Dementia Care
What Does the Fast Score Measure in Dementia?
Leverage the intricate layers of Fast Score Dementia to unravel the complexities of dementia progression – discover how this tool transforms patient care.

When evaluating tools to monitor the advancement of dementia, it is important to analyze how effectively the Fast Score Dementia tool reflects the intricate facets of cognitive deterioration.
However, delving into the nuances of this scale unveils a comprehensive framework that aids in understanding the multifaceted nature of dementia stages.
From subtle cognitive impairments to profound functional limitations, the Fast Score Dementia offers a detailed roadmap for caregivers and healthcare professionals.
Join us in exploring how this tool can revolutionize dementia care and enhance patient outcomes.
Key Takeaways
- Tailor care plans to individual needs for better outcomes
- Identify risk factors to enhance successful interventions
- Monitor progression using FAST score for personalized care
- Utilize lifestyle modifications to improve patient well-being
Understanding Fast Score Dementia
In understanding Fast Score Dementia, we analyze the progressive stages of functional decline and cognitive impairment assessed by the FAST scale. This scale plays a crucial role in guiding caregivers to comprehend the evolving needs of individuals with dementia as they face challenges in performing daily tasks. By utilizing the FAST scale, caregivers can tailor care plans specifically suited to the unique requirements of dementia patients at each stage of the disease. Understanding the nuances of functional decline and cognitive abilities enables caregivers to provide customized care that enhances patient outcomes and quality of life.
Caregivers rely on the FAST scale to gauge the level of support necessary for dementia patients, which aids in establishing achievable goals and ensuring that interventions are timely and appropriate. This systematic approach also proves beneficial for hospice care providers as they design personalized care plans that adapt to the changing needs of individuals with dementia, ultimately enhancing the quality of care provided.
Causes and Risk Factors
Understanding the various causes and risk factors associated with dementia is crucial for early detection and effective management of the condition. Dementia can stem from various sources, including Alzheimer's disease, vascular dementia, Lewy body dementia, and frontotemporal dementia. Risk factors for developing dementia encompass aging, family history of dementia, cardiovascular disease, genetic predispositions, brain injuries, and lifestyle factors such as lack of physical activity and poor dietary habits. Recognizing specific causes and risk factors enables healthcare professionals to tailor interventions for each individual, enhancing the likelihood of successful outcomes. Early identification of these factors can lead to timely interventions that may help slow down the progression of the disease. Below is a table summarizing some of the key causes and risk factors associated with dementia:
| Causes | Risk Factors |
|---|---|
| Alzheimer's | Aging |
| Vascular dementia | Family history of dementia |
| Lewy body dementia | Cardiovascular disease |
| Frontotemporal dementia | Genetic factors |
| Brain injuries |
Symptoms and Progression
Tracking the progression of dementia symptoms is essential for caregivers to provide appropriate support and interventions for patients. Symptoms of dementia can range from mild forgetfulness to severe cognitive impairment.
The FAST score is a valuable tool in monitoring functional decline, with Stage 7 indicating total dependence and severe cognitive decline. Caregivers rely on the FAST score to understand the evolving needs of individuals with dementia accurately.
Regular monitoring using the FAST score is crucial for tracking disease progression effectively. By observing changes in symptoms and progression through the FAST score, caregivers can tailor care plans to meet the specific requirements of patients at different stages of dementia.
Understanding the trajectory of cognitive decline allows caregivers to anticipate and address challenges proactively, ensuring that individuals with dementia receive the best possible care and support throughout the course of their illness.
Diagnosis and Evaluation

