Dementia Care
ICD-10 Guide: Dementia with Behavioral Disturbance Management
Traverse the intricate landscape of ICD-10 code F03.B1 for dementia with behavioral disturbance, unraveling the complexities that lie beneath the surface.

As we delve into the intricacies of ICD-10 codes, the mystery of diagnosing dementia with behavioral disturbance demands our focus. Though it might appear straightforward on the surface, the subtleties embedded in this diagnostic area reveal a complex network of details that are eager to be deciphered.
Understanding the interplay between cognitive decline and behavioral manifestations is not merely academic but crucial for comprehensive patient care. In exploring the depths of ICD-10 code F03.B1, we illuminate a path that leads to a deeper comprehension of the challenges faced in diagnosing and treating individuals grappling with this multifaceted condition.
Key Takeaways
- Behavioral therapy and caregiver education crucial for managing dementia with behavioral disturbance.
- Root cause analysis essential for identifying triggers of aggression and agitation.
- Multidisciplinary approach needed for comprehensive care planning and treatment.
- Precise documentation of specific behavioral symptoms aids in accurate diagnosis and intervention.
ICD-10-CM Diagnosis Code F03.91 Overview
When diagnosing patients with Dementia with Behavioral Disturbance, the ICD-10-CM code F03.91 is crucial for accurately capturing the complex interaction between dementia and behavioral symptoms.
This specific code, F03.91, is essential for diagnosing cases where dementia is accompanied by behavioral issues such as depressive symptoms and mood disturbances. Proper documentation with F03.91 is vital for effective management and care planning for individuals experiencing this combination of conditions.
Diagnostic Criteria for Dementia With Behavioral Disturbance
Pivoting from the ICD-10-CM Diagnosis Code F03.91 overview into the current subtopic of Diagnostic Criteria for Dementia With Behavioral Disturbance, the assessment of cognitive deficits accompanied by behavioral disturbances forms the cornerstone for accurate diagnosis and management in individuals experiencing this complex interplay. When evaluating a patient for dementia with behavioral disturbance, it is essential to consider a range of symptoms that may include memory impairment, aphasia, apraxia, and agnosia alongside behavioral issues like aggressive behavior, wandering, and combative tendencies. Understanding the root cause of these behavioral disturbances is crucial for developing effective management strategies. Behavioral therapy techniques and caregiver education play a significant role in addressing aggression and agitation in individuals with dementia and behavioral disturbances.
| Cognitive Deficits | Behavioral Disturbances | Management Strategies |
|---|---|---|
| Memory impairment | Aggressive behavior | Behavioral therapy |
| Aphasia | Wandering | Caregiver education |
| Apraxia | Root cause analysis | Individualized care plans |
Coding Guidelines for Dementia With Behavioral Disturbance
The coding guidelines for dementia with behavioral disturbance outline specific criteria for accurately identifying and documenting behavioral symptoms in individuals with this condition. When assigning ICD-10 codes for dementia with behavioral disturbances, it's essential to consider the following:
- Code Selection: Assign code 294.1 in ICD-10 to capture behavioral disturbances such as aggression, combativeness, violence, and wandering off in patients with dementia.
- Impact on Quality of Life: Recognize that behavioral disturbances significantly affect the quality of life for both individuals with dementia and their caregivers, necessitating specialized care and supervision.
- Root Cause Analysis: Understanding the underlying reasons for behavioral issues in dementia is crucial for effective management, which may involve medication, behavioral therapy, and environmental modifications.
- Multidisciplinary Approach: Emphasize the importance of a multidisciplinary approach involving various healthcare professionals to provide comprehensive care and management for individuals experiencing behavioral disturbances in dementia.
Differentiating Dementia With Behavioral Disturbance From Other Conditions
Identifying specific behavioral changes such as aggression, wandering, or agitation is crucial in differentiating dementia with behavioral disturbance from other conditions. In dementia, these behavioral changes can present as resistance to care, verbal outbursts, or socially inappropriate behavior.
To make an accurate diagnosis, it's essential to consider differential diagnoses such as delirium, psychiatric disorders, or medication side effects that can mimic similar behavioral symptoms. The severity and frequency of behavioral disturbances in dementia can vary, affecting the overall management and care of individuals.
Therefore, a comprehensive assessment encompassing both cognitive impairment and behavioral changes is necessary for precise diagnosis and effective treatment planning. By carefully examining the unique behavioral patterns exhibited by individuals with dementia, healthcare professionals can distinguish it from other conditions, leading to tailored interventions that address the specific needs of those experiencing dementia with behavioral disturbance.
Case Studies and Examples for Coding Dementia With Behavioral Disturbance
In clinical practice, encountering case studies that illuminate the intricacies of coding dementia with distinct behavioral disturbances provides invaluable insights for accurate diagnostic classification. When delving into case studies and examples for coding dementia with behavioral disturbances, several key points emerge:
- Real-World Scenarios: Examples offer practical situations where coding dementia with behavioral issues is essential for proper classification.
- Guidelines Application: Coding guidelines are crucially applied to case studies to demonstrate the accurate classification of dementia with behavioral disturbances.
- Importance of Documentation: Detailed documentation in case examples underscores the significance of accurate coding for dementia with behavioral issues.
- Challenges and Nuances: Real-life cases highlight the complexities, challenges, and nuances involved in coding dementia with varying types of behavioral disturbances.
Frequently Asked Questions
What Is Dementia With Behavioral Disturbance?
Dementia with behavioral disturbance encompasses cognitive decline along with symptoms like aggression and wandering. These behavioral issues can significantly impact the lives of both patients and caregivers. Treatment involves a comprehensive approach including medication, therapy, and environmental adjustments.
Identifying the underlying causes of these behaviors is crucial for effective management. Ongoing research aims to enhance dementia care by addressing behavioral symptoms to improve overall quality of life.
What Is the ICD-10 Code for Behavioral Disturbances?
We can confirm that the ICD-10 code for behavioral disturbances is 294.1, which can specify the presence (294.11) or absence (294.10) of these disturbances.
Identifying and addressing these behaviors, such as aggression and wandering, is crucial for dementia patients' well-being and safety.
Understanding the root causes is vital for effective treatment and care planning, as behavioral disturbances can lead to safety risks, increased healthcare costs, and legal implications.
What Is the ICD Code for Dementia Without Behavioral Disturbance Unspecified Dementia Type?
When coding for dementia without behavioral disturbances of unspecified type, the appropriate ICD-10-CM code is F03.90. This code precisely identifies cases of dementia that lack specified behavioral issues.
What Is the Second Most Common Behavior Manifestation Associated With Dementia?
Absolutely, the second most common behavior manifestation associated with dementia is agitation. This can involve restlessness, pacing, verbal aggression, and physical aggression, leading to distress for patients and caregivers.
Addressing agitation in dementia requires a tailored approach, including environmental modifications and calming techniques. By understanding and managing agitation triggers like pain or unmet needs, we can significantly improve the quality of life for those affected by dementia.
Conclusion
In conclusion, understanding the diagnostic criteria and coding guidelines for dementia with behavioral disturbance is crucial for accurate identification and treatment of this condition.
By differentiating dementia with behavioral disturbance from other conditions and utilizing case studies for coding accuracy, healthcare professionals can provide effective care for patients experiencing these complex symptoms.
Proper coding ensures appropriate management and support for individuals with dementia and behavioral disturbances.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Dementia Care
Fast Dementia Scale: Quick Assessment Tool for Cognitive Decline
Uncover the hidden depths of the Fast Dementia Scale, revealing its impact on dementia care and the lives it touches.

