Caregiver Support
Understanding the Different Stages of Dementia
Journey through the stages of dementia to unravel the complexities of cognitive decline and the evolving care needs – discover more insights ahead.
Understanding the different stages of dementia is essential for providing proper care. This condition progresses gradually through distinct stages marked by shifts in cognitive abilities. In the mild stage, one may experience memory lapses and challenges. The moderate stage shows more pronounced symptoms like confusion. Severe dementia displays profound loss of response and communication abilities. Symptoms vary from cognitive decline to behavioral changes. Tailored care is vital, adapting to changing needs. Encourage independence in early stages and offer complete care in advanced stages. Remember, each stage requires specialized attention. More insights await to deepen your understanding further.
Key Takeaways
- Dementia progresses through mild, moderate, and severe stages with distinct symptoms.
- Mild stage features memory lapses and mild challenges in daily functioning.
- Moderate stage shows pronounced confusion, mood changes, and sleep disturbances.
- Severe stage exhibits profound cognitive decline, communication struggles, and physical limitations.
- Tailored care and support are crucial at each stage to meet changing needs effectively.
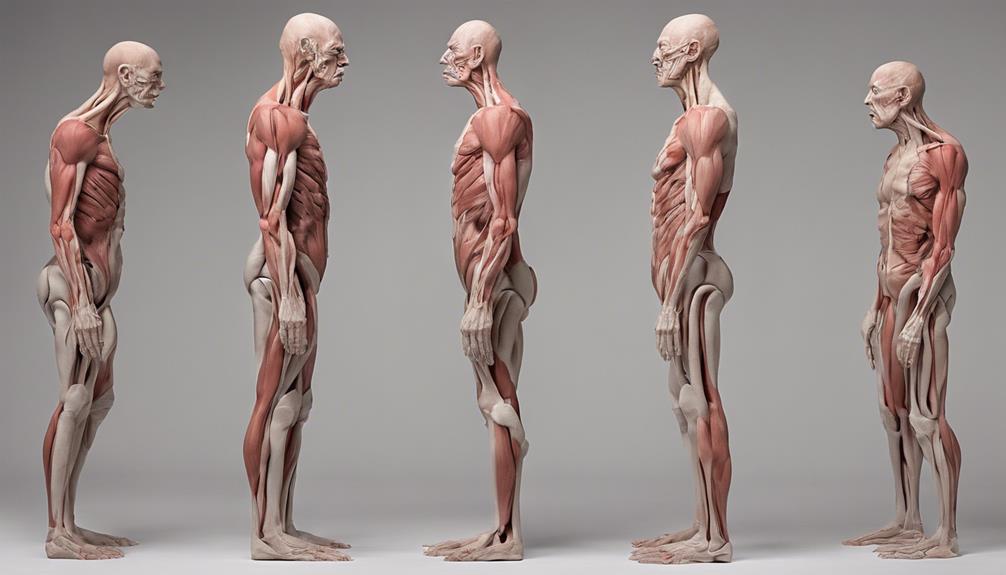
Progression of Dementia Stages
As we observe individuals affected by dementia, we witness a gradual progression through distinct stages, each marking a significant shift in cognitive abilities and daily functioning. The progression of dementia stages is important to understand as it impacts how we provide care and support to those with the condition.
From the early stages where individuals may experience mild forgetfulness and confusion to the late stages where they may lose the ability to communicate and perform daily tasks, the journey through dementia stages is marked by noticeable changes in symptoms and characteristics.
Diagnosis usually occurs around stage 4 of dementia when symptoms become more pronounced, and the need for support becomes more evident. It's important to recognize these stages to make sure appropriate care and interventions are in place. While the progression of dementia stages varies among individuals, having a clear understanding of the different stages helps us tailor our support to meet the specific needs of each person affected by dementia.
Mild Stage of Dementia

Moving through the stages of dementia, the mild stage presents individuals with memory lapses and challenges in tasks such as planning and organizing in social and work settings. In this early stage, forgetfulness may occur after reading or misplacing items, making cognitive impairments noticeable. People in the mild stage might have difficulty finding the right words or recalling object locations. Despite these mild symptoms, individuals may still be able to function independently in certain aspects of daily life. To better understand the characteristics of the mild stage of dementia, let's explore the following table:
| Mild Stage of Dementia Symptoms |
|---|
| Memory lapses |
| Challenges in planning and organizing tasks |
| Forgetfulness after reading |
| Difficulty recalling object locations |
In this stage, it's essential to provide support and understanding to those experiencing these challenges, helping them navigate through their daily activities with patience and compassion.
Moderate Stage of Dementia
Moving through the moderate stage of dementia brings about more pronounced symptoms such as confusion and mood changes for individuals. Memory loss becomes more severe, affecting personal information like addresses and phone numbers. Sleep patterns may also shift, leading to restlessness and wandering tendencies.
During this stage, caregivers should consider respite care options to provide temporary breaks and support. The moderate stage of dementia requires longer duration and increased attention compared to earlier stages. It's essential to monitor individuals closely, ensuring their safety and well-being.
Encouraging a calming environment and maintaining a consistent routine can help alleviate some of the distress caused by the heightened symptoms. Understanding the challenges that come with the moderate stage of dementia is vital for providing effective care and support. By staying informed and seeking assistance when needed, caregivers can navigate this stage with patience and compassion.
Severe Stage of Dementia

