Picture a scenario where a patient presents with severe pain and swelling in their knee, resulting in a diagnosis of septic arthritis. Despite our familiarity with this condition, accurately coding it according to ICD-10 guidelines can occasionally be overlooked.
Understanding the nuances of coding for septic arthritis is crucial not only for accurate documentation but also for ensuring proper reimbursement and effective tracking of cases.
Let's explore further how precise ICD-10 coding plays a vital role in managing and treating septic arthritis cases.
Key Takeaways
- Specific ICD-10 codes pinpoint infection location and bacteria responsible.
- Mastery of joint infection codes aids in targeted treatment and diagnosis.
- Accurate documentation crucial for billing, treatment precision, and communication.
- Proper identification with ICD-10 codes enhances reimbursement, clinical management, and outcomes.
Overview of Septic Arthritis ICD-10 Codes
When categorizing cases of septic arthritis, healthcare providers rely on a range of ICD-10-CM codes from M00.0 to M00.9 to specify the affected joint and underlying cause.
The use of specific ICD-10 codes for septic arthritis, such as M00.86 for the knee and M00.80 for an unspecified site, is crucial in differentiating between cases and ensuring accurate diagnosis and reimbursement. These codes not only help in pinpointing the exact location of the infection but also aid in identifying the specific bacteria responsible for the condition.
Understanding septic arthritis ICD-10 codes is essential for proper documentation and tracking of bacterial joint infections. By utilizing these codes, healthcare professionals can effectively classify septic arthritis based on the affected joints and the etiology, enabling streamlined tracking of cases and facilitating appropriate treatment protocols.
Proper utilization of septic arthritis ICD-10 codes enhances the overall management of the condition and ensures optimal patient care.
Specific ICD-10 Codes for Joint Infections
To accurately classify joint infections caused by various bacteria, specific ICD-10 codes are utilized. These codes, such as M00.80, M00.829, M00.849, M00.869, and M00.9, play a crucial role in distinguishing between different arthropathies due to bacterial arthritis.
By assigning these specific codes, healthcare providers can convey detailed diagnostic information regarding the type of joint infections present in a patient. Additionally, utilizing additional codes like B96 becomes essential to identify the specific microbiological agents responsible for the septic arthritis, aiding in targeted treatment strategies.
Understanding the nuances of these codes is pivotal for accurate documentation and proper reimbursement processes. Proper classification through these codes not only helps in the effective management of musculoskeletal conditions but also ensures appropriate tracking of joint infections for ongoing care.
Mastering the use of these specific ICD-10 codes is instrumental in providing quality care for patients with bacterial joint infections.
Understanding Coding for Septic Arthritis
Proper documentation of septic arthritis cases is crucial to accurately differentiate between bacterial causes and ensure precise identification for targeted treatment. In ICD-10 coding, septic arthritis falls under specific categories like M00.80, M00.829, M00.849, M00.869, and M00.9.
Understanding the intricacies of ICD-10 coding is essential for accurate billing and effective treatment of septic arthritis within the musculoskeletal system. Additional codes such as B96 are utilized to specify the bacterial cause, aiding in precise identification of the affected joint and the specific bacterial pathogen involved.
This detailed documentation is fundamental not only for billing purposes but also for providing the necessary information for appropriate medical intervention. By following the guidelines set by ICD-10 and ensuring meticulous documentation, healthcare providers can navigate the complexities of coding for septic arthritis efficiently, leading to improved patient care and outcomes.
Importance of Accurate ICD-10 Documentation
Effective ICD-10 documentation plays a critical role in accurately identifying and managing septic arthritis cases. Proper identification through specific ICD-10 codes is essential for appropriate reimbursement, ensuring that healthcare providers are compensated fairly for treating septic arthritis. Detailed documentation in medical records and billing using codes like M00.849 for bacterial infections in the hand is crucial for tracking the prevalence and outcomes of septic arthritis cases. This information is vital for effective healthcare management, allowing for informed decisions and resource allocation. Additionally, understanding the nuances of ICD-10 documentation enhances clinical communication among healthcare professionals, facilitating better coordination in the diagnosis and treatment of septic arthritis cases. Ensuring accurate and comprehensive documentation not only benefits individual patient care but also contributes to broader research efforts aimed at improving outcomes for individuals affected by septic arthritis.
| Importance of Accurate ICD-10 Documentation | ||
|---|---|---|
| Proper Identification | Reimbursement | Specific ICD-10 Codes |
| Bacterial Infections | Medical Records | Billing |
| Healthcare Management | Clinical Communication |
Managing Septic Arthritis Cases With ICD-10
Managing septic arthritis cases with ICD-10 involves precise classification and detailed documentation to ensure accurate diagnosis and appropriate treatment. Healthcare providers must utilize specific ICD-10-CM diagnosis codes such as M00.84 for hand arthritis, M00.80 for other bacterial arthritis, and M00.869 for knee arthritis when coding septic arthritis cases. Proper coding is essential for reimbursement and tracking purposes, enabling healthcare facilities to accurately record and monitor these cases.
