As dementia progresses, hallucinations become more frequent and significant. They can impact our perception of reality and engage all of our senses, not just our vision. Conditions like Lewy body dementia and changes in the brain can play a role in shaping these hallucinatory experiences. Maintaining a consistent routine, offering reassurance, and creating a calming environment can help manage hallucinations in advanced dementia. Healthcare professionals can assist by monitoring symptoms and recommending non-pharmacological coping mechanisms. Caregivers play a crucial role in providing support and empathy. Understanding hallucinations is essential, and implementing effective strategies can benefit everyone involved. There is always more to discover in the realm of enhancing dementia care.
Key Takeaways
- Hallucinations in dementia often occur as the condition progresses.
- Increased frequency and intensity of sensory experiences mark later stages.
- Factors like Lewy body dementia and Alzheimer's disease can trigger hallucinations.
- Likelihood of experiencing hallucinations rises in advanced stages of dementia.
- Hallucinations may involve multiple senses, complicating care.
Early Signs of Hallucinations in Dementia
As dementia progresses, individuals may begin to experience early signs of hallucinations, such as visual disturbances or misinterpretations of reality. These early signs can be vital for both the individual and their caregivers. Visual disturbances may include seeing things that aren't there, like shadows moving or objects appearing distorted. Misinterpretations of reality can lead to confusion about the environment, causing distress or fear.
Changes in brain function play a significant role in these sensory experiences. The cognitive decline associated with dementia can disrupt the brain's ability to process information accurately, leading to the perception of things that aren't real. As the disease advances, hallucinations can manifest in various senses, not just visual. Individuals may also report hearing things that have no external source, adding another layer of complexity to their experiences.
Understanding these early signs of hallucinations in dementia is essential for providing appropriate care and support to individuals affected by the disease. By recognizing and addressing these symptoms early on, caregivers can help manage the challenges that come with cognitive decline and sensory disturbances.
Progression of Hallucinations in Dementia

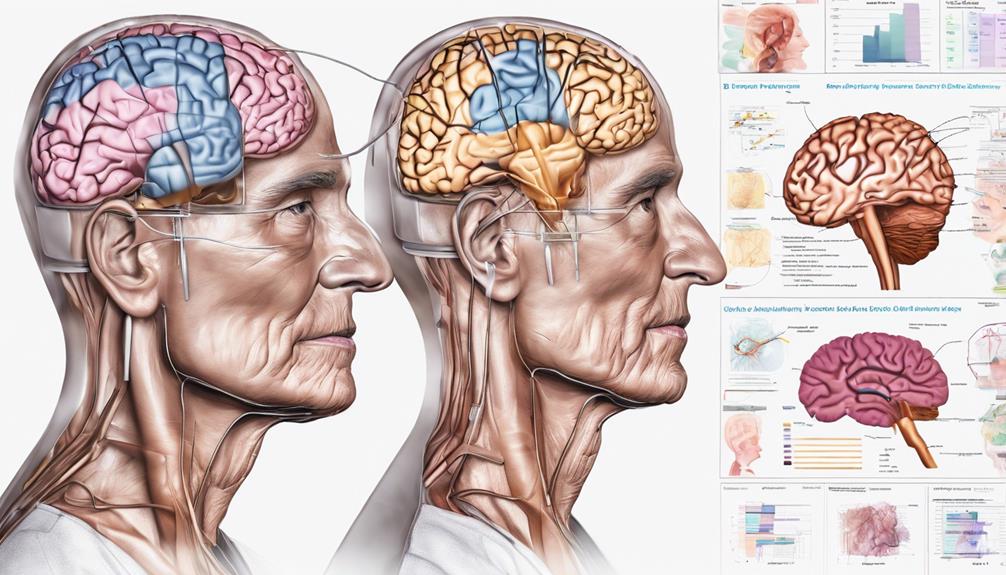
Hallucinations in dementia progress significantly as the disease advances, particularly manifesting in heightened frequency and intensity of sensory experiences. In the middle to later stages of Alzheimer's and other forms of dementia, when significant brain changes occur, individuals may start experiencing visual hallucinations more frequently.
