporosis without experiencing a bone fracture. This silent condition may go undetected until a fracture occurs. Fragile bones in osteoporosis heighten the risk of fractures from minor activities like sneezing or bending.
Early diagnosis through bone density screenings is vital to prevent fractures and manage the condition effectively. Proper management, including medication and lifestyle changes, can help reduce fracture risks even if osteoporosis is present.
Conclusion
In conclusion, the complexities of secondary osteoporosis require diligent evaluation and personalized intervention. Understanding the underlying mechanisms and risk factors is essential for effective prevention and management strategies.
By addressing metabolic bone disease, glucocorticoid-induced osteoporosis, and other contributing factors, we can strive to mitigate the impact of this silent disease.
Let's advocate for early detection and comprehensive care to combat the consequences of secondary osteoporosis.