Brain cell damage, Alzheimer’s disease, vascular dementia, and Lewy body dementia can all lead to confusion in individuals with dementia. This damage can affect memory, thinking, and behavior. Alzheimer’s disease specifically leads to memory loss and cognitive decline. Vascular dementia is caused by reduced blood flow to the brain, while Lewy body dementia is characterized by abnormal protein deposits. Cognitive decline can be accelerated by various factors, including medical conditions and genetics. Lifestyle choices also play a role in cognitive health. Understanding these causes is crucial for managing confusion in dementia. Delving deeper into these factors can offer a better understanding of the complexity of dementia.
Key Takeaways
- Brain cell damage contributes to confusion in dementia.
- Alzheimer's disease leads to memory loss and cognitive decline.
- Vascular dementia is caused by reduced blood flow to the brain.
- Lewy Body dementia is marked by abnormal protein deposits in the brain.
- Genetics, lifestyle, and medical conditions influence dementia-related confusion.
Brain Cell Damage
Brain cell damage greatly contributes to the confusion associated with dementia, impacting memory, thinking, and behavior. When brain cells are damaged, especially in conditions like Alzheimer's disease, it can lead to a decline in cognitive functions. Nerve cells play an essential role in transmitting messages within the brain. However, when these cells are damaged, communication between neurons is disrupted, affecting memory retrieval and cognitive processes. This breakdown in communication is one of the underlying causes of the confusion experienced by individuals with dementia.
Understanding the impact of brain cell damage is essential in addressing the root causes of dementia-related confusion. The destruction of nerve cells in specific regions of the brain can result in cognitive decline, leading to memory problems and difficulties with thinking and behavior. By recognizing the role of brain cell damage in dementia, we can better comprehend the complexities of this condition and work towards providing support and care for those affected.
Alzheimers Disease
Alzheimer's Disease is a condition that leads to significant memory loss and cognitive decline. It affects specific areas of the brain responsible for memory, language, and decision-making.
Changes in routines or living arrangements can worsen the symptoms of Alzheimer's Disease.
Memory Loss
Memory loss in Alzheimer's disease gradually erodes the ability to recall recent events, leading to frustration and impaired decision-making skills. It's a progressive condition that affects brain cells, causing confusion and difficulty in remembering details.
Individuals with Alzheimer's may struggle to recognize family members or understand relationships due to severe memory loss. Medications can help manage symptoms temporarily, but they can't halt the ongoing damage to brain cells that underlies the memory loss and confusion.
Signs such as calling family members by other names, confusion about time, and forgetting important information are common in Alzheimer's patients. Understanding these memory-related challenges is important when supporting individuals with Alzheimer's and their families. Caregivers and loved ones often witness moments of disorientation that can be both challenging and heart-wrenching. Additionally, funny texting mistakes by seniors, such as confusing autocorrected words or accidentally sending emojis, can provide lighthearted moments amidst the difficulties. Understanding that these behaviors stem from the disease helps foster patience and empathy in everyday interactions.
Cognitive Decline
In the progression of cognitive decline associated with Alzheimer's disease, individuals experience a gradual erosion of their ability to recall recent events, leading to frustration and impaired decision-making skills. As Alzheimer's disease advances, memory loss and confusion worsen, affecting daily functioning and behavior. The progressive damage to brain cells in Alzheimer's results in severe memory impairment, impacting personal relationships and independence. While medications can help manage symptoms temporarily, they do not halt the underlying disease process. Changes in living arrangements or routines can exacerbate cognitive decline, making it important to provide a supportive and familiar environment for individuals with Alzheimer's. Understanding the challenges posed by cognitive decline in Alzheimer's disease can aid in developing effective care strategies.
| Alzheimer's Disease Facts | ||
|---|---|---|
| Most common cause of cognitive decline | Progressive damage to brain cells | Severe memory impairment |
Vascular Dementia
Caused by reduced blood flow to the brain, vascular dementia leads to cognitive decline. Risk factors for this condition include hypertension, diabetes, and smoking. When individuals have vascular dementia, they may experience cognitive symptoms such as difficulty with planning, organizing, and decision-making. Strokes or small vessel disease in the brain can contribute to the development of vascular dementia.