Utilizing the FAST Scale is essential in assessing functional decline and planning care for individuals with dementia. This tool allows caregivers to track the progression of the disease and tailor personalized care plans to meet the specific needs of dementia patients. Here are three key points to consider when utilizing the FAST Scale:
- Stages of Decline: The FAST Scale consists of 7 stages, each representing a different level of functional decline, from no difficulty to total dependence in daily tasks. Caregivers can use these stages to evaluate cognitive and physical abilities over time accurately.
- Identification of Progression: By regularly assessing dementia patients using the FAST Scale, caregivers can identify the progression of the disease. This information is crucial in determining the appropriate level of care and support needed for each individual.
- Planning Care: Understanding the FAST Scale enables caregivers to develop personalized care plans that address the specific challenges faced by dementia patients at different stages of the disease. This tailored approach ensures that individuals receive the support they need to maintain their quality of life.
Treatment and Management
Treatment and management of dementia aim to enhance symptom control and improve the overall quality of life for individuals affected by the condition. Utilizing tools like the FAST scale and other functional assessment tools can aid in tracking cognitive decline and developing effective care plans.
Dementia management often involves a combination of treatment strategies, including medication, therapy, and lifestyle modifications such as cognitive stimulation, physical activity, and social engagement. Caregiver education and support groups are crucial components in providing comprehensive care.
Regular monitoring of symptoms allows for timely adjustments in treatment plans to optimize outcomes. By focusing on enhancing quality of life through personalized care plans and involving caregivers in the process, individuals with dementia can experience improved well-being and functional abilities.
Emphasizing lifestyle modifications and ensuring a supportive environment are essential aspects of dementia management that contribute to overall patient satisfaction and well-being.
Frequently Asked Questions
What Is Fast Score for Dementia?
We assess functional decline in all forms of dementia using the FAST score, a tool with 7 stages from no impairment to total dependence. It helps us plan and understand care needs.
The score tracks cognitive and physical abilities, aiding in monitoring decline. We, as caregivers, rely on the FAST score to tailor care plans for dementia patients.
It's essential for us to comprehend the FAST score to assess patients' functional status accurately and provide suitable care.
What Is Fast 7 Criteria for Hospice?
When considering hospice eligibility, Fast 7 criteria indicate the most severe stage of dementia, requiring extensive assistance for basic functions. This stage often involves loss of ambulatory ability and communication limitations.
Fast 7 criteria typically prompt consideration for hospice care, focusing on end-of-life comfort and support. Meeting these criteria signifies a significant decline in the patient's condition, necessitating specialized care to ensure their quality of life in this critical phase.
What Is the Life Expectancy of Someone With Rapid Onset Dementia?
We must understand that life expectancy in rapid onset dementia cases can vary significantly due to various factors.
It's crucial to consider the underlying cause and individual health conditions when predicting survival time.
Individuals with rapid onset dementia may experience a more aggressive decline in cognitive and physical functions, potentially leading to a shorter lifespan.
Tailored care and support from caregivers and healthcare providers are essential to enhance the well-being of those with this condition.
How Do You Score a Fast Assessment?
We score a FAST assessment by observing and evaluating a patient's daily activities to assess their level of independence. This involves looking at specific criteria for each stage of the scale, focusing on tasks like dressing, eating, and communication.
A higher score indicates greater functional impairment and the need for more assistance. Caregivers use the FAST score to monitor changes in a patient's abilities over time and adjust care plans accordingly.
Conclusion
In conclusion, the Fast Score Dementia tool provides a structured way to track the progression of dementia, allowing for better care and management of patients.
It's ironic how a simple numerical scale can encapsulate the complex journey of cognitive decline, serving as a stark reminder of the devastating impact of this disease.
The numbers may seem clinical, but they represent the gradual loss of a person's identity and independence.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Dementia Care
Managing Dementia Symptoms: Trazodone Guide
Curious about the mysterious connection between trazodone and dementia?

When delving into the world of trazodone and its possible effects on dementia, we are met with a wealth of studies uncovering a intricate link between this antidepressant and cognitive health. While some results suggest favorable results, a cloud of doubt remains, underscoring the importance of further in-depth research.
The connection between trazodone and dementia opens a door to a realm of possibilities, urging us to uncover the full extent of its effects and implications for those navigating cognitive challenges.
Key Takeaways
- Trazodone effectively manages behavioral symptoms in elderly dementia patients.
- Long-term trazodone use may lead to cognitive decline in elderly individuals.
- Trazodone influences neurotransmitters and cognitive aspects in dementia management.
- Research is ongoing to explore trazodone's impact on cognitive function in dementia.
Potential Link Between Trazodone and Dementia
In exploring the potential link between Trazodone and dementia, it becomes evident that its role in managing behavioral symptoms offers promising cognitive benefits for individuals with this condition.
Trazodone, an antidepressant, has shown potential in improving cognitive function by effectively addressing behavioral symptoms commonly seen in dementia patients. Studies indicate that Trazodone may also enhance sleep quality in these individuals, indirectly contributing to better cognitive outcomes.
Moreover, research suggests that Trazodone can reduce caregiver burden in elderly dementia patients without compromising their cognitive abilities, thereby improving the overall quality of life for both patients and caregivers.
When used in conjunction with standard treatments, Trazodone has been associated with a significant reduction in neuropsychiatric disorder symptoms in dementia patients. These findings underscore the importance of considering Trazodone as a potential therapeutic option for managing behavioral symptoms and enhancing cognitive function in elderly patients with dementia.
Risks of Long-Term Trazodone Use