In conjunction with ICD-10-CM codes, additional codes like B96 help specify the bacterial cause of septic arthritis, aiding in targeted treatment strategies. Understanding the nuances of ICD-10-CM coding is crucial for healthcare providers to effectively manage septic arthritis cases. These codes provide detailed information on the site of infection, facilitating precise diagnosis and ongoing monitoring.
Frequently Asked Questions
What Is the ICD-10 Code for Septic Arthritis?
We can provide the correct ICD-10 code for septic arthritis, which is crucial for accurate diagnosis and treatment. In this case, the ICD-10 code is M00.9, specifically for infective arthritis not otherwise specified.
Proper coding is essential to ensure effective reimbursement and manage infectious joint conditions efficiently. Understanding the nuances of coding for septic arthritis aids in tracking and addressing joint infections promptly.
What Is Septic Arthritis?
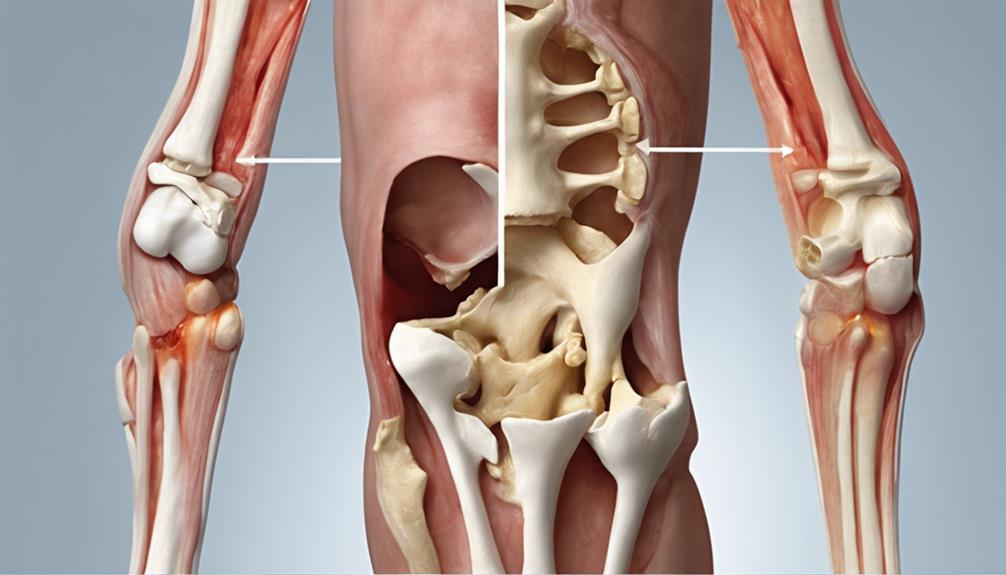
When bacteria, viruses, or fungi infect a joint, it leads to septic arthritis, a serious condition characterized by joint pain, swelling, warmth, and limited range of motion.
Timely diagnosis and treatment are crucial to prevent joint damage and other complications. Risk factors include prior joint issues, recent surgery, and a weakened immune system.
While septic arthritis can affect any joint, it commonly targets the knee, hip, shoulder, and elbow joints.
What Is the ICD-10 Code for Septic Prosthetic Arthritis?
We've got the answer you're looking for!
The ICD-10 code for septic prosthetic arthritis is T84.59X1A.
This specific code is used to indicate an infection in a prosthetic joint post-implantation.
The 'X' in the code pinpoints the location of the infection in the body, while the 'A' at the end signifies that it's the initial encounter for treatment.
What Is the ICD-10 Code for M00.9?
We use the ICD-10 code M00.9 to classify cases of unspecified pyogenic or pyemic arthritis. This code falls under infectious arthropathies and covers infective arthritis not otherwise specified. It encompasses various joints like the hip, knee, shoulder, and metatarsophalangeal.
Correctly applying M00.9 is vital for accurately diagnosing and ensuring proper reimbursement for septic arthritis cases. Understanding this code is essential for effective medical coding and billing processes.
Conclusion
In the intricate web of medical coding, accurate documentation of septic arthritis cases is crucial for effective treatment and reimbursement.
Like a skilled detective piecing together clues, healthcare professionals must utilize specific ICD-10 codes to identify the culprit bacteria causing joint infections.
Precision in coding is the key to unlocking the door to successful management of septic arthritis cases. Just as every piece fits perfectly in a puzzle, every code must align for optimal patient care.