Managing underlying vascular risk factors is important in slowing down the progression of vascular dementia. Controlling conditions like hypertension and diabetes, as well as quitting smoking, can help improve the overall brain health and potentially delay cognitive decline. It's essential to consult healthcare professionals for proper diagnosis and treatment strategies tailored to individual needs.
Being aware of these risk factors and symptoms can aid in early detection and intervention, potentially improving the quality of life for those affected by vascular dementia.
Lewy Body Dementia
Lewy Body Dementia is the second most common progressive dementia. It is marked by abnormal protein deposits in the brain known as Lewy bodies. Symptoms of this condition include visual hallucinations, fluctuations in cognition, movement issues, and sleep disturbances.
Sensitivity to certain medications can lead to adverse reactions in individuals with Lewy Body Dementia. Therefore, accurate diagnosis is essential for appropriate management.
Hallucinations in Lewy Body Dementia
Hallucinations, affecting up to 80% of individuals with Lewy Body Dementia, are vivid and detailed experiences involving seeing unreal people, animals, or objects. These symptoms can be distressing for both the person with Lewy Body Dementia and their caregivers.
Managing hallucinations in Lewy Body Dementia requires a thorough approach that includes medications and non-pharmacological interventions. Caregivers play an essential role in supporting individuals experiencing these hallucinations.
Motor Impairments Associated
Motor impairments commonly seen in individuals with Lewy Body Dementia include muscle stiffness, tremors, and slow movement akin to Parkinson's disease. These symptoms can vary in intensity, affecting everyday tasks and mobility.
In addition to motor issues, Lewy Body Dementia is known for visual hallucinations and REM sleep behavior disorder. The combination of cognitive symptoms, motor challenges, and psychiatric manifestations can make diagnosing this condition complex.
Understanding the specific motor impairments associated with Lewy Body Dementia is essential for developing effective care plans and management strategies.
Cognitive Decline Factors
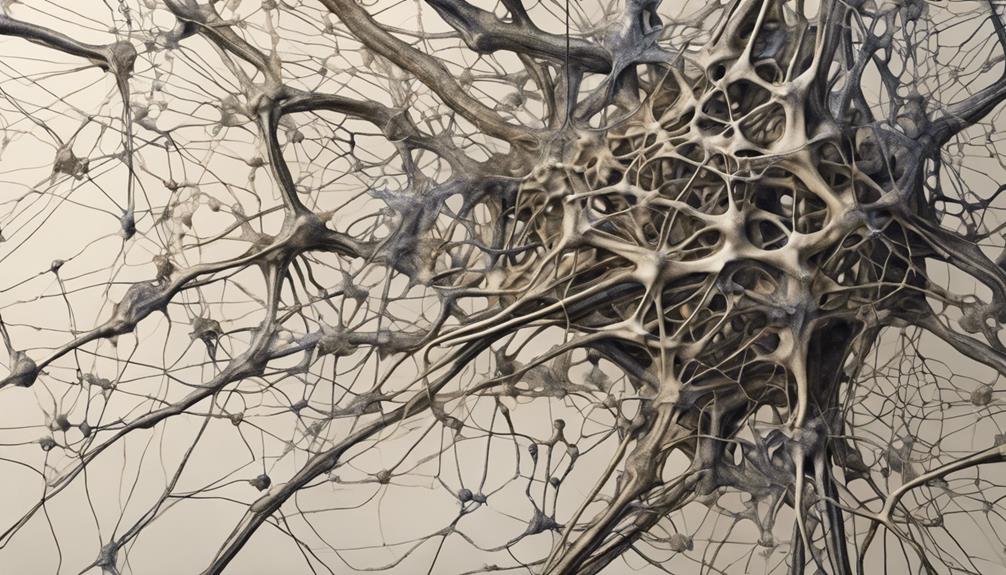
Cognitive decline factors play a significant role in contributing to the confusion experienced by individuals with dementia, stemming from progressive damage to brain cells caused by diseases like Alzheimer's. In Alzheimer's disease, changes in brain chemistry and structure can lead to memory loss and reasoning difficulties. These cognitive changes are a result of specific neurological changes that affect cognitive functions.
Factors such as inflammation, genetics, and environmental influences can accelerate cognitive decline, leading to increased confusion in individuals with dementia. Identifying and addressing these cognitive decline factors early on is vital for helping manage dementia symptoms and improve the quality of life for those affected.