It's estimated that around 30% of Alzheimer's patients may encounter dementia-related psychosis, which often involves seeing things that aren't there. As dementia progresses, the frequency and intensity of these hallucinations tend to increase, affecting how individuals perceive reality. Additionally, these hallucinations can involve various senses, such as auditory, olfactory, tactile, and gustatory experiences, reflecting complex changes in the brain.
These sensory hallucinations can be distressing for both the individual and their caregivers. Therefore, it becomes essential to provide tailored support and management strategies as the disease evolves to help individuals cope with these challenging experiences.
Factors Influencing Hallucinations in Dementia
With the progression of dementia, various factors come into play that influence the occurrence and intensity of hallucinations experienced by individuals. Conditions such as Lewy body dementia and Parkinson's disease can heighten the chances of experiencing hallucinations. These hallucinations may stem from disruptions in the brain’s normal processing of information, particularly when there are changes in certain neurotransmitter systems. Atypical parkinsonism explained, refers to conditions that present with similar movement difficulties seen in Parkinson’s disease, but are often accompanied by additional symptoms like cognitive decline and more frequent hallucinations. Understanding these variations helps in managing both the motor and non-motor symptoms more effectively. Furthermore, understanding atypical parkinsonism is crucial for caregivers and medical professionals in providing accurate care, as these conditions may require tailored therapeutic approaches. Early recognition of the cognitive and psychiatric symptoms, alongside motor difficulties, allows for more comprehensive management strategies, helping to improve the quality of life for those affected.
In Alzheimer's disease, as brain cells deteriorate and cognitive functions decline, hallucinations may manifest. These visual or auditory perceptions can be triggered by neurotransmitter imbalances caused by abnormal protein buildup in the brain.
Hallucinations in dementia can involve multiple senses and tend to become more frequent as the disease advances. Providing support and care to individuals experiencing hallucinations is essential in managing their symptoms and ensuring their well-being.
Understanding the impact of these factors on hallucinations in dementia is vital for caregivers and healthcare providers to deliver appropriate care and support to those affected by the disease. By recognizing these influences, we can better assist people in dealing with the challenges associated with hallucinations in advanced dementia.
Managing Hallucinations in Advanced Dementia

In advanced dementia, our focus shifts towards creating a secure and tranquil environment to effectively manage hallucinations experienced by individuals. When dealing with hallucinations in advanced dementia, it's important to remember the following:
- Provide constant reassurance: Individuals experiencing visual hallucinations may feel frightened or confused. Offering reassurance and a comforting presence can help alleviate their distress.
- Maintain a consistent routine: Consistency in daily activities and environment can provide a sense of stability for individuals with advanced dementia. Predictability can help reduce anxiety and the likelihood of hallucinations.
- Implement calming strategies: Techniques such as soothing music, gentle lighting, and familiar objects can contribute to a peaceful atmosphere. Creating a safe and serene space is essential in managing hallucinations without resorting to medication.
Role of Healthcare Professionals in Hallucinations
Healthcare professionals play an essential role in recognizing and addressing hallucinations among individuals with dementia, guiding personalized care plans, and optimizing treatment outcomes. When working with dementia patients experiencing hallucinations, healthcare professionals assess the frequency and severity of these symptoms to determine the most appropriate interventions. By collaborating with caregivers, they develop personalized care plans tailored to managing hallucinations effectively. Monitoring medication effectiveness and potential side effects is crucial in optimizing treatment outcomes for patients. Furthermore, healthcare professionals provide valuable guidance on non-pharmacological approaches that can help reduce hallucinations and enhance the quality of life for individuals with dementia. Through a holistic approach that considers both pharmacological and non-pharmacological interventions, healthcare professionals aim to enhance the overall well-being of dementia patients and support their caregivers.