Long-term use of trazodone in elderly patients has been linked to potential risks of cognitive impairment, particularly concerning memory and cognitive function deterioration over time. Chronic trazodone use may have adverse effects on cognitive abilities, raising concerns about cognitive decline in patients, especially those with dementia. It is essential to carefully monitor individuals on prolonged trazodone treatment to assess any cognitive changes and address them promptly.
To better understand the risks associated with long-term trazodone use, the table below summarizes key points regarding cognitive impairment and dementia risk in elderly patients:
| Aspect | Impact | Importance |
|---|---|---|
| Memory Function | Affected by prolonged trazodone use | Regular monitoring crucial |
| Cognitive Decline | Potential risk for deterioration over time | Early intervention necessary |
| Adverse Effects | May lead to cognitive impairment in elderly patients | Close observation required |
These factors emphasize the critical need for proactive monitoring of elderly patients on long-term trazodone therapy to mitigate cognitive risks effectively.
Mechanisms of Trazodone-Related Dementia
Prolonged use of trazodone in elderly patients has been associated with potential mechanisms that could contribute to dementia development. Trazodone's mechanism of action involves the modulation of neurotransmitters such as serotonin and norepinephrine, which play crucial roles in cognitive function.
Additionally, trazodone's impact on energy management systems and sleep patterns is thought to influence the progression of dementia. The drug's interaction with neuroplasticity, specifically in regulating amyloid-β protein precursor metabolism, may hold significance for dementia treatment.
Studies also highlight trazodone's effects on cognitive fatigue, synaptic plasticity, and learning mechanisms, suggesting a complex interplay in dementia pathology. Understanding trazodone's role in balancing synaptic plasticity and its potential disease-modifying effects in conditions like Alzheimer's disease is essential for elucidating its impact on dementia progression.
Further research into trazodone's influence on brainstem pathways is warranted to comprehensively assess its implications for cognitive health in the aging population.
Implications for Patients and Healthcare Providers

Considering the promising outcomes observed in behavioral symptom management and caregiver burden reduction in elderly dementia patients, trazodone emerges as a valuable therapeutic option with potential benefits for both patients and healthcare providers. Trazodone's efficacy in improving sleep quality contributes significantly to the overall well-being of dementia patients. Additionally, its ability to reduce neuropsychiatric symptoms highlights its potential as a comprehensive treatment option. The statistical analysis revealing a significant decrease in NPI-NH scores underscores the positive impact of trazodone on behavioral symptoms in dementia. This evidence suggests that trazodone not only aids in managing cognitive decline but also addresses the challenging behavioral aspects of dementia, providing relief to both patients and caregivers.
- Trazodone shows promise in managing behavioral symptoms in elderly dementia patients
- Studies indicate a significant reduction in caregiver burden with trazodone treatment
- Improvement in sleep quality was noted with trazodone therapy
- Trazodone's effectiveness in reducing neuropsychiatric symptoms highlights its potential as a valuable treatment option
- Statistical analysis revealed a significant decrease in NPI-NH scores
Current Research on Trazodone and Dementia
Current research on trazodone and dementia explores its effectiveness in managing behavioral symptoms and potential impact on cognitive function in elderly patients. Studies have shown mixed results regarding trazodone's influence on cognitive function in dementia patients. However, it has demonstrated potential in improving sleep quality and reducing behavioral symptoms in this population. Research suggests that trazodone may aid in managing neuropsychiatric disorders associated with dementia without exacerbating cognitive impairment. Moreover, the use of trazodone has been linked to a notable decrease in caregiver burden when employed for addressing behavioral symptoms in dementia.
| Aspect | Findings |
|---|---|
| Cognitive Function | Mixed results on trazodone's impact on cognitive function in dementia |
| Sleep Quality | Potential improvement in sleep quality and reduction in behavioral symptoms |
| Neuropsychiatric Care | Management of neuropsychiatric disorders without worsening cognitive function |
| Caregiver Burden | Significant reduction in caregiver burden when managing behavioral symptoms |
Ongoing research aims to further investigate trazodone's efficacy in managing dementia-related behavioral symptoms and its potential impact on cognitive function.
Frequently Asked Questions
What Are 3 Things to Never Do With Your Loved One With Dementia?
When caring for a loved one with dementia, it's important to remember a few key points:
- Never argue or correct them, as it can lead to frustration.
- Avoid leaving them unsupervised in dangerous situations due to memory loss.
- Don't overwhelm them with too many choices or tasks at once, as it can cause anxiety.
Prioritizing their safety, emotional well-being, and minimizing stress are essential in providing the best care for our loved ones with dementia.
What Is the Best Medication for Agitation in Dementia?
When addressing agitation in dementia, it's crucial to consider individual needs. Medications like antipsychotics can be effective but come with risks. Non-pharmacological approaches, such as environmental modifications and personalized care, are key.
One interesting statistic highlights that non-drug strategies can reduce agitation in up to 40% of cases. By focusing on tailored interventions, we prioritize the well-being of those with dementia while minimizing potential side effects associated with medications.
What Is the Best Anxiety Medication for Dementia Patients?
For anxiety in dementia patients, a variety of medications can be considered, including selective serotonin reuptake inhibitors (SSRIs) like sertraline or citalopram, or benzodiazepines such as lorazepam.
Each medication has its benefits and risks, and the choice should be individualized based on the patient's specific needs and medical history. Consulting with a healthcare provider is crucial to determine the best anxiety medication for dementia patients.
What Is the Number One Trigger for Dementia Behavior?
We find that environmental factors, such as changes in routine or surroundings, are often the primary triggers for dementia behavior. These factors, like loud noises or unfamiliar environments, can cause confusion and agitation in individuals with dementia.
Identifying and minimizing these triggers is crucial for managing challenging behaviors. By creating a calm and structured environment, caregivers can significantly improve the quality of life for both dementia patients and themselves.
Conclusion
In exploring the potential link between trazodone and dementia, the risks of long-term use must be carefully considered. Mechanisms of trazodone-related dementia remain unclear, highlighting the need for further research.
Implications for patients and healthcare providers are significant, given the mixed results of current studies. Continued investigation into the cognitive effects of trazodone is crucial for understanding its impact on dementia risk.
Dementia Care
7 Key Stages of Frontotemporal Dementia Explained
Keen to understand the intricate journey of Frontotemporal Dementia? Explore the seven stages and their impact on individuals and relationships.

