Genetic factors, including mutations in specific genes MAPT, GRN, and C9ORF72, play a role in 10-30% of Frontotemporal Dementia (FTD) cases. Abnormal proteins like tau and TDP-43 can cause damage to brain cells. A family history of FTD can increase the risk of inheriting the disease. Damage to the frontal and temporal lobes can impact cognitive functions. Neuronal loss in these regions can disrupt normal brain function. Understanding these causes is crucial in the management of FTD. Various types of brain damage can be identified through imaging techniques. If you would like to learn more, further details about the causes of FTD can be uncovered.
Key Takeaways
- Genetic factors like MAPT, GRN, and C9ORF72 mutations contribute to FTD.
- Abnormal protein accumulation, particularly tau and TDP-43, leads to neuronal damage.
- Family history of FTD increases the risk of developing the condition.
- Brain atrophy and damage in frontal and temporal lobes are common in FTD.
- Environmental factors such as toxins or head trauma may influence FTD onset.
Genetic Factors in FTD
Genetic factors play a significant role in the development of behavioral variant frontotemporal dementia (bvFTD), contributing to 10-30% of cases. Inherited gene variants like MAPT, GRN, and C9ORF72 are linked to genetic forms of bvFTD. Having a family history of bvFTD raises the chances of inheriting these genetic forms of the disorder.
Changes in specific genes, such as the MAPT, GRN, and C9ORF72 genes, can be identified as underlying causes of genetic bvFTD. For individuals with a family history of bvFTD, genetic testing may be advised to evaluate the risk of developing the condition.
Understanding these genetic factors is essential in determining the likelihood of developing bvFTD and can guide healthcare providers in offering appropriate support and guidance. By recognizing the impact of genetic variants and family history, we can take proactive steps towards early detection and management of bvFTD in those at risk.
Mutations in Specific Genes

Upon examining specific genes associated with frontotemporal dementia (FTD), mutations in MAPT, GRN, and C9ORF72 have been identified as key factors contributing to the development of this neurodegenerative condition.
MAPT gene mutations lead to the accumulation of abnormal tau protein in the brain, which is a hallmark of FTD. On the other hand, mutations in the GRN gene result in reduced levels of progranulin, a protein important for brain cell survival and function, consequently playing a role in FTD development.
C9ORF72 gene mutations, the most common genetic cause of familial FTD and amyotrophic lateral sclerosis (ALS), are also linked to FTD. Genetic testing can help identify these mutations, aiding in the diagnosis and understanding of the causes of FTD.
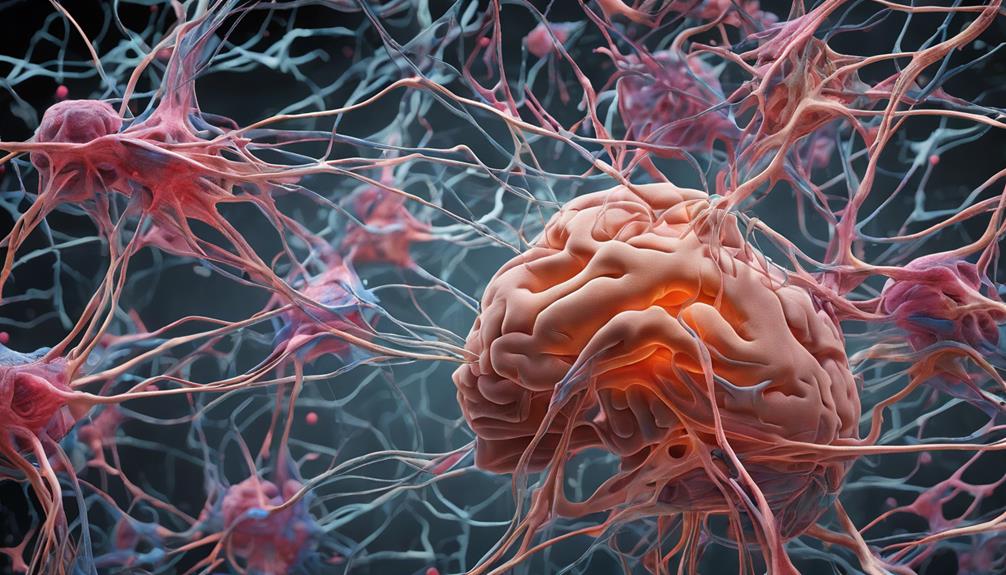
Protein Abnormalities in the Brain
Protein abnormalities in the brain, specifically the accumulation of abnormal proteins like tau and TDP-43, are key factors in the development of Frontotemporal Dementia (FTD). These abnormal proteins play a vital role in causing neuronal damage, leading to cell dysfunction and eventual death.