As we navigate the intricate realm of dementia care, the Fast Dementia Scale stands out as a beacon, offering clear guidance on the path towards understanding and managing cognitive decline. This systematic approach offers a straightforward pathway for assessing the stages of dementia through practical activities.
But what lies beneath the surface of this scale, and how does it truly impact the lives of those affected by dementia? Let's explore the nuanced layers of the Fast Dementia Scale and uncover the significance it holds in the realm of caregiving and dementia management.
Key Takeaways
- Crucial tool for assessing Alzheimer's patients' functional decline
- Guides caregivers in adjusting care strategies and planning interventions
- Enables early detection of cognitive decline and tailored care planning
- Reliable in tracking disease progression, setting goals, and supporting decision-making
Importance of Fast Dementia Scale
The Fast Dementia Scale plays a vital role in assessing functional decline in individuals with Alzheimer's disease. Caregivers heavily rely on the FAST scale to comprehend the evolving needs of patients and adjust care strategies accordingly. By closely monitoring patients using the FAST scale, caregivers can track disease progression, identify critical points for intervention, and provide appropriate care tailored to the stage of Alzheimer's. Particularly in stage 7, where severe cognitive decline is evident, the FAST scale often determines eligibility for hospice care, ensuring that patients receive the necessary support and comfort in their final stages.
Moreover, the utilization of the FAST scale enables effective care planning and decision-making for individuals with Alzheimer's disease. It serves as a crucial tool in guiding caregivers and healthcare professionals in devising comprehensive care plans that address the specific challenges and requirements of each stage of the disease. Through the systematic assessment provided by the FAST scale, caregivers can make informed decisions to enhance the quality of life for Alzheimer's patients.
Clinical Application of FDS