Frontotemporal dementia (FTD) is typically acknowledged as being less prevalent than Alzheimer’s disease, representing approximately 10-15% of all dementia cases.
But did you know that FTD progresses through seven distinct stages, each with its own set of challenges and symptoms?
Understanding these stages can provide valuable insights into the progression of this complex disease and the care needed at each phase.
Let's explore how individuals with FTD navigate through these stages and the impact it has on their lives and relationships.
Key Takeaways
- Early signs include memory loss, behavioral changes, language difficulties, and movement problems.
- Social challenges may manifest as apathy, disinhibition, lack of empathy, and inappropriate behaviors.
- Communication breakdowns can arise from speech problems, word-finding challenges, and reduced fluency.
- Severe stages exhibit profound memory loss, impaired decision-making, communication difficulties, and behavioral changes.
Early Warning Signs
In the early stages of frontotemporal dementia, warning signs manifest through a range of behavioral, language, movement, and cognitive changes. Memory loss, particularly in short-term memory, is often one of the first noticeable symptoms. Individuals may struggle to retain recently acquired information or recall recent events. Behavioral changes such as apathy, disinhibition, and loss of empathy can also emerge early on. These alterations in behavior may be stark departures from the individual's previous demeanor.
Language difficulties present another common early warning sign. Speech problems, difficulty finding words, or reduced fluency in conversation can indicate the onset of frontotemporal dementia. Movement problems, including muscle weakness and coordination issues, may become apparent in the initial stages. Executive function decline, characterized by challenges in planning, organizing tasks, and decision-making, is also frequently observed early in the progression of the disease.
Recognizing these early warning signs is crucial for timely intervention and management of frontotemporal dementia.
Mild Cognitive Changes