Entering the severe stage of dementia brings about a profound loss of response to the environment and communication for individuals. In this stage, movement control is severely impaired, making daily activities such as walking and swallowing challenging. Awareness of recent experiences and surroundings diminishes drastically, making it difficult for individuals to understand their environment. Communication becomes a struggle, and individuals may find it hard to express pain or discomfort, highlighting the need for attentive caregiving.
Moreover, those in the severe stage of dementia are more vulnerable to infections, particularly pneumonia, due to their weakened immune systems and decreased ability to fight off illnesses. This vulnerability emphasizes the importance of close monitoring and timely medical care to prevent complications.
Understanding and providing care for individuals in the severe stage of dementia require patience, compassion, and specialized attention. By being aware of their needs and ensuring a safe and comfortable environment, caregivers can support these individuals in their daily struggles and provide the necessary assistance to maintain their well-being.
Symptoms in Different Stages
As dementia progresses through its stages, symptoms manifest in varying degrees of cognitive decline and behavioral changes. In the early stages, individuals may experience memory impairment, such as forgetfulness and difficulty with planning.
As the disease advances to the middle stages, pronounced confusion, mood changes, and trouble recalling personal information become more prominent. Communication difficulties may also arise during this phase.
In late-stage dementia, there's severe loss of response to the environment, along with significant physical decline. Walking difficulties, swallowing problems, and vulnerability to infections like pneumonia are common in this stage. It's important to provide appropriate care and support to individuals with late-stage dementia as they face these challenges.
Understanding the progression of symptoms throughout the stages of dementia is essential for caregivers and healthcare professionals to provide the best possible care for those affected by this condition.
Care Considerations for Each Stage

When caring for individuals in different stages of dementia, it's essential to adapt our approach to meet their changing needs.
In the early stages, providing support while encouraging independence can help maintain a sense of self-sufficiency.
As the disease progresses to advanced stages, more complete care and assistance become necessary to guarantee the individual's safety and well-being.
Early Stage Care
During the early stage of dementia, we focus on providing tailored support for memory-related challenges while fostering independence in daily activities. Individuals may experience memory lapses, forgetfulness, and difficulties in social settings. Caregivers should offer reminders and emotional support while monitoring changes in cognitive abilities. It's essential to help with object locations and assist in planning for future care needs. Below is a table summarizing key aspects of early stage care:
| Care Aspect | Description |
|---|---|
| Memory Challenges | Help with forgetfulness and word recall |
| Independence | Encourage self-reliance in daily tasks |
| Emotional Support | Provide comfort and reassurance |
| Planning | Assist in organizing and planning future activities |
| Cognitive Abilities | Monitor changes in cognitive functions |
Advanced Stage Support
In advanced stage dementia, we prioritize specialized care to address severe cognitive decline and physical limitations. At this stage, individuals require assistance with basic activities of daily living, such as eating, bathing, and dressing. Ensuring their comfort, safety, and quality of life becomes paramount. Vital care plays a critical role in managing symptoms and enhancing their overall well-being.
Caregivers need additional support and education to provide best care for those in late-stage dementia. It's essential to create a supportive environment that promotes dignity and respect for the individual. By focusing on specialized care, we can help individuals navigate the challenges of advanced stage dementia with compassion and understanding.
Frequently Asked Questions
How Long Does Dementia Take to Progress?
Dementia progression time varies widely based on factors such as age, health, and type of dementia. It's unpredictable, with some individuals living 4 to 8 years post-diagnosis, while others may endure up to 20 years.
At What Stage of Dementia Do They Sleep a Lot?
In the late stages of dementia, we notice increased daytime sleepiness and longer napping periods. Excessive sleeping can affect daily activities and quality of life. Monitoring changes in sleep patterns and promoting consistent routines can help manage this symptom.
At What Stage of Dementia Does Aggression Occur?
Aggression in dementia typically surfaces during the middle to late stages. Triggers like confusion and fear can lead to verbal or physical outbursts. Calm environments and personalized strategies help manage aggression effectively, enhancing the well-being of individuals.
What Causes Dementia Patients to Suddenly Get Worse?
When dementia patients suddenly worsen, factors like infections, changes in medication, dehydration, stress, hospitalization, or caregiver burnout could be culprits. It's essential to address triggers promptly to provide the best care and support for these individuals.
Which Type of Bathroom Option is More Suitable for Each Stage of Dementia?
At various dementia stages, safety and accessibility dictate bathroom choices. The walkin tub versus walkin shower debate often hinges on specific needs—tubs may aid those needing assisted baths, while showers offer quicker access for others with mobility aids, ensuring a secure and dignified bathing experience at every stage.
Conclusion
To summarize, understanding the various stages of dementia is essential for providing appropriate care and support to individuals living with this condition.
As the saying goes, 'knowledge is power,' and knowing what to expect at each stage can help families and caregivers navigate the challenges ahead with confidence and compassion.
By staying informed and being proactive in addressing the needs of those with dementia, we can make a positive difference in their quality of life.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Caregiver Support
How to Address the Top 7 Dementia Behaviors
Journey through effective strategies to address the top 7 dementia behaviors, uncovering triggers and communication techniques along the way.

