Did you know that veterans who developed Ischemic Heart Disease as a result of being exposed to Agent Orange may be eligible for an average disability compensation from the VA?
The compensation amount varies based on factors such as the severity of the condition and the impact on daily life.
Understanding how these payments are determined can provide valuable insight for veterans navigating the process of applying for disability benefits.
It's essential to explore the intricacies of the compensation system to ensure veterans receive the support they rightfully deserve.
Key Takeaways
- Average payment from settlement fund: $3,800 per affected individual.
- Single veterans eligible for up to $39,984 per year in disability benefits.
- Cash payments from fund ceased in 1994 affecting average compensation.
- Compensation amounts vary based on severity, disability rating, and individual circumstances.
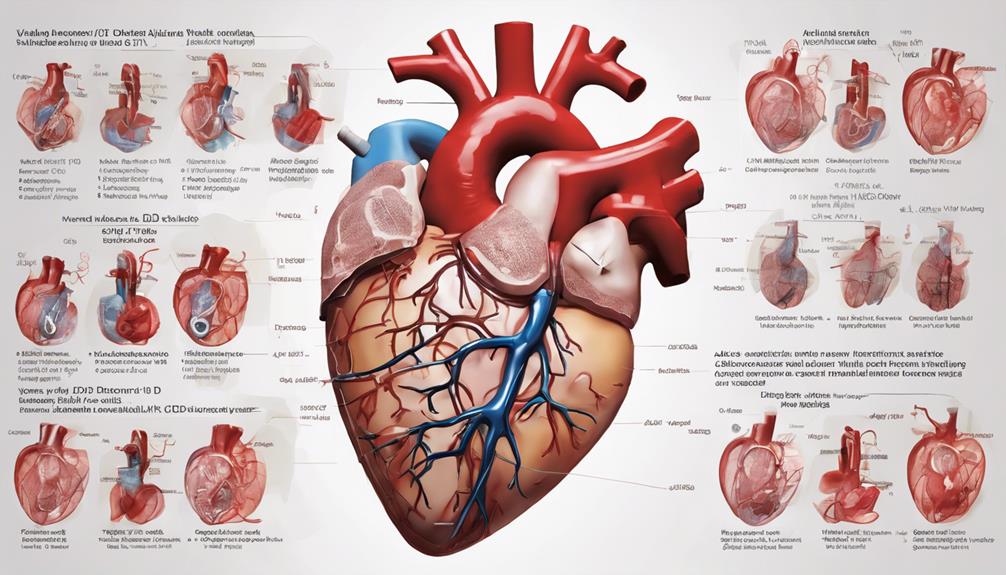
Agent Orange and Ischemic Heart Disease
Exposure to Agent Orange is a known risk factor for developing ischemic heart disease among veterans. Veterans with ischemic heart disease linked to Agent Orange exposure may qualify for VA disability benefits through presumptive service connection. Disability ratings for ischemic heart disease can range from 10% to 100%, determined by the severity of symptoms and functional limitations.
Those affected could receive up to $39,984 per year in disability compensation for ischemic heart disease related to Agent Orange exposure. In cases where veterans undergo heart surgeries like transplants or pacemaker implantations, temporary 100% disability ratings for ischemic heart disease may be granted.
Navigating the complexities of filing disability claims for ischemic heart disease tied to Agent Orange exposure can be challenging. Seeking expert legal assistance, such as that provided by Berry Law, can greatly aid veterans in understanding their eligibility for VA disability benefits and in maximizing their potential compensation.
Eligibility for Disability Benefits

To qualify for disability benefits related to ischemic heart disease associated with Agent Orange exposure, specific criteria and evidence must be presented to establish eligibility. Veterans seeking VA disability benefits for ischemic heart disease should consider the following:
- Disability Ratings: Disability ratings for ischemic heart disease can range from 10% to 100% based on the severity of symptoms and how they impact daily life.
- Evidence: It's crucial to provide medical evidence linking the ischemic heart disease to Agent Orange exposure. This evidence can include medical records, test results, and statements from healthcare providers.
- Veterans Law Attorneys: Seeking assistance from experienced Veterans law attorneys can be beneficial in navigating the complex VA disability benefits process. These professionals can provide guidance on gathering the necessary evidence, completing paperwork accurately, and advocating for the best possible outcome for veterans with ischemic heart disease linked to Agent Orange exposure.
Average Compensation Amounts
Veterans seeking disability benefits related to ischemic heart disease associated with Agent Orange exposure may receive varying compensation amounts influenced by factors such as disability rating and dependents. The average payment from the Agent Orange settlement fund stood at $3,800 per affected individual. However, cash payments from the fund ceased in 1994, impacting the average compensation received by veterans.
Single veterans affected by Agent Orange exposure could be eligible for up to $39,984 per year in disability benefits, with actual amounts varying based on individual circumstances and severity of the condition. Specifically, for veterans with ischemic heart disease linked to Agent Orange exposure, the average disability compensation amount is shaped by specific factors like disability rating and the presence of dependents.
It's crucial for affected individuals to understand how these elements influence the average compensation amounts they may receive to better prepare for the financial support they're entitled to under the disability benefits system.
Applying for Disability Benefits
When seeking disability benefits for ischemic heart disease linked to Agent Orange, applicants have multiple avenues for application submission. Here are some key steps to apply for disability benefits for ischemic heart disease:
- Online Application: Veterans can conveniently apply for disability benefits online through the VA's website. This method allows for a streamlined process and easy submission of required documents.