Mild cognitive changes in frontotemporal dementia typically manifest as subtle alterations in memory, decision-making, language, and behavior. Forgetfulness becomes noticeable, with individuals experiencing difficulty in recalling recent events or information.
Tasks requiring planning may present challenges, leading to inefficiency in organizing daily activities. Memory problems start to affect routines and tasks, causing disruptions in usual functioning. Decision-making abilities may diminish, making it harder to weigh options and choose the best course of action.
Language difficulties may arise, with individuals struggling to find words or articulate thoughts clearly. Additionally, behavioral changes like decreased motivation and reduced interest in once enjoyable activities can be observed.
These early signs of mild cognitive changes in frontotemporal dementia highlight the importance of monitoring cognitive functions and seeking medical evaluation if such symptoms become apparent. Understanding these subtle alterations can aid in early detection and intervention to improve the quality of life for individuals affected by this condition.
Behavioral Shifts
Behavioral shifts in frontotemporal dementia encompass early changes like apathy and disinhibition, along with challenges in regulating emotions. These alterations can manifest as reduced empathy and inappropriate social conduct, often affecting relationships and social interactions significantly.
Individuals may also exhibit a lack of judgment and decreased inhibitions as part of these behavioral transformations.
Early Behavioral Changes
During the early stages of frontotemporal dementia, individuals often experience notable shifts in their behavior, including apathy, disinhibition, and a loss of empathy. These early behavioral changes may manifest as inappropriate social behaviors, reduced interest in activities, and a lack of judgment.
Apathy, characterized by a lack of motivation or interest, is a common early symptom. Disinhibition, where individuals may act impulsively without considering social norms, is also prevalent. Moreover, the loss of empathy towards others and challenges in understanding social cues contribute to the behavioral shifts seen in early frontotemporal dementia.
These changes can have significant consequences on relationships and daily interactions, underscoring the importance of early recognition and support for individuals affected by FTD.
Social Interaction Challenges
The manifestation of social interaction challenges in frontotemporal dementia presents as a complex interplay of apathy, disinhibition, and loss of empathy. Individuals with FTD may exhibit inappropriate social behaviors and show reduced interest in social activities, impacting their relationships and ability to engage in interpersonal interactions.
These behavioral shifts can lead to difficulties in socializing and maintaining connections, as the loss of empathy and judgment strains communication with others. Understanding and addressing these social interaction challenges are crucial for providing effective support and care to individuals with FTD.
Emotional Regulation Difficulties
Emotional regulation difficulties in frontotemporal dementia often manifest as a complex interplay of apathy, disinhibition, and loss of empathy, impacting social interactions and behavioral responses.
Individuals with FTD may display inappropriate social behaviors due to challenges in controlling emotions, leading to a lack of judgment and reduced interest in activities.
The loss of inhibitions in frontotemporal dementia can result in socially unacceptable actions and speech, necessitating a focused approach on managing emotional regulation.
Understanding these behavioral shifts is essential in providing appropriate care for individuals with frontotemporal dementia.
Language Difficulties
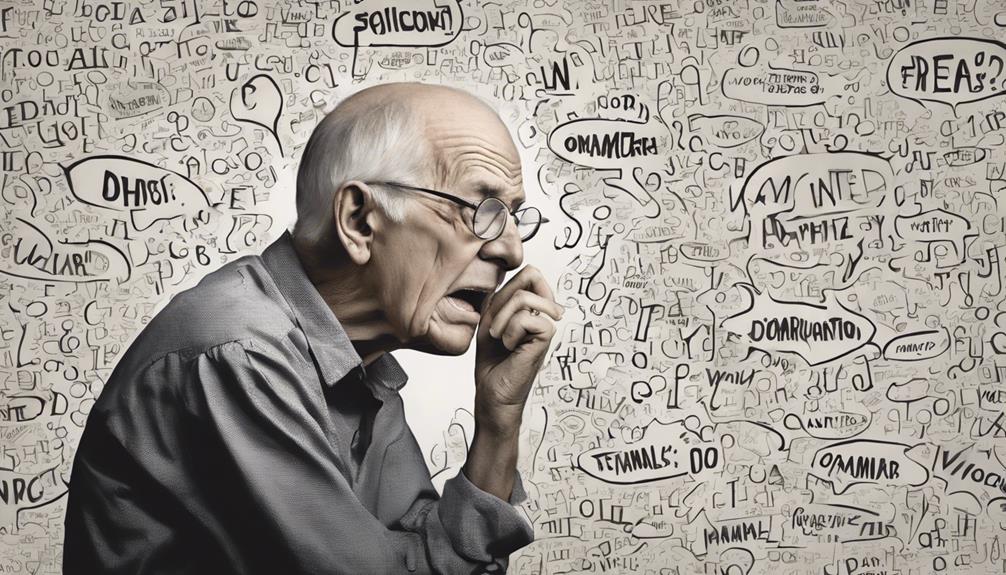
Amidst the progression of frontotemporal dementia, individuals often encounter a range of language difficulties, encompassing speech impediments, word retrieval challenges, and diminished verbal fluency. These challenges can significantly impact daily communication and social interactions. Individuals with frontotemporal dementia may experience difficulty in naming objects, understanding complex sentences, and following conversations, leading to frustration and isolation.
| Language Difficulties | Examples | Management |
|---|---|---|
| Speech problems | Difficulty articulating words | Speech and language therapy |
| Word-finding challenges | Struggling to recall words | Cognitive exercises |
| Reduced verbal fluency | Speaking in shorter sentences | Communication strategies |
It is crucial to address these language difficulties promptly through interventions like speech and language therapy. Such therapies can help individuals improve their communication skills, enhance their ability to express themselves, and maintain meaningful connections with others amidst the challenges presented by frontotemporal dementia.
Quality of Life Impact