To address the top seven dementia behaviors, we need to understand triggers and use effective communication strategies. Be aware of environmental changes and emotional factors that can influence behaviors. Set a positive mood through body language and clear, simple words. Manage wandering by ensuring safety and a secure environment. Handle incontinence by monitoring fluid intake and seeking healthcare guidance. When faced with agitation or paranoia, stay calm and seek professional help if needed. Manage sleep issues by maintaining a bedtime routine and addressing medical conditions affecting sleep. These strategies are essential in providing proper care for dementia patients.
Key Takeaways
- Identify triggers such as environmental changes and unmet needs.
- Use positive communication strategies to create a supportive environment.
- Implement safety measures to manage wandering behavior effectively.
- Address incontinence challenges through proper fluid management and hygiene practices.
- Employ calming techniques to manage agitation, aggression, and paranoia symptoms.
Understanding Dementia Behavior Triggers
We often encounter various triggers that can influence dementia behaviors, such as environmental changes, emotional factors, and unmet needs. Environmental triggers like loud noises or unfamiliar surroundings can lead to overstimulation and confusion in individuals with dementia. Emotional triggers, such as feeling scared or frustrated, may result in challenging behaviors like agitation or aggression. Unmet needs, like hunger or thirst, can also manifest as problematic behaviors. Caregivers play an important role in identifying and addressing these triggers to help manage challenging behaviors effectively.
Understanding the individual's routine, preferences, and past experiences is essential in recognizing potential triggers. Changes in routine can be particularly triggering for individuals with dementia, leading to feelings of disorientation or anxiety. By creating a calm and familiar environment, minimizing noise, and avoiding overstimulation, caregivers can help reduce the likelihood of challenging behaviors. Anticipating and addressing these triggers proactively can greatly improve the quality of care provided to individuals with dementia.
Communication Strategies for Dementia Care

When providing dementia care, effective communication strategies are essential for fostering understanding and connection with individuals experiencing cognitive decline. To communicate successfully with your loved one, consider the following strategies:
- Set a positive mood through body language and tone to create a welcoming environment for conversations.
- Minimize distractions and use nonverbal cues like gentle touches to attract their attention during interactions.
- State messages clearly using simple words and short sentences to aid comprehension.
- Ask straightforward, answerable questions to avoid confusion and encourage engagement.
- Listen attentively and patiently, both verbally and nonverbally, to show understanding and provide necessary support throughout the conversation.
These strategies can help improve communication with your loved one and enhance your relationship while addressing the challenges of dementia.
Managing Wandering in Dementia Patients
Addressing the issue of wandering in dementia patients requires essential safety measures and a secure environment to prevent potential risks and guarantee their well-being. Six out of 10 individuals with dementia may engage in wandering behavior, which can pose safety risks and present challenges for caregivers.
Wandering episodes can be triggered by changes in location, unmet needs, or sundowning episodes. To manage wandering, caregivers can implement safety measures such as using tracking devices and locking doors to prevent incidents. Involving neighborhood watch groups can also be beneficial in monitoring and ensuring the safety of wandering dementia patients.
Taking an important approach is essential to minimize the potential risks associated with wandering and provide a secure environment for individuals with dementia, promoting their overall well-being and safety. By being vigilant and implementing these strategies, caregivers can create a supportive and secure environment for dementia patients prone to wandering.
Addressing Incontinence Challenges

In managing incontinence challenges related to dementia, it's essential to focus on managing fluid intake and providing proper hygiene. Monitoring the amount of liquids consumed and ensuring regular bathroom visits can help in controlling incontinence issues.
Managing Fluid Intake
Understanding the importance of managing fluid intake is crucial in effectively addressing incontinence challenges commonly faced by individuals with dementia. Here are five key strategies to help manage fluid intake and incontinence:
- Providing regular bathroom reminders
- Creating a consistent toileting schedule
- Using absorbent products like adult diapers or pads
- Monitoring fluid intake and scheduling bathroom breaks
- Seeking guidance from healthcare professionals for specialized care plans.
Providing Proper Hygiene
To effectively manage incontinence challenges in individuals with dementia, establishing proper hygiene practices is essential for maintaining comfort and dignity. Incontinence affects up to 60-70% of those in later stages of dementia, making it essential to create a toileting schedule and provide access to suitable incontinence products.
Caregivers play a crucial role in monitoring hydration levels and offering frequent bathroom breaks to prevent accidents. Seeking professional guidance can provide valuable support in effectively managing incontinence in dementia care. By maintaining good hygiene practices, caregivers can help individuals with dementia feel more comfortable and maintain their dignity.
Coping With Agitation in Dementia

Addressing agitation in dementia requires a thorough understanding of the triggers and effective coping strategies to manage this challenging behavior. Agitation is common in about half of dementia patients in middle to later stages, often leading to verbal threats and physical aggression. Causes of agitation can vary from confusion and pain to frustration and reactions to medications.
To cope with agitation, it's essential to comprehend the patient's needs, create a calm environment, seek professional help if necessary, and employ reassurance and redirection techniques. Triggers such as environmental stressors or unmet needs can exacerbate agitation, making it crucial to address these factors for successful management. Caregivers play an important role in establishing a safe and supportive environment while implementing strategies to reduce agitation and enhance the well-being of individuals with dementia.
- Understand the patient's needs
- Create a calm environment
- Seek professional help if necessary
- Use reassurance and redirection techniques
- Address triggers for effective management
Dealing With Paranoia Symptoms