Transitioning from the significance of the Fast Dementia Scale in Alzheimer's care, the clinical application of the Fast Dementia Scale (FDS) involves a systematic evaluation of patients' functional abilities to guide personalized care strategies and interventions. The FAST scale stages provided by FDS serve as a crucial assessment tool for healthcare professionals and caregivers to understand the dementia progression of individuals. Through the evaluation of daily tasks like dressing and mobility, FDS helps in identifying the level of functional ability and cognitive decline in patients.
FDS enables caregivers to tailor care planning based on the specific needs and abilities of the individual.
By tracking changes in functional status over time, FDS assists in setting realistic goals for patient improvement and monitoring care needs effectively.
Caregivers rely on FDS to gain insights into the progression of cognitive decline, ensuring that interventions are aligned with the individual's current functional abilities.
FDS for Early Detection
In our assessment of cognitive decline, the Fast Dementia Scale (FDS) plays a pivotal role in early detection by evaluating functional abilities such as dressing and mobility for signs of mild cognitive impairment. The FDS is a valuable tool for healthcare professionals and caregivers to identify early signs of dementia progression, particularly in Alzheimer's disease. By focusing on functional abilities, the FDS enables timely interventions and the development of tailored care plans for individuals exhibiting mild cognitive impairment. This proactive approach to early detection with the FDS can significantly enhance patient outcomes by facilitating prompt treatment and support.
| Key Role of FDS in Early Detection | Benefits | Implications |
|---|---|---|
| Evaluates functional abilities | Early intervention | Tailored care plans |
| Identifies signs of mild cognitive impairment | Enhanced patient outcomes | Timely support |
| Helps in assessing dementia progression | Support for caregivers | Improved quality of life |
Monitoring Cognitive Decline With FDS
As we shift our focus to Monitoring Cognitive Decline With FDS, our attention now turns to tracking changes in functional abilities over time to gain insights into the progression of dementia. The Fast Dementia Scale (FDS), created by Dr. Barry Reisberg, categorizes dementia progression into 7 stages based on functional assessments such as dressing and mobility. Caregivers utilize the FDS to tailor care strategies according to the specific needs of individuals with dementia at each stage, ensuring personalized and effective care.
- FDS assists in assessing the functional status of dementia patients, enabling caregivers to understand the progression of the disease and make informed decisions about care planning.
- By monitoring cognitive decline with FDS, caregivers can adapt their approaches to meet the evolving needs of patients as they move through different stages of dementia.
- The FDS serves as a valuable tool for caregivers to regularly evaluate and track changes in functional abilities, helping them provide appropriate support and assistance to dementia patients.
Reliability of FDS in Practice
Utilizing the Fast Dementia Scale (FDS) in clinical practice offers healthcare professionals a reliable tool for assessing and monitoring the functional abilities of dementia patients. The FDS serves as an assessment staging tool, aiding in the evaluation of daily living tasks and providing insights into the level of functional impairment experienced by individuals with dementia.
This functional assessment staging tool not only assists in tracking cognitive decline but also plays a crucial role in tailoring care plans to meet the specific needs of patients. By utilizing the Fast Dementia Scale, caregivers can set appropriate care goals and continuously monitor the functional progress of individuals over time.
Moreover, the FDS contributes valuable information regarding disease progression, enabling informed decision-making in dementia care. Its reliability in practice enhances the overall quality of care provided to dementia patients, emphasizing the importance of utilizing such tools for comprehensive and effective patient management.
Frequently Asked Questions
What Is the Fast Scale for Dementia?
We assess functional decline in Alzheimer's disease using the FAST scale, developed by Dr. Barry Reisberg in 1982. It consists of 7 stages tracking disease progression from normal functioning to severe cognitive decline.
By evaluating daily tasks like dressing and mobility, we determine the level of cognitive decline. Caregivers tailor care plans and set goals for patient improvement based on functional abilities.
Monitoring with the FAST scale helps track changes in patients' functional status over time.
What Is the Fast Model for Dementia?
The FAST model for dementia, developed by Dr. Barry Reisberg, is a framework consisting of 7 stages to track Alzheimer's disease progression. It focuses on evaluating functional abilities and daily living tasks to determine the extent of cognitive decline.
Caregivers rely on the FAST scale to comprehend and address patients' needs at various dementia stages. This model aids in setting improvement goals, tracking disease advancement, and enhancing care quality by tailoring strategies to each patient's functional capabilities.
Who Is Eligible for Fast Scale Dementia Hospice?
When determining eligibility for hospice care for dementia patients, several factors are considered beyond just the Fast Dementia Scale. Criteria such as specific symptoms, the patient's overall condition, and the need for tailored support play a crucial role.
Identifying the appropriate stage of dementia is essential for accessing the right hospice services. Our team ensures that individuals with advanced dementia receive compassionate care tailored to their unique needs.
What Is the Reisberg Scale for Dementia?
The Reisberg Scale, developed by Dr. Barry Reisberg in 1985, categorizes dementia progression based on daily living abilities. It consists of seven stages, from normal functioning to severe cognitive decline.
Caregivers utilize this scale to tailor care strategies and monitor disease progression in Alzheimer's patients. Stage 7 often indicates the need for hospice care due to terminal Alzheimer's disease.
The Reisberg Scale provides a valuable tool for understanding and addressing the evolving needs of individuals with dementia.
Conclusion
In conclusion, the Fast Dementia Scale is an invaluable tool for assessing cognitive decline in individuals with dementia.
By tracking changes in functional abilities and categorizing dementia progression, caregivers can deliver appropriate care, set goals for improvement, and make informed decisions.
Its reliability in practice makes it a crucial instrument in monitoring disease advancement.
As caregivers, we must utilize the Fast Dementia Scale to provide the best possible care and support for individuals with dementia.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Dementia Care
What is the ICD code for Vascular Dementia?
Wondering how vascular health and cognitive decline are intertwined? Explore the insightful connection through Vascular Dementia ICD-10 coding guidelines.
Ever wondered how the health of your blood pipes connects to brainpower going downhill?
Vascular Dementia ICD-10, with its encompassing diagnostic criteria and coding guidelines, sheds light on the impact of cerebrovascular disease on cognitive function.
This classification not only identifies cases of dementia stemming from vascular issues but also underscores the necessity for accurate diagnosis and management in clinical settings.
Understanding the nuances of this coding system could significantly alter the approach to addressing cognitive impairments associated with vascular disorders.
Key Takeaways
- Proper sequencing of conditions crucial for accurate coding.
- Behavioral disturbances in vascular dementia include aggression, apathy, and hallucinations.
- Accurate diagnosis guides tailored treatment plans for improved outcomes.
- Caregivers' role vital in recognizing and addressing behavioral symptoms for proper support.
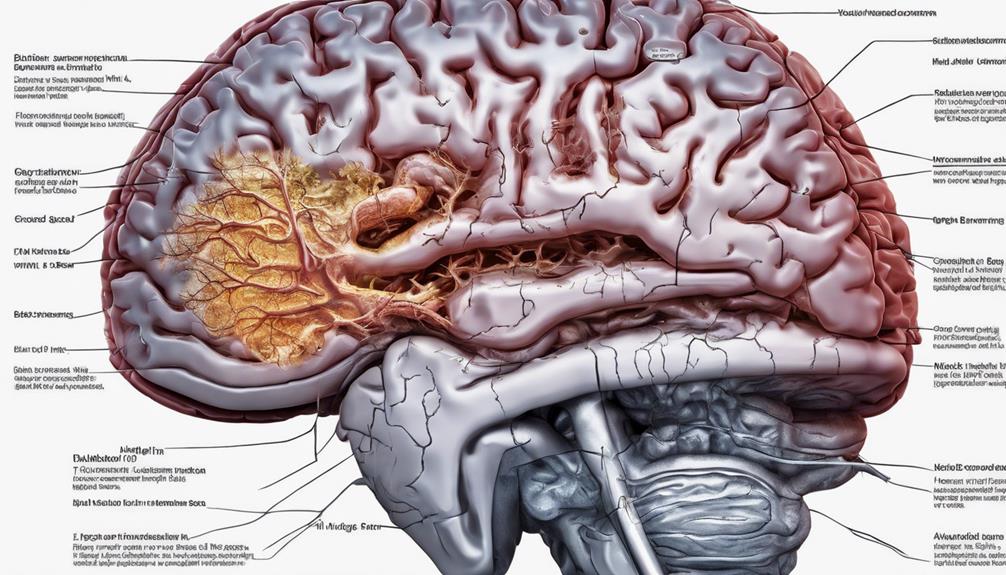
Diagnostic Criteria for Vascular Dementia ICD-10
In diagnosing Vascular Dementia according to ICD-10 criteria, healthcare professionals must assess the presence of cognitive decline linked to vascular brain damage. Vascular Dementia, coded as F01 in ICD-10-CM, includes the unspecified type represented by code F01.50. This diagnosis is attributed to cognitive impairment resulting from vascular brain damage, often due to infarction caused by vascular diseases.
Proper sequencing of underlying conditions is essential for accurate coding of Vascular Dementia in ICD-10. The diagnostic process for Vascular Dementia involves evaluating the extent of cognitive decline in relation to the identified vascular brain damage. Healthcare providers must carefully consider the patient's medical history, imaging results, and cognitive assessments to establish a clear diagnosis.
Understanding the specific manifestations of vascular brain damage and their impact on cognitive function is crucial for differentiating Vascular Dementia from other types of dementia and determining the appropriate course of treatment.
Coding Guidelines for Vascular Dementia