As individuals progress through the stages of frontotemporal dementia, they may encounter challenges in daily living activities, such as self-care and household tasks.
Social interaction difficulties can arise due to behavioral changes and communication impairments, impacting relationships and connections with others.
Emotional well-being effects, including mood alterations and frustration, can further diminish the quality of life for both patients and their caregivers.
Daily Living Challenges
Daily living challenges in frontotemporal dementia significantly impact individuals' quality of life by diminishing their independence and functional abilities as the disease progresses.
Basic activities such as dressing, grooming, and meal preparation become challenging. Tasks requiring planning, organization, and decision-making skills become increasingly difficult, leading to a reliance on caregivers for daily needs.
Personal care, household chores, and managing finances can become overwhelming. The decline in cognitive function and behavioral changes pose safety concerns, further reducing the quality of life in daily living situations.
It's crucial for caregivers and healthcare professionals to provide support in managing these challenges to ensure the well-being and safety of individuals with frontotemporal dementia.
Social Interaction Difficulties
Navigating social interactions in frontotemporal dementia poses significant challenges that can lead to strained relationships and isolation, impacting the quality of life for individuals with this condition. Individuals with FTD may exhibit inappropriate social behaviors, lack of empathy, and reduced interest in engaging with others. Communication breakdowns due to language and speech issues can further hinder social interactions for FTD patients. Behavioral changes like disinhibition and apathy can impact the quality of life and social interactions of individuals with FTD. Caregivers and support networks play a vital role in helping FTD patients navigate social challenges and maintain connections with loved ones.
| Social Interaction Difficulties | Impact on Individuals with FTD |
|---|---|
| Inappropriate social behaviors | Strained relationships |
| Lack of empathy | Isolation |
| Reduced interest | Challenges in maintaining friendships |
| Communication breakdowns | Hindered social interactions |
Emotional Well-Being Effects
The impact of frontotemporal dementia on emotional well-being, particularly in relation to quality of life, is profound and multifaceted. Personality changes, emotional challenges, and disrupted social connections can significantly affect individuals with FTD and their caregivers.
Patients may struggle with managing frustration, confusion, and feelings of isolation, while caregivers often experience stress, grief, and emotional strain. Seeking support from healthcare professionals, engaging in support groups, and maintaining social connections are vital for improving emotional well-being.
Additionally, therapy, self-care practices, and relaxation techniques play a crucial role in enhancing the quality of life for both patients and caregivers. Addressing emotional well-being proactively is essential in navigating the challenges posed by frontotemporal dementia and promoting overall well-being.
Personality and Mood Changes

Personality and mood changes manifest prominently in the behavioral variant of frontotemporal dementia, impacting individuals' social interactions and relationships significantly. Individuals may exhibit disinhibition, apathy, loss of empathy, and inappropriate social behaviors, leading to challenges in their daily interactions. These changes can be distressing for both the individual with frontotemporal dementia and their caregivers, as they may struggle to comprehend and cope with the altered behaviors.
| Personality Changes | Mood Changes | Behavioral Interventions |
|---|---|---|
| Disinhibition | Apathy | Cognitive Behavioral Therapy |
| Loss of Empathy | Inappropriate Social Behaviors | Structured Daily Routine |
| Social Withdrawal | Emotional Lability | Medication Management |
Managing these personality and mood changes often involves a combination of behavioral interventions, counseling, and medications tailored to address specific symptoms. It is crucial to provide support not only for the individual with frontotemporal dementia but also for their caregivers, to navigate the complexities of these behavioral changes with empathy and understanding.
Severe Cognitive Decline

Severe cognitive decline in frontotemporal dementia results in profound memory loss and impaired decision-making abilities. Individuals at this stage often struggle with basic daily activities, necessitating extensive support for personal care. Communication difficulties become more pronounced, with challenges in both expressing thoughts and understanding language. Moreover, behavioral changes can escalate significantly, leading to increased agitation, aggression, and social withdrawal.
In the late stage of frontotemporal dementia characterized by severe cognitive decline, individuals typically require 24-hour care and support. It's essential to provide a safe and structured environment to manage the profound impact of memory loss and impaired decision-making. Moreover, communication strategies should be adapted to accommodate the increasing difficulties in expressing and understanding language.
As caregivers and healthcare providers, our focus shifts towards ensuring the individual's comfort and safety while navigating the complexities of severe cognitive decline in frontotemporal dementia. By addressing the unique challenges presented in this stage, we can strive to enhance the quality of life for those affected.
Frequently Asked Questions
How Long Does a Person With Frontal Lobe Dementia Live?
We can expect variations in the life expectancy of individuals with frontal lobe dementia, influenced by personal factors and disease progression. On average, those with this condition typically live around 6 to 8 years following diagnosis.
Studies indicate that survival rates for FTD may be shorter compared to other forms of dementia. Factors like age at onset, FTD subtype, and overall health can impact the lifespan.
Quality care, symptom management, and support from caregivers can enhance life quality and possibly extend life expectancy.
How Fast Does Frontotemporal Dementia Progress?
We've got the scoop on how fast frontotemporal dementia progresses. The speed can vary widely, influenced by factors like subtype and individual characteristics.
Early signs might go unnoticed, delaying diagnosis and treatment. As it advances, cognitive and behavioral changes intensify, affecting daily life.
In later stages, severe cognitive decline demands extensive care. The progression rate fluctuates, making each journey unique.
What Are the Final Stages of Frontal Lobe Dementia?
In the final stages of frontotemporal dementia, individuals face profound challenges. Severe cognitive decline, behavioral disturbances, and increased risk of infections like pneumonia are common. As the disease progresses, 24-hour care becomes essential.
Relationships may suffer, and daily functioning is severely impacted. Comprehensive support is crucial during this difficult stage.
What Is the Most Prominent Symptom of Frontotemporal Dementia?
The most prominent symptom of frontotemporal dementia is the significant behavioral changes individuals experience. These changes can manifest as apathy, disinhibition, and loss of empathy, impacting daily interactions and relationships.
Understanding and managing these behavioral shifts are crucial in providing effective care and support for those affected by frontotemporal dementia. Early recognition and intervention can help individuals navigate these challenges and enhance their quality of life.
Conclusion
In conclusion, navigating the seven stages of frontotemporal dementia can be a challenging journey for both patients and caregivers.
Early detection and intervention are essential in managing the progression of this complex disease.
With a combination of medications, therapy, and support, individuals can strive to maintain quality of life and functionality.
While the road ahead may seem daunting, remember that with determination and perseverance, we can conquer even the most formidable of obstacles.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Dementia Care
What Role Does Depakote Play in Managing Dementia Symptoms?
Fascinating insights into Depakote's potential for managing dementia behaviors will challenge your perceptions – find out more!