When dealing with paranoia symptoms in dementia, it's important to approach the individual with patience and understanding, as this common symptom can greatly impact daily interactions and relationships.
Persons with dementia may express unfounded suspicions or beliefs about others, leading to challenges in their daily interactions and relationships with caregivers. Responding calmly and reassuring those experiencing paranoia symptoms is vital to reduce anxiety and distress.
Understanding the underlying causes of paranoia in dementia is essential in tailoring strategies to address and manage this behavior effectively. By being attentive to the individual's concerns and providing a supportive environment, caregivers can help alleviate the distress caused by paranoia symptoms.
It's important to remember that individuals with dementia may perceive situations differently, and their paranoia should be handled with empathy and care. By approaching paranoia symptoms with compassion and a focus on reducing anxiety, caregivers can create a more supportive and understanding environment for individuals with dementia.
Strategies for Sleep Issues in Dementia

Establishing a consistent bedtime routine can greatly aid in regulating sleep patterns and reducing nighttime awakenings in individuals with dementia. When addressing sleep issues in dementia patients, it's important to take into account various factors that can impact their rest. Here are some strategies to improve sleep quality:
- Maintain a regular bedtime: Creating a predictable schedule can help regulate the circadian rhythm.
- Ensure exposure to daylight: Daytime light exposure is vital for maintaining the sleep-wake cycle.
- Address medical conditions: Treating underlying issues like sleep apnea or restless leg syndrome can alleviate sleep disturbances.
- Use non-pharmacological approaches: Creating a calming sleep environment and avoiding stimulants before bedtime can promote better rest.
- Monitor nighttime habits: Keeping track of sleep patterns and adjusting the routine accordingly can help improve overall sleep quality.
Frequently Asked Questions
How Long Do the 7 Stages of Dementia Last?
The 7 stages of dementia vary in duration, lasting from a few years to over a decade, with stages 6 and 7 typically being more extended and challenging. Each stage reflects a different level of cognitive decline and functional impairment.
What Are Three Tips for Helping People With Dementia?
We focus on simple communication, structured routines, and engaging activities to support individuals with dementia. These strategies provide comfort, reduce confusion, and enhance cognitive function. Our approach emphasizes understanding, security, and well-being.
How Do You Deal With Advanced Dementia Patients?
When dealing with advanced dementia patients, we focus on providing comfort, safety, and meeting physical needs. Prevent wandering, secure harmful substances, and guarantee a safe environment. Nurture connections and maintain familiarity. Tailor care strategies based on dementia stages.
What Is the Best Way to Manage Behaviors Associated With Dementia?
Addressing behaviors tied to dementia involves understanding triggers and offering person-centered care. Creating a calming environment, tailoring communication, and seeking professional support are essential. We focus on holistic approaches to enhance the quality of care.
Conclusion
In summary, understanding and addressing the top 7 dementia behaviors is vital for providing effective care for individuals with dementia.
By utilizing communication strategies, managing wandering, addressing incontinence challenges, coping with agitation, dealing with paranoia symptoms, and implementing strategies for sleep issues, caregivers can help improve the quality of life for those with dementia.
It's important to approach each behavior with patience, empathy, and a willingness to adapt to the individual's unique needs and preferences.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Caregiver Support
Symptoms Tests and Evaluations for Diagnosing Dementia
Hovering over dementia diagnosis? Learn about symptoms, tests, and evaluations to uncover the complexities of identifying this condition.
To diagnose dementia, recognize symptoms like memory loss, poor judgment, and confusion. Behavioral and memory assessments, including memory testing, reveal cognitive decline. Lab tests analyze tau and beta-amyloid levels. Brain imaging techniques like MRI provide detailed brain scans. EEGs and lumbar punctures aid diagnosis by detecting abnormal brain patterns. Thorough evaluation involves medical history review and neuro evaluations. Understanding these steps is important for addressing dementia effectively. Further exploration into these diagnostic processes uncovers significant insights for thorough dementia management.
Key Takeaways
- Memory loss, poor judgment, confusion, and disorientation are common symptoms.
- Memory testing, behavior pattern observation, and cognitive decline indication aid diagnosis.
- Laboratory tests analyze tau and beta-amyloid levels, ruling out conditions and tracking progression.
- Brain imaging techniques like MRI and CT scans provide valuable insights for specific diagnoses.
- EEGs and lumbar punctures serve as supplementary tools for comprehensive dementia evaluation.
Common Symptoms of Dementia
We commonly observe memory loss as a key symptom of dementia, particularly in individuals who struggle to recall recent events or important information. Alongside memory issues, poor judgment often manifests in those with dementia, impacting their decision-making abilities.
Confusion and disorientation in familiar surroundings can also signal the presence of dementia, causing distress and uncertainty for the individual. Difficulty speaking, understanding, or expressing thoughts may indicate early cognitive decline, highlighting the progressive nature of this condition.
Additionally, symptoms like wandering, getting lost, trouble handling money, and repeating questions are typical in dementia cases, emphasizing the multifaceted challenges individuals face. Recognizing these signs early can aid in timely intervention and support for those affected by dementia, paving the way for better management and quality of life.
Behavioral and Memory Assessments