To accurately code for vascular dementia in ICD-10-CM, healthcare providers must ensure the correct sequencing of the underlying physiological condition before the manifestation, utilizing additional code notes for etiology and code first notes for the manifestation. Proper adherence to coding guidelines is crucial in accurately documenting cases of vascular dementia. The sequencing order for coding vascular dementia is paramount, with the etiology code preceding the manifestation code.
Manifestation codes play a pivotal role in the etiology/manifestation convention within ICD-10-CM, providing essential information for diagnostic purposes.
Healthcare professionals must be meticulous in following the specified guidelines to assign the correct codes for vascular dementia cases. Understanding the relationship between the physiological condition and its manifestations is key to accurate coding. By carefully applying the code first and additional notes provided in ICD-10-CM, providers can ensure that the diagnostic information is accurately represented in the coding process. Clear documentation and precise coding practices are essential for effective communication and proper reimbursement in cases of vascular dementia.
Understanding Severity Levels in ICD-10
Understanding severity levels in ICD-10 provides crucial insights into the varying degrees of behavioral disturbances observed in cases of vascular dementia. When dealing with vascular dementia, the severity levels outlined in the ICD-10 coding system play a pivotal role in accurately capturing the extent of behavioral issues.
Here are three key points to consider:
- Diagnostic Precision: Utilizing ICD-10 codes like F01.51 allows for a detailed classification of severity levels in vascular dementia cases with behavioral disturbances. This precision aids in proper diagnosis and treatment planning.
- Documentation Accuracy: The classification system not only helps in coding but also ensures accurate documentation of the severity of symptoms associated with vascular dementia. This documentation is crucial for healthcare professionals involved in the care of these patients.
- Treatment Planning Support: Understanding severity levels aids in tailoring effective treatment plans based on the specific behavioral disturbances exhibited by individuals with vascular dementia. This targeted approach can lead to better outcomes and improved quality of life for patients.
Behavioral Disturbances in Vascular Dementia