Investigating the possible benefits of using Depakote to address difficult behaviors linked to dementia involves delving into the intricacies of its off-label usage. Although some caregivers and medical professionals have observed enhancements in mood and reduction in aggression among individuals with Alzheimer’s disease, the efficacy of Depakote in easing behavioral symptoms of dementia is still a subject of debate.
By delving into the mechanisms of action, efficacy in cognitive function, and considerations for use, we can gain a better understanding of the role Depakote plays in the management of dementia-related behaviors.
Key Takeaways
- Depakote benefits mood, aggression, seizures in Alzheimer's.
- Enhances GABA levels, modulates neurotransmitters for behavioral symptoms.
- Limited efficacy in cognitive function improvement.
- Requires careful monitoring for side effects and dosage adjustments.
Benefits of Depakote for Dementia
Despite its limited efficacy in treating challenging behaviors associated with dementia, Depakote (divalproex sodium) is sometimes prescribed to Alzheimer's patients, given its potential benefits in managing certain symptoms. While it may not significantly reduce agitation or behavioral symptoms, some clinical evidence suggests that Depakote could be beneficial in addressing specific symptoms associated with dementia.
In a clinical setting, healthcare providers may consider prescribing Depakote to manage symptoms like mood changes, aggression, or certain types of seizures that can occur in Alzheimer's patients.
Although the primary use of Depakote isn't for treating dementia-related behavioral issues, some patients may experience improvements in specific symptoms, leading to an overall enhancement in their quality of life. Careful monitoring is essential due to the potential side effects, such as drowsiness and dizziness, which can impact the daily functioning of Alzheimer's patients. By weighing the clinical effects and side effects of Depakote, healthcare professionals can make informed decisions about its usage in dementia patients.
Mechanism of Action
The mechanism of action of Depakote involves enhancing the neurotransmitter GABA in the brain to stabilize mood. This modulation of GABA levels is crucial in managing challenging behaviors associated with dementia, especially in Alzheimer's patients. Divalproex sodium, the active ingredient in Depakote, acts on neuronal pathways, impacting various neurotransmitters to help reduce aggressive behavior and alleviate behavioral disturbances common in dementia. Understanding how Depakote works at a neurochemical level provides valuable insights for caregivers and healthcare providers when developing tailored treatment strategies for individuals experiencing behavioral changes related to dementia.
Key Points:
- Depakote enhances GABA levels in the brain to stabilize mood.
- Divalproex sodium impacts neuronal pathways to alleviate behavioral disturbances.
- Modulation of neurotransmitters by Depakote helps reduce aggressive behavior in Alzheimer's patients.
- The mechanism of action of Depakote is essential in managing challenging behaviors in dementia.
Efficacy in Cognitive Function
When evaluating the efficacy of Depakote in cognitive function for individuals with dementia, research findings consistently indicate a lack of significant improvement in cognitive abilities. Studies on Valproate therapy have shown that it doesn't slow cognitive decline or enhance cognitive function in dementia patients. Cognitive assessments of individuals undergoing Valproate treatment haven't demonstrated notable positive changes in cognitive performance.
Despite its effectiveness in managing behavioral symptoms, Depakote isn't considered a medication for improving cognitive function in dementia patients. Research suggests that Valproate treatment doesn't lead to cognitive improvement and is generally ineffective in addressing cognitive symptoms associated with dementia. Therefore, when considering the use of Depakote in patients with dementia, it's crucial to understand that its primary role lies in managing behavioral aspects rather than fostering cognitive enhancement.
Managing Behavioral Symptoms