When evaluating for dementia, it's essential to concentrate on memory testing to assess cognitive function and recall abilities.
Additionally, observing behavior patterns can provide valuable insights into changes in mood, personality, and social interactions that may indicate cognitive decline.
These evaluations play a key role in diagnosing dementia and understanding the progression of the condition.
Memory Testing Importance
Memory testing plays an essential role in diagnosing dementia by evaluating cognitive decline and memory loss. Conducting memory tests, such as the Mini-Mental State Examination (MMSE), is vital for early detection and accurate diagnosis of different types of dementia. These assessments help in identifying early signs of dementia and monitoring progression over time. Behavioral assessments complement memory testing by evaluating changes in behavior, mood swings, and personality shifts that can indicate dementia. By combining memory and behavioral assessments, healthcare professionals can gain a thorough understanding of an individual's cognitive function and provide appropriate interventions. The table below highlights the importance of memory testing in diagnosing dementia:
| Memory Testing Benefits | Description |
|---|---|
| Early Detection | Identifying cognitive decline and memory loss early on |
| Progression Monitoring | Tracking changes over time to assess disease progression |
| Accurate Diagnosis | Differentiating between various types of dementia for targeted treatment |
| Cognitive Impairment Assessment | Measuring cognitive function and memory deficits |
| Comprehensive Evaluation | Combining memory and behavioral assessments for a holistic understanding of the individual's condition |
Behavior Patterns Evaluation
Evaluation of behavior patterns and memory in dementia diagnosis provides essential insights into the individual's cognitive and emotional functioning. Behavioral assessments focus on changes in behavior patterns, social interactions, and emotional responses, aiding in understanding the impact on daily living activities and decision-making capabilities.
Memory assessments explore memory loss, including short-term memory difficulties, long-term memory recall, and recent event forgetfulness. These assessments may involve standardized tests like the Mini-Mental State Examination (MMSE) to evaluate cognitive functions such as memory, attention, and language skills.
Laboratory Tests for Dementia
When considering laboratory tests for dementia, it's essential to prioritize blood tests and brain imaging. These assessments play a pivotal role in ruling out underlying conditions that could be contributing to cognitive decline.
Blood Tests
Blood tests are essential for diagnosing dementia due to their ability to analyze markers like tau and beta-amyloid levels. They aid in ruling out conditions that mimic dementia symptoms, monitoring treatment efficacy, and tracking disease progression. Moreover, investigating blood markers supports drug development and improves the design of clinical trials. Although not standard practice in clinical settings, blood tests hold great potential for transforming dementia diagnosis.
Blood tests play a crucial role in diagnosing dementia by analyzing markers such as tau and beta-amyloid levels. These tests help in ruling out conditions mimicking dementia symptoms, track treatment effectiveness, and disease progression. Investigating blood markers supports drug development and enhances clinical trial design. While not yet routine in clinical settings, blood tests show promise for revolutionizing dementia diagnosis.
Brain Imaging
Brain imaging tests, such as MRI and CT scans, are pivotal in diagnosing dementia as they can help rule out other conditions and confirm the specific type of dementia by revealing brain abnormalities like shrinkage. MRI scans offer detailed brain images, while CT scans detect strokes or tumors mimicking dementia symptoms. SPECT and PET scans assess brain function and blood flow, aiding in specific dementia diagnoses. EEG tests, though uncommon, detect unusual brain activity linked to conditions like epilepsy. In in some cases, a lumbar puncture analyzes cerebrospinal fluid for dementia markers. These imaging techniques play an important role in accurately diagnosing dementia by providing valuable insights into brain structure and function.
| Imaging Test | Purpose | Use in Dementia Diagnosis |
|---|---|---|
| MRI | Detailed brain images | Confirms brain abnormalities |
| CT scan | Detects strokes and tumors | Rules out conditions resembling dementia |
| SPECT scan | Evaluates brain function | Helps in specific dementia diagnoses |
| PET scan | Assesses blood flow | Provides additional insights for diagnosis |
Imaging Techniques in Diagnosis
Utilizing advanced imaging techniques is essential in diagnosing dementia as they provide detailed insights into brain structure and function. When it comes to brain imaging for dementia diagnosis, CT scans and MRI scans play an important role in identifying structural changes that may indicate the presence of the condition. Additionally, SPECT and PET scans are valuable tools for evaluating brain function and detecting any abnormalities in blood flow, aiding in the accurate diagnosis of specific types of dementia.
MRI scans are particularly effective in confirming the type of dementia and revealing patterns of brain shrinkage associated with conditions like Alzheimer's disease. By using these imaging techniques, healthcare professionals can improve the accuracy of dementia diagnoses, ruling out other conditions such as brain tumors or strokes that may present similar symptoms. This ensures that individuals receive appropriate treatment tailored to their specific condition.
Additional Diagnostic Procedures

When exploring further diagnostic procedures for dementia, additional scans beyond MRI and CT scans can provide more detailed information about brain function. Tests like SPECT and PET scans are recommended when initial imaging results are inconclusive, offering insights into brain blood flow abnormalities. These scans play an important role in evaluating brain function, aiding in the early diagnosis of diseases like Alzheimer's. While EEG tests are rare, they can detect unusual brain activity in specific cases, especially when epilepsy is suspected. Additionally, lumbar punctures, also known as spinal taps, involve analyzing spinal fluid to diagnose certain types of dementia. These procedures are essential in understanding the mental processes and memory functions affected by various brain conditions. Autopsy post-death is sometimes necessary for definitive identification of the underlying causes of dementia. Below is a table summarizing the key additional diagnostic procedures for evaluating dementia:
| Diagnostic Procedure | Purpose |
|---|---|
| SPECT and PET Scans | Evaluate brain function and blood flow |
| EEG | Detect unusual brain activity |
| Lumbar Puncture | Analyze spinal fluid for diagnosis |
| Autopsy | Definitive identification post-death |
Role of EEGs and Lumbar Punctures
Exploring further diagnostic tools beyond standard imaging scans, EEGs and lumbar punctures play a pivotal role in evaluating brain function and detecting specific abnormalities related to dementia.
EEGs, or electroencephalograms, measure brain activity, aiding in distinguishing dementia from delirium and identifying abnormal brain patterns. This tool provides valuable insights into brain function and can pinpoint specific abnormalities associated with various forms of dementia.
Additionally, lumbar punctures, also known as spinal taps, involve collecting cerebrospinal fluid to analyze protein levels and biomarkers linked to dementia. By evaluating biomarkers like tau and beta-amyloid, lumbar punctures can indicate the presence of Alzheimer's disease or other types of dementia.
Both EEGs and lumbar punctures serve as essential supplementary diagnostic tools that, when combined with imaging tests and cognitive assessments, contribute significantly to the thorough evaluation of dementia.
Comprehensive Dementia Evaluation