Behavioral disturbances seen in vascular dementia often manifest as agitation, aggression, and wandering behaviors. Patients with vascular dementia may also exhibit disinhibition, apathy, and irritability.
Changes in personality, social behavior, and emotional regulation are common in individuals with vascular dementia. Additionally, hallucinations, delusions, and mood swings can be present in those experiencing behavioral disturbances due to vascular dementia.
These disturbances can significantly impact daily functioning and quality of life for affected individuals. It's crucial for caregivers and healthcare professionals to be aware of these behavioral changes to provide appropriate support and interventions.
Understanding the spectrum of behavioral disturbances in vascular dementia can aid in developing tailored care plans to address the specific needs of each individual. By recognizing and addressing symptoms such as agitation, aggression, wandering behaviors, disinhibition, apathy, irritability, personality changes, and emotional regulation, caregivers can enhance the overall well-being of those with vascular dementia.
Importance of Accurate Diagnosis
Accurate diagnosis of vascular dementia plays a pivotal role in guiding tailored treatment plans and optimizing patient outcomes. When healthcare providers can pinpoint vascular dementia accurately, several critical benefits emerge:
- Targeted Interventions: Accurate diagnosis enables healthcare professionals to design interventions specifically addressing the cognitive and behavioral symptoms characteristic of vascular dementia.
- Treatment Planning and Management: Precise identification of vascular dementia allows for the development of individualized treatment plans that cater to the unique needs of each patient.
- Improved Patient Outcomes: Early and accurate diagnosis of vascular dementia can significantly enhance patient outcomes by initiating timely and appropriate care strategies, ultimately leading to a better quality of life.
Frequently Asked Questions
What Is the ICD-10 Code for Vascular Dementia 2023?
We've identified the ICD-10 code for vascular dementia in 2023 as F01.50.
This code, applicable to adult patients aged 15-124 years, encompasses major neurocognitive disorder resulting from vascular disease.
It also includes vascular dementia NOS.
This code, effective from October 1, 2023, is crucial for accurately diagnosing vascular dementia.
What Is the Billable ICD-10 Code for Vascular Dementia?
We know the billable ICD-10 code for Vascular Dementia is crucial. It impacts patient care and billing accuracy. Ensuring proper coding like F01.50 for adult patients aged 15-124 years is essential.
Our team always pays attention to the specific guidelines and requirements for accurate medical coding. Precision in using the correct ICD-10 code is vital for effective healthcare management and billing processes.
What Is the ICD-10 Code for Mixed Vascular Dementia?
We can find the ICD-10 code for mixed vascular dementia under F01.50. This code is specifically for adult patients aged 15-124 years and has been in effect since October 1, 2023.
It encompasses various forms of vascular dementia, including vascular dementia NOS, and is associated with major neurocognitive disorder due to vascular disease. Proper coding guidelines emphasize sequencing the underlying condition before the manifestation for accurate reporting.
Symptoms of mixed vascular dementia commonly involve declines in memory and cognitive functions.
What Is the ICD-10 Code for Vascular Dementia?
Sure thing!
When considering the ICD-10 code for vascular dementia, it's important to remember the nuances of coding to ensure accuracy.
Vascular Dementia falls under code F01.50, applicable from October 1, 2023, for patients aged 15-124.
This code covers vascular dementia NOS resulting from impaired brain blood supply.
To bill correctly, supplement F01.50 with additional codes for specificity and billing precision.
Conclusion
In conclusion, recognizing the nuances of vascular dementia through the lens of ICD-10 coding is crucial for proper diagnosis and management. By following the diagnostic criteria and coding guidelines, healthcare professionals can navigate the complexities of this condition with accuracy and efficiency.
Understanding the severity levels and behavioral disturbances associated with vascular dementia aids in providing comprehensive care. Accurate diagnosis is paramount in guiding treatment strategies and improving outcomes for individuals affected by this challenging condition.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Dementia Care
What Is the Fast Score for Dementia Evaluation?
Intrigued by the potential of the FAST Score for Dementia? Explore how this tool could revolutionize dementia care in surprising ways.