Medical Conditions Influence

In considering the factors that contribute to confusion in individuals with dementia, it's important to recognize the significant impact that medical conditions can have on exacerbating cognitive impairment and disorientation. Medical conditions play a vital role in influencing the level of confusion experienced by individuals with dementia.
Here are three key ways these conditions can affect cognitive function:
- Neurological Disorders: Conditions like Parkinson's disease, multiple sclerosis, or Huntington's disease can worsen confusion and cognitive decline in people with dementia.
- Underlying Health Issues: Infections, thyroid problems, or vitamin deficiencies can contribute to cognitive impairment and confusion in dementia patients.
- Medication Side Effects: Interactions or adverse effects from multiple prescriptions, especially in older adults, can trigger confusion and cognitive impairment in individuals with dementia.
Understanding and addressing these medical conditions is essential in managing and improving the cognitive symptoms experienced by those with dementia. By identifying and treating these underlying issues, caregivers and healthcare professionals can work towards enhancing the quality of life for individuals affected by dementia.
Genetics and Dementia
Genetics greatly influence the development of dementia, with specific genes playing an important role in increasing the risk of certain types of the condition. Mutations in genes like APP, PSEN1, and PSEN2 are associated with early-onset Alzheimer's disease, a form of dementia appearing before age 65. The APOE gene, especially the APOE ε4 allele, is a significant genetic risk factor for late-onset Alzheimer's disease, the most common type of dementia. Familial Alzheimer's disease, caused by inherited genetic mutations, is responsible for a small portion of all Alzheimer's cases. Understanding the genetic aspects of dementia is important as it aids in early detection, personalized treatment plans, and genetic counseling for families at risk.
| Gene | Associated with | Type of Dementia |
|---|---|---|
| APP | Early-onset Alzheimer's | Early-onset dementia |
| PSEN1 | Mutations in PSEN1 | Early-onset Alzheimer's |
| PSEN2 | Mutations in PSEN2 | Early-onset Alzheimer's |
| APOE gene | APOE ε4 allele | Late-onset Alzheimer's |
Lifestyle and Cognitive Health
Regular physical exercise and a healthy diet play key roles in reducing the risk of developing dementia-related confusion. Engaging in mentally stimulating activities, such as solving puzzles or learning new skills, can enhance cognitive health and decrease confusion associated with dementia.
Adequate sleep and effective stress management are crucial for maintaining cognitive function and reducing confusion linked to dementia. Social interaction and nurturing strong social connections can help prevent or delay cognitive decline and confusion related to dementia.
Avoiding smoking, limiting alcohol intake, and effectively managing chronic conditions like diabetes can greatly lower the risk of developing confusion due to dementia. By incorporating these lifestyle choices into our daily routines, we can proactively work towards preventing cognitive decline and promoting overall cognitive health.
Frequently Asked Questions
What Is the Number One Trigger for Dementia Behavior?
Changes in environment or routine, like sudden shifts in caregiving practices, are the primary triggers for dementia behavior. These alterations can lead to confusion and agitation. Recognizing and minimizing environmental triggers can help manage and reduce behavioral challenges.
What Stage of Dementia Is Sundowning?
In the middle to later stages of dementia, sundowning often emerges. It can trigger confusion and agitation, mainly in individuals with memory loss. This phenomenon, believed to be linked to disruptions in our body clock, can persist into the night.
What Are Signs That Dementia Is Getting Worse?
As signs of dementia worsen, memory loss, confusion, difficulty in tasks, mood changes, communication struggles, and loss of independence become more pronounced. These changes indicate a decline in cognitive function and may require increased support and care.
What Causes Confusion in Dementia Patients?
When dementia patients experience confusion, it's due to nerve cell damage in the brain, cognitive impairment, chemical imbalances, and physical changes like plaques. Factors like Alzheimer's disease, vascular dementia, and health issues can exacerbate this confusion.
Conclusion
To sum up, dementia confusion can be triggered by various factors such as brain cell damage, Alzheimer's disease, vascular dementia, Lewy body dementia, cognitive decline factors, medical conditions, genetics, and lifestyle choices.
It's crucial to seek medical attention and make healthy lifestyle choices to help prevent or manage dementia symptoms.
By understanding the causes of dementia confusion, individuals can take proactive steps to maintain cognitive health and overall well-being.