In a thorough dementia evaluation, detailed medical history review plays a significant role in identifying symptoms and potential causes. Neuropsychological tests are conducted to evaluate cognitive function, memory, language skills, and orientation levels. These tests provide valuable insights into the individual's cognitive abilities and help in determining the presence and severity of dementia.
Additionally, neurological evaluations aid in identifying abnormalities in reflexes, coordination, muscle strength, and eye movements, which can further contribute to the diagnostic process. Brain imaging scans, such as MRI and CT scans, are essential for visualizing brain structure and ruling out other potential conditions that may mimic dementia symptoms.
Laboratory tests, including blood tests, CSF analysis, and genetic testing, may also be included to provide additional information for diagnosing and evaluating dementia. A thorough evaluation that incorporates these various tests is essential in accurately understanding and grasping the complexities of dementia, guiding healthcare professionals towards appropriate management and care strategies.
Frequently Asked Questions
What Tests Are Done to Confirm Dementia?
When confirming dementia, various tests are typically conducted. These include cognitive assessments and brain imaging scans like MRI or CT, which help identify memory issues and brain abnormalities, while also ruling out other potential causes. Laboratory tests may also be performed to check for underlying medical conditions. Additional tests like PET scans or EEGs can offer more detailed information. In some rare cases, autopsy post-mortem may be necessary for a definitive diagnosis.
What Assessment Is Used to Diagnose Dementia?
When diagnosing dementia, a variety of assessments is employed to evaluate cognitive functions, memory, language skills, and orientation. Neurological examinations help pinpoint physical abnormalities that may indicate dementia.
Brain imaging techniques like MRI and CT scans are essential for confirming dementia type and ruling out other conditions. EEG tests measure brain activity, aiding in distinguishing dementia from delirium.
These evaluations, along with spinal fluid analysis and post-mortem examinations, provide a thorough diagnostic picture.
What Is the 12 Question Test for Dementia?
The 12 Question Test for Dementia, also known as the General Practitioner Assessment of Cognition (GPCOG), is a brief screening tool that evaluates cognitive function and memory.
It includes questions on memory, orientation, and language skills. GPCOG scores can be influenced by factors like education level.
While this test can't diagnose dementia directly, it can signal potential memory issues.
It's an essential tool in the initial assessment of cognitive function.
What Is the Diagnostic Exam for Dementia?
When diagnosing dementia, a thorough medical history review and mental status exam are essential.
Lab tests like thyroid hormone and Vitamin B12 levels help rule out other conditions.
Imaging tests like CT scans identify brain abnormalities.
Additional tests like EEG measure brain activity.
Combining these evaluations gives a detailed view for an accurate diagnosis.
Proper assessment is key for early intervention and management of dementia.
Conclusion
In diagnosing dementia, it's essential to recognize the common symptoms. This includes conducting behavioral and memory assessments and utilizing laboratory tests and imaging techniques. Additional diagnostic procedures such as EEGs and lumbar punctures may also be necessary for a thorough evaluation.
By addressing these steps systematically, healthcare professionals can provide a clearer picture of the condition and guide appropriate treatment plans. Remember, early detection and intervention are key in managing dementia effectively.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Caregiver Support
Key Signs of End-Stage Lewy Body Dementia
Discover the critical signs of end-stage Lewy body dementia, including memory loss and hallucinations, essential for understanding advanced care needs.
In the final stages of Lewy body dementia, key signs such as memory loss, confusion, and difficulty with decision-making emerge. Hallucinations, paranoia, and motor symptoms like tremors become more pronounced. Behavioral changes, including aggression and agitation, can occur alongside swallowing difficulties and infection risk. Caregivers must focus on comfort and safety, managing symptoms through hospice care and emotional support. Specialized equipment and adjusted medication plans are vital. These indicators signal the need for specialized care and attention. As you learn more about these signs, you'll gain a better understanding of how to support individuals with end-stage Lewy body dementia.
Key Takeaways
- Increased cognitive decline leading to severe memory loss and confusion.
- Persistent and distressing hallucinations and delusions.
- Severe motor symptoms like tremors and rigidity affecting mobility.
- Aggressive behavior, agitation, and verbal outbursts escalate.
- Swallowing difficulties with a high risk of aspiration and infections.
Cognitive Decline and Memory Loss
As cognitive decline progresses in end-stage Lewy Body Dementia, individuals experience profound memory loss and confusion. In this advanced stage of dementia, the ability to remember recent events, familiar faces, or even essential personal details becomes severely compromised. Tasks that once seemed simple, like recalling names or following familiar routines, may now present significant challenges. The impact of severe memory loss in end-stage Lewy Body Dementia extends beyond forgetfulness; it can lead to disorientation, difficulty in communicating effectively, and an increased reliance on caregivers for daily activities.
The progression of cognitive decline in advanced dementia stages such as end-stage Lewy Body Dementia can result in a noticeable deterioration in decision-making abilities and problem-solving skills. As memory loss becomes more pronounced, individuals may struggle to make sense of their surroundings or engage in coherent conversations. This decline in cognitive function underscores the importance of providing compassionate support and understanding to those affected by this challenging condition.
Hallucinations and Delusions