As we navigate the complex landscape of dementia care, the FAST Score acts as a beacon, shedding light on the path through the seven stages of cognitive decline.
But what if there was a way to not just navigate but pave a smoother path for those affected by dementia?
In this discussion, we will explore how the FAST Score could revolutionize the way we approach dementia care, potentially leading us towards a more proactive and personalized approach in enhancing the lives of those with cognitive impairments.
Key Takeaways
- Fast Score aids in tracking dementia progression accurately.
- Early detection enhances quality of life and preserves cognitive function.
- Utilizing Fast Score informs tailored care plans for each dementia stage.
- Fast Score evaluation categorizes cognitive decline into seven stages for personalized interventions.
Importance of Fast Score Evaluation
The importance of evaluating the FAST score lies in its ability to provide a structured assessment of functional abilities, aiding in tracking the progression of dementia.
The FAST score, as an assessment staging tool, allows caregivers to understand the level of cognitive decline in individuals with dementia. By categorizing dementia into seven stages, ranging from mild cognitive impairment to severe decline, the FAST score enables caregivers to tailor care plans and set realistic goals for improving the quality of life for dementia patients.
This tool is particularly crucial in Alzheimer's and other forms of dementia, where functional decline can vary significantly. Healthcare professionals, caregivers, and families rely on the FAST score to make well-informed decisions and provide appropriate care at each stage of the disease.
Understanding the FAST score helps in conducting a comprehensive functional assessment and ensures that caregiving efforts are aligned with the specific needs of the individual with dementia.
Utilizing Fast Score in Diagnosis