Here are some important points to understand about protein abnormalities in FTD:
- Neuronal damage in FTD occurs due to the buildup of abnormal proteins like tau and TDP-43.
- The presence of tau and TDP-43 proteins in the brain affects nerve cell communication and function, contributing to FTD pathology.
- Abnormal protein aggregation disrupts normal brain processes, resulting in the characteristic symptoms of FTD.
- Targeting protein abnormalities is essential for developing potential treatments to slow or prevent the progression of FTD.
- Understanding how abnormal proteins like tau and TDP-43 impact the brain is crucial in the study of FTD and potential therapeutic interventions.
Role of Tau in FTD
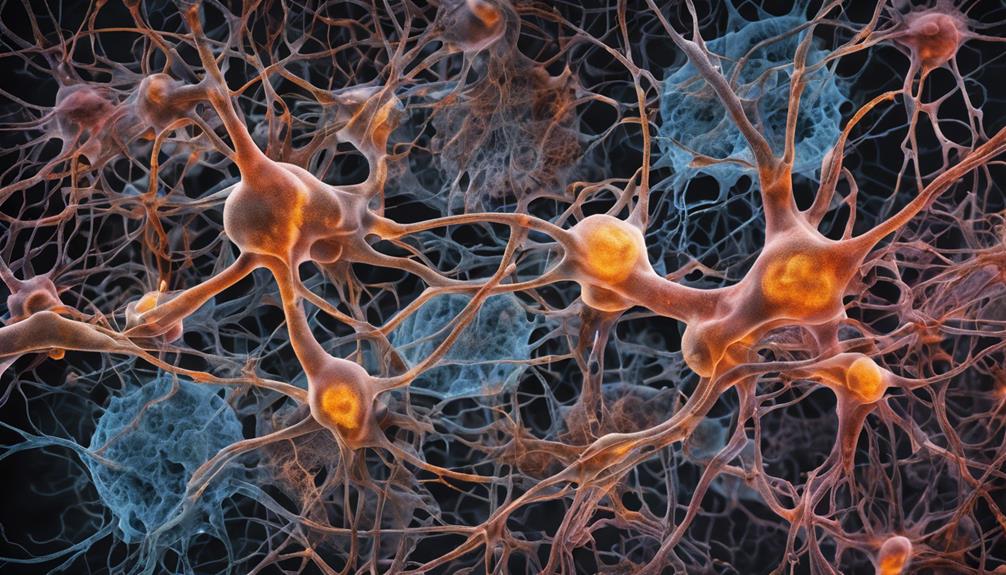
Understanding the pivotal role that tau protein plays in the development of Frontotemporal Dementia (FTD) is essential for unraveling the disease's pathophysiology.
Tau, a protein in the brain, forms tangles that contribute to nerve cell damage in FTD. These tangles disrupt normal cellular functions, leading to neurodegeneration seen in FTD.
Tau pathology is a key feature in specific FTD subtypes like progressive supranuclear palsy (PSP) and corticobasal degeneration (CBD). Abnormal tau in FTD can spread across the brain, impacting cognitive and motor functions as the disease advances.
Scientists are exploring tau-targeted therapies as potential treatments for FTD, aiming to address the underlying protein abnormalities. By studying tau's role in FTD, researchers hope to develop interventions that can target and potentially slow down the progression of this neurodegenerative disease.
Understanding tau's impact on the brain is vital for devising effective strategies to combat the devastating effects of FTD on individuals' cognitive and motor functions.
Role of TDP-43 in FTD
TDP-43 is an abnormal protein that we find in the brains of people with frontotemporal dementia. This protein is linked to causing damage to neurons in the brain.
In certain types of FTD, like semantic variant primary progressive aphasia, the accumulation of TDP-43 is a common feature.
TDP-43 Protein Function
Abnormal accumulation of TDP-43 protein in affected brain regions characterizes Frontotemporal Dementia (FTD). This protein plays an essential role in regulating gene expression and RNA processing within cells.
In FTD, dysfunction of TDP-43 leads to neuronal damage and cell death, contributing to the progression of the disease. TDP-43 pathology is a common feature in some FTD subtypes, impacting cellular functions and causing neurodegeneration.
Research indicates that abnormalities in TDP-43 are significant in understanding the disease mechanism, highlighting its role in the pathogenesis of FTD. Understanding the function of TDP-43 is essential in comprehending how FTD develops and progresses, providing valuable insights for potential treatments.