Hallucinations and delusions, prevalent symptoms in end-stage Lewy body dementia, greatly impact individuals' perception of reality and behavior. Visual hallucinations, such as seeing people or objects that aren't there, are common and can be distressing. Similarly, delusions involving false beliefs like paranoia can lead to fear and suspicion. As Lewy body dementia progresses, these symptoms often worsen, affecting how individuals understand the world around them and leading to changes in their actions.
Managing hallucinations and delusions in end-stage Lewy body dementia requires a thorough approach. Healthcare professionals, caregivers, and supportive interventions play vital roles in helping individuals cope with these challenging symptoms. It's crucial to create a safe and calming environment, provide reassurance and validation, and guarantee proper medication management under the guidance of healthcare providers. By working together and tailoring strategies to the individual's needs, we can offer essential support and improve their quality of life during this difficult time.
Motor Symptoms: Tremors and Rigidity
Progressing through the advanced stages of Lewy body dementia, individuals may experience pronounced and persistent tremors, affecting their daily activities and mobility. These tremors can make simple tasks like eating, drinking, or writing challenging. Additionally, rigidity in muscles can cause stiffness, making movement uncomfortable and restricted. Both tremors and rigidity are common motor symptoms in advanced Lewy body dementia and can have a major impact on the quality of life of those affected.
In the end stages of the disease, managing these motor symptoms becomes essential. Specialized care that focuses on addressing tremors and rigidity is crucial for providing comfort and maintaining the individual's well-being. This specialized care may involve adjustments in medications, physical therapy to improve mobility, and assistive devices to support daily activities.
Caregivers and healthcare providers play a critical role in monitoring changes in tremors and rigidity to tailor care plans accordingly. By staying attentive to these motor symptoms, they can make sure that individuals with advanced Lewy body dementia receive the necessary support and interventions to enhance their quality of life.
Behavioral Changes: Aggression and Agitation

Managing aggression and agitation becomes essential in providing effective care for individuals in the end stages of Lewy Body Dementia. Aggression and agitation are common behavioral changes in this stage, causing distress for both the person with LBD and their caregivers. Agitation may show through restlessness, pacing, or verbal outbursts, while aggression can include physical violence, yelling, or threats.
Caregivers play an important role in understanding and managing these behaviors. It's essential to approach the individual with empathy and patience, acknowledging their frustrations and validating their feelings. Creating a calm and safe environment can help reduce triggers for aggression and agitation. Techniques such as distraction, redirection, and maintaining a consistent routine can be beneficial. Seeking support from healthcare professionals or joining caregiver support groups can also provide valuable guidance and assistance.
Swallowing Difficulties and Aspiration Risk
Given the challenges of aggression and agitation in end-stage Lewy Body Dementia, it's important to address the significant issue of swallowing difficulties and aspiration risk that can arise in this advanced stage of the disease.
Swallowing difficulties in late-stage Lewy body dementia can lead to aspiration, where food or liquid enters the airway instead of the esophagus. Aspiration risk increases due to weakened swallowing muscles and impaired coordination, making individuals more susceptible to complications. Swallowing problems can result in coughing, choking, chest infections, and pneumonia, particularly aspiration pneumonia, which is a common concern in end-stage Lewy body dementia.
It's essential to monitor and manage swallowing difficulties in late-stage Lewy body dementia to prevent aspiration-related complications, ensuring comfort and quality of life for individuals. Caregivers and healthcare providers play a crucial role in supporting individuals with Lewy body dementia through this challenging aspect of the disease, promoting safety and well-being.
Sleep Disturbances and Urinary Incontinence
Sleep problems, like increased daytime napping and nighttime confusion, are common in those with end-stage Lewy Body Dementia.
Urinary issues, such as incontinence, can also arise due to cognitive decline affecting bladder control.
Managing these symptoms is essential for enhancing comfort and quality of life in individuals facing advanced stages of Lewy Body Dementia.
Sleep Problems in LBD
Experiencing disruptions in sleep patterns and struggles with urinary incontinence are prevalent challenges faced by individuals with Lewy body dementia (LBD). These issues can have a substantial impact on the quality of life of both the affected individual and their caregivers. Here are some key points to keep in mind:
- Sleep disturbances: Insomnia, excessive daytime sleepiness, and disrupted sleep patterns are common in LBD.
- REM sleep behavior disorder: Acting out dreams, talking, or moving during sleep can occur, posing safety risks.
- Urinary incontinence: Affects over 50% of individuals with advanced LBD, leading to challenges in managing bladder control.
Addressing these challenges through appropriate management strategies is essential for enhancing overall well-being and quality of life.
Urinary Issues in LBD
Frequently observed in individuals with Lewy body dementia (LBD) are urinary issues, especially urinary incontinence, which arises from disruptions in the brain's bladder control functions. LBD patients may also experience REM sleep behavior disorder, contributing to sleep disturbances. Nocturia, the frequent need to urinate at night, can further impact the quality of sleep for individuals with LBD.
Managing urinary issues in LBD involves strategies like scheduled toileting, fluid management, and adjusting medications. These approaches aim to improve bladder activity and enhance the overall well-being of those affected by LBD. Understanding and addressing urinary incontinence in LBD is essential for maintaining comfort and dignity, emphasizing the importance of holistic LBD management that considers all aspects of the disease.
Increased Susceptibility to Infections