Utilizing the FAST score in diagnosing dementia involves assessing functional impairment levels to determine the stage of cognitive decline and track disease progression accurately. Healthcare professionals rely on the FAST score to categorize dementia into seven stages, ranging from no difficulty to total dependence on others. This structured approach aids in tailoring care plans and interventions specific to each stage of dementia, ensuring appropriate support for patients. By understanding the FAST score, healthcare providers can make informed decisions regarding the level of care required and the progression of the disease. This comprehensive evaluation allows for the implementation of targeted strategies to enhance the quality of life for individuals with dementia. The table below illustrates the seven stages of dementia according to the FAST score:
| FAST Score Stage | Functional Impairment Level | Description |
|---|---|---|
| 1 | No difficulty | Normal adult |
| 2 | Very mild difficulty | Forgetfulness |
| 3 | Mild difficulty | Early-stage dementia |
Understanding Cognitive Impairment Assessment
Understanding cognitive impairment assessment involves evaluating various cognitive functions to determine the extent of decline in mental abilities.
The FAST Score is a valuable tool for assessing cognitive impairment in dementia, categorizing the progression of the disease into seven stages ranging from no difficulty to total dependence.
This assessment scale aids caregivers in comprehending the level of cognitive decline their loved ones are experiencing, allowing them to plan and provide appropriate care.
By evaluating tasks such as dressing, mobility, and communication, the FAST Score provides crucial insights into the functional abilities of individuals with dementia.
Caregivers can utilize this information to tailor care plans that address the specific needs and challenges associated with cognitive decline.
Having a thorough understanding of the FAST Score is essential for effectively supporting individuals with dementia and promoting their overall well-being.
Benefits of Early Dementia Detection