TDP-43 Mutations in FTD
In approximately 50% of Frontotemporal Dementia cases, mutations in the TDP-43 protein contribute significantly to the disease's progression. These mutations lead to neuronal dysfunction in the frontal and temporal lobes, where TDP-43 normally plays an essential role in RNA processing and regulation.
The abnormal accumulation of TDP-43 in neurons is a hallmark pathology of FTD, disrupting cellular functions essential for health. Research suggests that these mutations may trigger neurodegeneration and cognitive decline by interfering with RNA metabolism.
Understanding the impact of TDP-43 mutations in FTD is vital for developing targeted therapies that could potentially slow down or halt the progression of this devastating neurodegenerative disorder.
Impact of Family History

Considering the significant role family history plays in the development of frontotemporal dementia (FTD), understanding its impact is essential for evaluating genetic risks and providing appropriate care.
Family history can have a profound impact on the development of FTD, affecting the genetic mutations individuals may inherit.
Here are five key points to better grasp the impact of family history on FTD:
- Genetic mutations linked to FTD can be inherited from family members.
- Individuals with a family history of FTD have an increased risk of developing the disease.
- Genetic counseling is vital for evaluating risk factors and potential genetic mutations associated with FTD.
- Healthcare providers can use knowledge of family history to monitor individuals at higher risk for FTD development.
- Understanding the impact of family history allows for proactive measures in caring for those at risk of FTD.
Neuronal Death in FTD
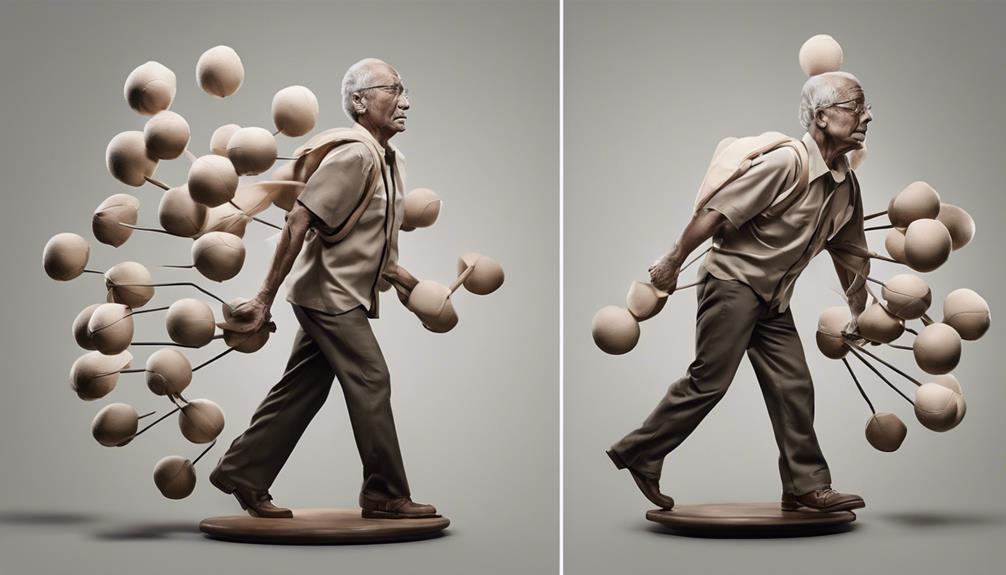
Understanding the mechanisms behind neuronal death in frontotemporal dementia is essential for developing targeted treatment strategies to combat the progression of the disease. In FTD, abnormal proteins like tau and TDP-43 accumulate in the frontal and temporal lobes, leading to the degeneration and eventual death of nerve cells.
This process disrupts normal cellular functions, communication between neurons, and impairs brain processes, resulting in cognitive and behavioral changes. The affected regions in the brain are pivotal for personality, behavior, language, and motor function, explaining the diverse symptoms seen in individuals with FTD.
Brain Damage in FTD

Brain damage in Frontotemporal Dementia (FTD) can take various forms, impacting vital brain regions responsible for behavior, personality, and language. This damage leads to atrophy, affecting cognitive functions like decision-making and language processing.
Neuronal loss in FTD is often accompanied by the accumulation of abnormal proteins, further exacerbating the brain damage and cognitive decline in individuals with this condition.
Types of Brain Damage
Damage to nerve cells in the frontal and temporal lobes characterizes Frontotemporal Dementia (FTD), with specific types of brain damage involving the accumulation of abnormal proteins. Understanding these types of brain damage is essential for managing FTD effectively.
Here are five key points to help you grasp the impact of brain damage in FTD:
- FTD is associated with atrophy and damage to nerve cells in the frontal and temporal lobes.
- Abnormal proteins like tau and TDP-43 accumulate in the brain, leading to neuronal loss and dysfunction.