Individuals with end-stage Lewy Body Dementia exhibit a heightened vulnerability to infections due to their compromised immune systems. In this advanced stage of the disease, the body's ability to fight off harmful pathogens is greatly weakened, making individuals more prone to infections. Common infections that affect those with end-stage Lewy Body Dementia include pneumonia and urinary tract infections. These infections can worsen the symptoms of Lewy Body Dementia and contribute to a rapid decline in health. It's essential to monitor for signs of infections and seek prompt medical attention if any are suspected.
Weakened immune systems increase susceptibility to infections.
Pneumonia and urinary tract infections are common in end-stage Lewy Body Dementia.
Infections can accelerate the progression of the disease and require immediate medical treatment.
Caregiver Focus: Comfort and Safety

To enhance the well-being of individuals with end-stage Lewy body dementia, caregivers should prioritize creating a safe and comforting environment. It's vital to make sure the surroundings are free from hazards that could lead to falls or accidents. Implement measures such as removing clutter, securing rugs, and providing support with mobility to enhance safety.
Additionally, focus on maintaining a calm and soothing atmosphere to reduce agitation and distress in individuals with Lewy body dementia. Consider using specialized equipment like cushions or chairs to optimize comfort and positioning, which can make a substantial difference in their daily comfort levels. Regularly assess and address any pain or discomfort the individual may be experiencing to improve their overall quality of life.
Symptom Management in End-Stage

In the care of individuals with end-stage Lewy body dementia, the focus shifts towards effective symptom management to provide comfort and alleviate pain and distress. When managing symptoms in this stage, it's important to prioritize palliative care and pain management to enhance the individual's quality of life.
Here are key strategies for symptom management in end-stage Lewy body dementia:
- Observing Signs of Pain: Caregivers should carefully observe for any signs of pain or distress in individuals with end-stage Lewy body dementia to address their needs promptly.
- Calling Hospice for Support: Hospice care can provide specialized assistance in pain management, adjust medication plans, and offer emotional and spiritual support tailored to the individual's requirements.
- Providing Comfort Equipment: Ensuring the individual has necessary equipment for comfort, such as specialized beds or cushions, can improve their well-being during end-stage care.
Frequently Asked Questions
What Happens in the Final Stages of Lewy Body Dementia?
In the final stages of Lewy Body Dementia, individuals may experience severe cognitive decline, limited mobility, and increased dependency on caregivers. Hallucinations, delusions, and motor symptoms worsen considerably. Swallowing difficulties, behavioral changes, and communication decline are common.
What Are the Signs That Lewy Body Dementia Is Getting Worse?
As we observe the progression of Lewy body dementia, we notice heightened frequency and severity of hallucinations, cognitive decline with significant memory loss, movement difficulties, intensified sleep disturbances, and aggravated mood swings, anxiety, and depression.
What Is the Timeline of the Stages of Lewy Body Dementia?
In Lewy body dementia, the stages vary in duration and progression. Symptoms like cognitive decline, hallucinations, and movement issues manifest differently. Understanding each stage aids in treatment decisions and care planning, allowing for tailored support.
What Is Palliative Care for Lewy Body Dementia?
Palliative care for Lewy Body Dementia focuses on improving quality of life, managing symptoms, and providing emotional support. It aims to enhance comfort, reduce suffering, and maintain dignity in end-stage LBD, involving a team of healthcare professionals to address holistic needs.
Conclusion
In summary, when caring for someone with end-stage Lewy body dementia, it's important to be aware of the key indicators of the disease.
Remember, like a puzzle with missing pieces, each symptom plays a vital role in understanding the progression of the illness.
By recognizing these signs and addressing them promptly, caregivers can provide the necessary support and comfort to their loved ones during this challenging time.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
-

 Dementia Care2 weeks ago
Dementia Care2 weeks agoHow Gabapentin Affects Dementia: A Comprehensive Guide
-

 Dementia Care2 months ago
Dementia Care2 months agoUnderstanding the Stages of Vascular Dementia: A Visual Chart Guide
-

 Dementia Care2 weeks ago
Dementia Care2 weeks ago5 Things You Need to Know About Jack Nicholson’s Dementia
-

 Medication Management1 month ago
Medication Management1 month agoGabapentin Side Effects: Memory Loss Concerns?
-

 Dementia Care2 months ago
Dementia Care2 months agoUnderstanding Narcissism and Dementia: A How-To Guide
-

 Palliative Care for Parkinson's2 weeks ago
Palliative Care for Parkinson's2 weeks agoPalliative Care for Parkinson’s: A New Hope for Patients”
-

 Dementia Care2 weeks ago
Dementia Care2 weeks ago10 Engaging Dementia Games for Cognitive Stimulation
-

 Dementia Care2 months ago
Dementia Care2 months agoHow to Deal with a Parent’s Dementia: A Practical Guide

