| Healthcare professionals | Role in Hallucinations | Impact |
|---|---|---|
| Assessing symptoms | Determining appropriate interventions | Improved quality of life |
| Collaborating with caregivers | Developing personalized care plans | Enhanced patient well-being |
| Monitoring medication | Optimizing treatment outcomes | Better symptom management |
| Providing guidance | Non-pharmacological approaches | Reduced hallucinations |
| Evaluating effectiveness | Ensuring personalized care plans | Support for caregivers |
Impact of Hallucinations on Caregivers

Experiencing hallucinations in individuals with dementia can greatly impact the well-being and stress levels of caregivers. Here are three ways in which hallucinations can affect caregivers:
- Essential Strain: Caregivers often experience heightened emotional strain when managing hallucinations in dementia patients. Witnessing a loved one going through distressing hallucinations can be emotionally challenging and draining.
- Communication Obstacles: Hallucinations can lead to communication difficulties between caregivers and individuals with dementia. Understanding and responding to the hallucinations require patience and effective communication strategies to provide proper care and support.
- Heightened Stress: Managing hallucinations in dementia patients can significantly increase the stress levels of caregivers. The constant vigilance and need for quick responses to the hallucinations can lead to overwhelming stress, requiring caregivers to seek additional support and interventions to cope effectively.
In order to support caregivers in handling the impact of hallucinations in dementia patients, it's essential to provide them with the necessary tools, resources, and guidance to navigate these challenges with resilience and compassion.
Seeking Support for Dementia-Related Hallucinations

Addressing the challenges of managing hallucinations in individuals with dementia requires proactive seeking of support and understanding. As dementia progresses to later stages, the likelihood of experiencing dementia-related hallucinations, particularly visual ones, increases. Approximately 30% of people with Alzheimer's may encounter these hallucinations, which can involve multiple senses, adding to the complexity of care. Caregivers play a vital role in providing support and empathy to individuals affected by these hallucinations. Seeking support becomes essential not only for the well-being of the individual with dementia but also for the caregivers who may feel overwhelmed by the progression of the disease.
Understanding the nature of dementia-related hallucinations and learning effective strategies to address them can greatly benefit both the individual and their caregiver. By seeking support from healthcare professionals, support groups, and educational resources, caregivers can gain valuable insights and techniques to navigate these challenging experiences with compassion and patience. Remember, you aren't alone in this journey, and seeking support is a proactive step towards providing the best care possible for those affected by dementia-related hallucinations.
Frequently Asked Questions
What Stage of Dementia Do Hallucinations Occur?
Hallucinations in dementia can occur in later stages as cognitive function declines. Visual hallucinations, seeing things that aren't there, are frequent in advanced dementia. Changes in the brain due to Alzheimer's progression may trigger hallucinations.
What Is the Most Common Type of Hallucination for a Person With Dementia?
Visual hallucinations are the most common type experienced by individuals with dementia. They often involve seeing things that aren't there. As dementia progresses, these hallucinations may become more frequent, impacting the individual's perception of reality.
What Stage Is Delusions in Dementia?
Delusions in dementia typically manifest in later stages, leading to fixed false beliefs like persecution or altered identity. Addressing these requires medical evaluation, patience, and tailored support to enhance well-being and quality of life for individuals.
What Stage of Dementia Is Hiding Things?
In the mid to late stages of dementia, hiding things often emerges as memory loss and confusion worsen. This behavior can result from various factors, like memory issues or paranoia. Caregivers may need creative solutions to address this distressing behavior.
Conclusion
As dementia progresses, hallucinations can occur at different stages, impacting both the individual and their caregivers. Understanding the early signs, progression, and factors influencing hallucinations is essential for managing them effectively.
Healthcare professionals play a key role in providing support and guidance for those experiencing dementia-related hallucinations. Caregivers must also seek support and resources to navigate the challenges that come with caring for someone with dementia.
Stay informed and proactive to guarantee the best possible care for your loved one.