- In-Person Application: For those who prefer face-to-face assistance, visiting a local VA office can be beneficial. Veterans can receive personalized help from VA representatives to ensure a smooth application process.
- Assistance from Veterans Law Attorneys: Seeking guidance from experienced Veterans law attorneys, such as those at Berry Law, can greatly assist veterans in navigating the complexities of the application process. These professionals can provide valuable expertise and support to help veterans secure the disability benefits they deserve.
VA Disability Ratings
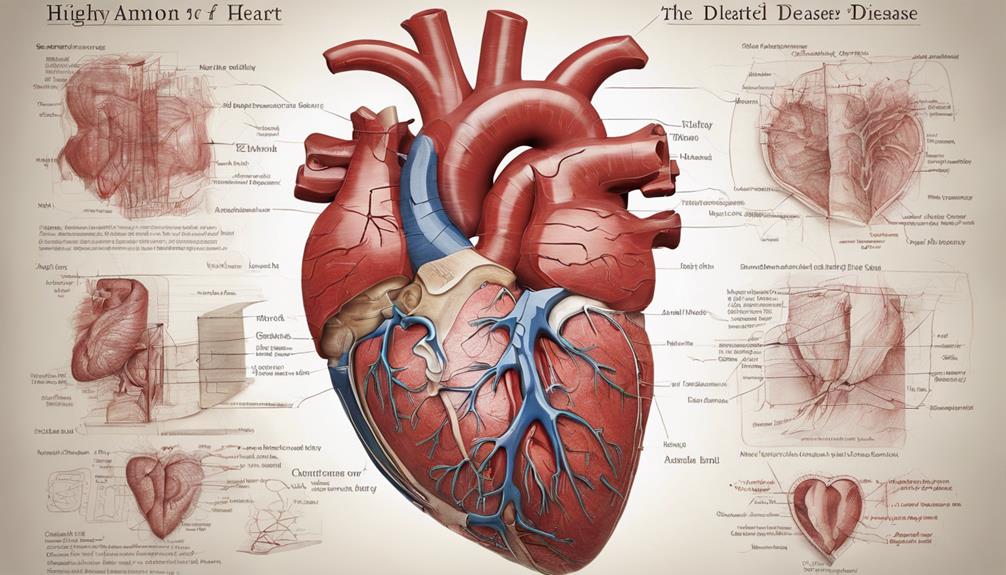
In evaluating disabilities related to ischemic heart disease, the VA employs specific criteria to assign disability ratings based on symptom severity and other relevant factors. Ischemic heart disease is rated at 10%, 30%, 60%, or 100% based on the severity of symptoms as outlined in Diagnostic Code 7005 of the VA Schedule of Ratings.
Factors such as heart workload METs, symptoms like breathlessness and fatigue, and the impact of treatments are carefully considered in determining the disability rating. In cases where individuals undergo heart surgeries such as transplants, temporary 100% disability ratings may be warranted.
It's crucial for individuals with ischemic heart disease, especially those exposed to Agent Orange, to understand how these disability ratings are calculated as they can have a significant impact on the benefits they receive. By closely monitoring symptoms and seeking appropriate medical care, individuals can ensure they receive the disability rating that accurately reflects the impact of their condition.
Frequently Asked Questions
What Is the VA Disability Rate for Ischemic Heart Disease?
We determine the VA disability rate for Ischemic Heart Disease based on the severity of symptoms, which can range from 10% to 100%. Factors like heart workload METs, heart failure symptoms, and ejection fraction play a key role in this assessment.
METs levels are crucial, with over 6.0 indicating vigorous activities and under 3.0 suggesting sedentary behavior. Veterans who undergo heart surgeries may receive temporary 100% disability ratings.
Symptoms such as breathlessness, fatigue, and arrhythmia are carefully considered in determining the disability rating.
What Is the Average Compensation for Agent Orange?
Sure thing!
When it comes to the average compensation for Agent Orange exposure, our veterans saw payments that averaged around $3,800.
Back in the day, single veterans could receive up to $39,984 per year in disability benefits.
These payments aimed to address the health impacts of Agent Orange exposure on our beloved veterans.
It's crucial to recognize and support those who've sacrificed for our country's well-being.
What Are the Secondary Conditions of Ischemic Heart Disease?
Secondary conditions of ischemic heart disease include heart failure, arrhythmias, angina pectoris, myocardial infarction, sudden cardiac death, peripheral artery disease, stroke, chronic kidney disease, anxiety, depression, and post-traumatic stress disorder.
Individuals with ischemic heart disease may also experience fatigue, shortness of breath, and chest pain.
These secondary conditions can significantly impact one's quality of life and overall health, requiring proper management and care.
Is Ischemic Heart Disease a Permanent Disability?
Yes, ischemic heart disease can indeed be a permanent disability. The severity of the condition plays a vital role in determining disability benefits for veterans.
Some may even qualify for a 100% disability rating based on the impact of the disease. These benefits provide crucial ongoing financial support for veterans facing severe cases of ischemic heart disease.
It's a significant aspect of our commitment to supporting those who've served.
Conclusion
In conclusion, veterans exposed to Agent Orange may be eligible for disability benefits due to ischemic heart disease.
On average, the compensation amount for this condition is $2,000 to $4,000 per month.
It's important for veterans to apply for VA disability benefits and receive proper ratings based on the severity of their symptoms.
This assistance can greatly help improve their quality of life and access to necessary medical treatments.