Valproate (Depakote) is occasionally prescribed off-label for managing challenging behavioral symptoms in dementia. When considering the use of Depakote for behavioral symptoms in dementia, healthcare providers should keep the following points in mind:
- Limited Efficacy: Research studies suggest that Valproate may not be more effective than a placebo for reducing challenging behaviors in dementia. Therefore, its use should be carefully evaluated based on individual patient needs.
- Common Side Effects: Common side effects of Depakote include drowsiness and dizziness. More severe effects such as liver damage are also possible, emphasizing the importance of monitoring patients closely.
- Dosage Adjustment: Depakote dosage is typically initiated at a low level and adjusted gradually based on the patient's response. Healthcare providers should closely monitor patients for both therapeutic effects and adverse reactions.
- Regular Monitoring: Regular monitoring by healthcare providers is essential to assess the effectiveness and side effects of Depakote in managing behavioral symptoms of dementia. This monitoring ensures optimal outcomes and patient safety.
Considerations and Side Effects
Considering the limited efficacy and common side effects associated with Depakote for managing challenging behaviors in dementia, careful consideration of alternative strategies is crucial for optimal patient care.
Depakote, also known as divalproex sodium, has been shown to be generally ineffective in treating challenging behaviors in dementia, as studies suggest that Valproate isn't more effective than a placebo. Common side effects of Depakote include drowsiness and dizziness, while more severe side effects such as liver damage and pancreatitis can occur.
When using Depakote for agitation in Alzheimer's patients, healthcare providers typically start with a low dosage and gradually increase it based on the individual's response. Regular monitoring is essential to evaluate both the effectiveness and potential side effects of Depakote, allowing for necessary adjustments in dosage to optimize patient outcomes.
Healthcare providers play a critical role in monitoring and assessing the use of Depakote in dementia patients to ensure safe and effective care.
Frequently Asked Questions
What Do They Give Dementia Patients to Calm Them Down?
When dementia patients exhibit agitation or aggression, healthcare providers may prescribe medications to help manage these behaviors. These medications aim to calm the individual and improve their quality of life.
It's essential to monitor the patient's response to the medication and report any changes to the healthcare team promptly. Caregivers play a crucial role in observing the effectiveness and potential side effects of these medications to ensure the best care for the patient.
What Is Depakote Used for in the Elderly?
In the elderly, Depakote is sometimes used off-label to help stabilize mood and reduce aggressive behavior. It's important to note that research studies suggest it may not be more effective than a placebo in treating challenging behaviors in dementia.
Common side effects include drowsiness and dizziness, with more serious effects like liver damage and pancreatitis.
Dosage typically starts low and is gradually increased based on individual response, with regular monitoring by healthcare providers essential.
What Are Mood Stabilizers for Dementia Patients?
Mood stabilizers for dementia patients aim to stabilize mood and reduce behavioral challenges. These medications, like Valproate, work by enhancing neurotransmitter function. While studies show limited efficacy compared to a placebo, they're still commonly used.
Starting with low doses and closely monitoring levels is crucial. Divalproex sodium, a form of Valproate, is widely prescribed for managing agitation in dementia patients. Proper administration and dosage adjustments are essential for optimal outcomes.
What Are the Top 3 Drugs for Dementia?
We believe the top 3 drugs commonly used for dementia are:
- Cholinesterase inhibitors like Donepezil (Aricept)
- Memantine (Namenda)
- Antipsychotics such as risperidone (Risperdal).
These medications are tailored to address memory issues, regulate brain activity, and manage challenging behaviors in dementia patients.
It's crucial for healthcare providers to closely monitor the effects and potential side effects of these drugs to ensure optimal care for individuals with dementia.
Conclusion
In conclusion, while Depakote may offer some benefits for managing challenging behaviors in dementia patients, its efficacy is limited and comes with potential side effects. Caregivers should approach its use cautiously, monitoring for any changes in behavior or mood.
Symbolically, Depakote is like a delicate balance beam, requiring careful attention and adjustment to ensure the safety and well-being of those navigating the complexities of dementia care.
Open communication with healthcare providers is key to addressing any concerns promptly.
-

 Financial2 days ago
Financial2 days agoWho Pays for Hospice Room and Board? A Complete Guide
-

 Activities6 days ago
Activities6 days ago10 Engaging Activities for Dementia: Expert Ideas to Try Today
-

 Dementia Care5 hours ago
Dementia Care5 hours agoManaging Dementia Symptoms: Trazodone Guide
-
 Dementia Care1 day ago
Dementia Care1 day agoWhat Causes Reversible Dementia and How Can It Be Treated?
-

 Caregiving Issues7 days ago
Caregiving Issues7 days agoHow Many Hours of Respite Care Are You Allowed?
-

 Behavior Modification7 days ago
Behavior Modification7 days ago10 Essential Dementia Behavior Training Tips for Caregivers
-

 Caregiving Issues7 days ago
Caregiving Issues7 days agoWhat Is Respite Care for Elderly?
-

 Dementia Care1 day ago
Dementia Care1 day agoManaging Weight Loss in Dementia Patients