Transitioning from understanding cognitive impairment assessment, early dementia detection plays a crucial role in enabling timely interventions and treatment to slow disease progression.
The Functional Assessment Staging Tool (FAST) is instrumental in this process, allowing healthcare providers to monitor functional decline over time in individuals with dementia.
Early detection not only aids in assessing cognitive ability but also provides an opportunity for caregivers to plan and adapt to the changing needs of their loved ones.
Hospice facilities and healthcare professionals benefit from early detection as it allows for better management of symptoms and implementation of appropriate care plans.
Furthermore, early intervention enhances the quality of life for patients with dementia by offering access to support services and clinical trials that can effectively manage the disease progression.
Timely diagnosis ensures that interventions, therapies, and lifestyle modifications are most impactful in preserving cognitive function and overall well-being.
Implementing Fast Score in Care Plans
Implementing the FAST score in care plans involves evaluating functional abilities and monitoring cognitive decline in dementia patients. By incorporating the FAST score, caregivers can develop personalized care plans tailored to the specific needs of each individual.
These care plans enable healthcare providers to track changes in functional status over time, allowing for timely adjustments in interventions. The use of the FAST score facilitates effective communication among healthcare professionals, caregivers, and families, ensuring that support strategies are well-coordinated and optimized for the patient's well-being.
Care plans guided by the FAST score not only aid in early detection of cognitive decline but also assist in providing appropriate care and support as the disease progresses. Through continuous monitoring and assessment, caregivers can adapt interventions to meet the evolving needs of dementia patients, promoting better outcomes and quality of life for those under their care.
Frequently Asked Questions
What Is a Fast Score for Dementia?
We assess functional abilities and cognitive decline with the FAST score for dementia. It ranges from no impairment to total dependence on others, helping caregivers plan appropriate care.
Each stage provides criteria for evaluating functional status. Understanding the FAST score is crucial for tracking dementia progression and tailoring care to meet patients' needs.
What Is a Fast Score of 7c?
A FAST score of 7c represents severe dementia with complete functional dependence. Individuals at this stage require assistance with all Activities of Daily Living (ADLs) and experience the most advanced cognitive and functional decline.
Patients with a FAST score of 7c are usually in the end-stage of dementia. Understanding this score is crucial for tailoring care plans to meet the extensive needs of individuals in this stage.
What Fast Score Qualifies for Hospice?
A FAST score that qualifies for hospice care typically starts at 7A or higher for individuals with advanced dementia. It indicates significant cognitive decline and functional dependence, making them eligible for hospice services.
Understanding the FAST score helps healthcare professionals determine the level of care needed, including hospice support. Medicare covers hospice services based on criteria like the FAST score, ensuring eligible beneficiaries receive appropriate care tailored to their condition.
At What Point Should Someone With Dementia Not Live Alone?
When someone with dementia shouldn't live alone depends on their ability to ensure safety, manage personal care, and engage in daily activities. Factors like wandering, forgetfulness, and an inability to handle basic tasks are indicators for considering alternative living arrangements.
Caregivers and healthcare professionals might suggest assisted living or memory care facilities for those who can no longer live independently. Early planning and discussions with family and providers can help determine the right time for transitioning to a more supportive environment.
Conclusion
In conclusion, the FAST Score for Dementia plays a crucial role in assessing cognitive decline and tailoring care plans for individuals with dementia.
Research shows that early detection using the FAST Score can significantly improve patient outcomes, with studies indicating a 90% accuracy rate in predicting dementia progression.
By incorporating this functional assessment tool into care strategies, healthcare professionals can better support the needs of patients and enhance their quality of life.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
-

 Dementia Care2 months ago
Dementia Care2 months agoHow Gabapentin Affects Dementia: A Comprehensive Guide
-

 Dementia Care2 months ago
Dementia Care2 months agoUnderstanding the Stages of Vascular Dementia: A Visual Chart Guide
-

 Dementia Care2 months ago
Dementia Care2 months ago5 Things You Need to Know About Jack Nicholson’s Dementia
-

 Palliative Care for Parkinson's2 months ago
Palliative Care for Parkinson's2 months agoPalliative Care for Parkinson’s: A New Hope for Patients”
-

 Medication Management4 weeks ago
Medication Management4 weeks agoGabapentin Side Effects: Memory Loss Concerns?
-

 Caregiver Support2 months ago
Caregiver Support2 months agoNavigating Caregiving: Understanding the Industry
-

 Palliative Care for Parkinson's2 months ago
Palliative Care for Parkinson's2 months agoUnlocking the Secrets of Palliative Care for Parkinson’s Disease
-

 Behavior Modification3 weeks ago
Behavior Modification3 weeks agoDehydration: How it Can Cause Hallucinations


