- Frontal lobe damage in FTD results in noticeable behavioral changes.
- Damage to the temporal lobe affects language skills and emotional processing.
- Brain imaging techniques like MRI scans can reveal the extent of brain damage in individuals with Frontotemporal Dementia.
Impact on Cognitive Functions
FTD's impact on cognitive functions becomes evident through the atrophy and damage to nerve cells in the frontal and temporal lobes, affecting decision-making, problem-solving, and social behavior. Executive functions like planning and organizing may also be compromised. Changes in memory, language, and emotional responses are commonly observed in individuals with Frontotemporal Dementia.
These alterations in brain structure lead to challenges in reasoning, judgment, and social interactions. Understanding these cognitive deficits is vital for providing appropriate support and care for those affected by FTD. By recognizing the specific areas of cognitive decline, such as the frontal lobes' role in decision-making and the temporal lobes' influence on memory, interventions can be tailored to enhance the quality of life for individuals facing these challenges.
Neuronal Loss in FTD
Neuronal loss in Frontotemporal Dementia primarily targets the frontal and temporal lobes, resulting in significant damage within these brain regions.
- Damage to neurons in FTD occurs due to abnormal proteins like tau and TDP-43.
- Atrophy and shrinkage of brain tissue in the frontal and temporal lobes are common in FTD.
- This neuronal loss disrupts normal brain function, affecting behavior, language, and motor skills.
- Understanding neuronal loss in FTD is essential for diagnosing and managing the condition.
- Cognitive and behavioral changes in FTD stem from the damage to neurons in the frontal and temporal lobes.
Environmental Influences on FTD

Exposure to certain toxins or chemicals may contribute to the development of Frontotemporal Dementia (FTD), according to research findings. Additionally, head trauma or traumatic brain injuries could potentially increase the risk of developing FTD later in life. Chronic stress, resulting from prolonged exposure to stressful situations, may also play a role in the development or progression of FTD.
Moreover, lifestyle factors like diet, exercise, and sleep patterns could influence the risk of FTD, although limited research exists in this area. It's essential to understand that further research is needed to fully grasp the impact of environmental influences on the onset and progression of Frontotemporal Dementia.
It's vital to be mindful of our surroundings, avoid harmful chemicals or toxins, protect our heads from injury, manage stress levels, and maintain a healthy lifestyle through proper diet, regular exercise, and adequate sleep to potentially reduce the risk of developing FTD.
Frequently Asked Questions
Can FTD Be Prevented?
Yes, we can take steps to potentially reduce the risk of Frontotemporal Dementia (FTD) through a healthy lifestyle. While prevention is challenging due to complex causes, choices like exercise, diet, and mental stimulation may help.
Is Frontotemporal Dementia Caused by Trauma?
No, frontotemporal dementia is not directly caused by trauma. However, in some cases, traumatic brain injuries can potentially trigger or worsen its development, particularly in individuals with genetic predispositions. Understanding this relationship is essential.
What Is the Average Age of Onset of Frontotemporal Dementia?
Oh, the joys of discovering that Frontotemporal Dementia typically starts showing its colors between 40 and 65 years. Both men and women face this equally. Seeking medical care for those symptoms is essential.
How Long Can a Person Live With Ftd?
We recognize the concern about life expectancy with FTD. The duration varies, influenced by individual factors. Supportive care and early intervention can enhance quality of life and potentially extend survival. It's important to address these aspects for better outcomes.
Conclusion
To sum up, the reasons behind frontotemporal dementia (FTD) are intricate and multifaceted, involving: a complex interplay of genetic, environmental, and molecular factors. Research has shown that certain gene mutations, such as those affecting the tau protein, play a significant role in FTD development, while other cases remain sporadic with unclear origins. Additionally, overlaps with other neurodegenerative conditions, including the stages of Parkinson’s disease, have been observed, further complicating diagnosis and treatment strategies. Emerging studies suggest that the shared characteristics between FTD and other diseases, such as Parkinson’s, might offer insight into common pathways of neurodegeneration. Efforts to better understand these connections, as seen in the detailed analysis of neurodegenerative progression like in *parkinson’s disease stages explained*, could lead to improved diagnostic tools and potential therapeutic targets. As research advances, the hope is to uncover more precise methods to differentiate and treat these conditions effectively.
- Genetic factors
- Protein abnormalities in the brain
- Family history
- Neuronal death
- Brain damage
- Environmental influences
While research is ongoing to uncover the exact mechanisms behind FTD, it's evident that a combination of genetic predisposition and environmental factors play a significant role in the development of this condition.
Understanding these causes is essential for early detection and potential future treatments.