When exploring the complex realm of pediatric cardiology, it is important to recognize the critical significance of Ductal Dependent Congenital Heart Disease.
The complexities surrounding this condition extend far beyond its initial presentation, prompting a closer examination that uncovers a cascade of considerations.
As we explore the nuances of this critical topic, we find ourselves drawn into a realm where early identification and strategic management hold the key to unfolding a path towards improved patient outcomes.
Key Takeaways
- Prompt recognition of symptoms crucial for neonates with ductal dependent CHD.
- Echocardiography essential for confirming duct-dependent circulation in newborns.
- PGE1 infusion vital to maintain ductal patency and stabilize neonates.
- Timely surgical interventions may be necessary to support heart function in neonates.
Understanding Ductal Dependent Congenital Heart Disease
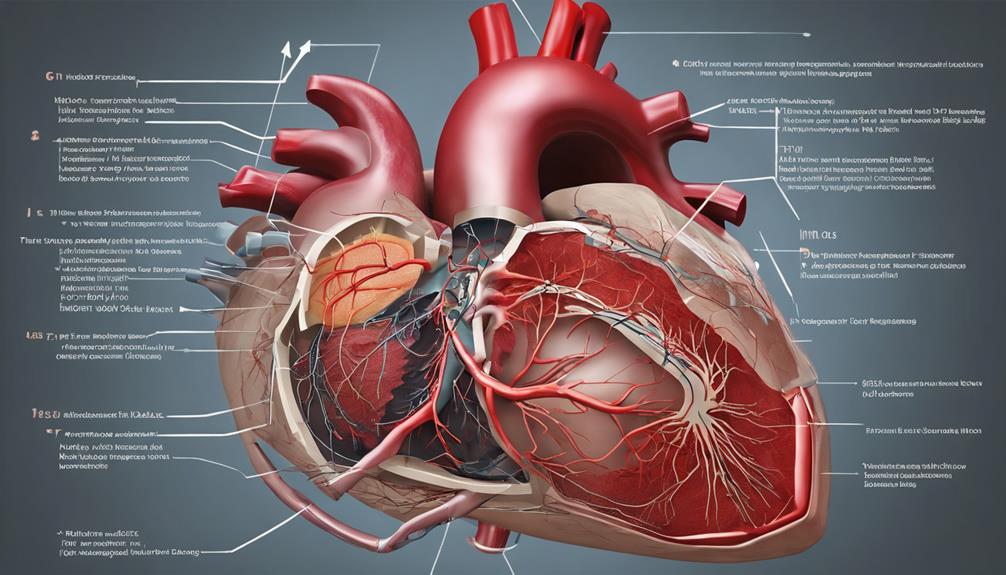
In neonates with ductal dependent congenital heart disease, the patent ductus arteriosus (PDA) serves a critical function in maintaining systemic or pulmonary blood flow. When this vital connection fails to close appropriately after birth, it can lead to significant issues such as severe cyanosis, respiratory distress, and compromised systemic circulation.
In such cases, immediate intervention becomes necessary to sustain the neonate's life. Diagnosis of ductal dependent CHD involves evaluating oxygen saturation levels and clinical presentation, prompting swift action to initiate PGE1 infusion therapy. The management of these fragile patients revolves around ensuring ductal patency through pharmacological means while closely monitoring for any potential complications.
Timeliness in diagnosing and treating ductal dependent CHD is paramount in preventing adverse outcomes and optimizing the neonate's chances of survival. By prioritizing diligent monitoring of oxygen saturation, response to PGE1 infusion, and overall clinical status, healthcare providers can offer these neonates the best possible care during this critical period.
Causes and Risk Factors
What're the primary causes and risk factors associated with ductal-dependent congenital heart disease (CHD)? Ductal-dependent CHD is often linked to specific structural heart defects that necessitate the patency of the ductus arteriosus for adequate circulation postnatally.
Some risk factors and causes include:
- Structural Heart Defects: Conditions such as transposition of the great arteries and hypoplastic left heart syndrome are examples of structural heart defects that require the ductus arteriosus to be open to ensure proper oxygenation.
- Premature Closure: Premature closure of the ductus arteriosus can result in critical circulatory issues in neonates with ductal-dependent CHD, impacting their overall health and wellbeing.
- Management in Infants: Timely recognition and appropriate management of ductal-dependent CHD are crucial in infants to prevent severe complications and optimize outcomes. This involves close monitoring and potentially surgical interventions to maintain adequate circulation and support the infant's heart function.
Recognizing Symptoms in Newborns
Recognizing symptoms in newborns with ductal-dependent congenital heart disease requires keen observation and prompt action to ensure timely intervention and proper management. In the neonatal period, infants with ductal dependent lesions may exhibit severe cyanosis, respiratory distress, shock, or collapse. It's crucial to promptly recognize signs such as poor perfusion, tachypnea, and poor feeding, as they indicate potential cardiac issues. Utilizing diagnostic tools like echocardiography and oxygen saturation monitoring aids in confirming the presence of duct-dependent circulation and guides treatment decisions.
When assessing newborns for suspected ductal dependent lesions, distinguishing between cardiac and pulmonary causes of cyanosis is essential for initiating appropriate management strategies. Immediate medical attention is paramount, and initiating prostaglandin infusion can be life-saving in stabilizing these neonates. By closely monitoring for symptoms of respiratory distress, poor perfusion, and shock, healthcare providers can swiftly intervene and optimize outcomes for newborns with ductal-dependent congenital heart disease.
Diagnostic Procedures and Tests

Utilizing advanced diagnostic tools is crucial in accurately assessing and managing ductal dependent congenital heart disease. The following diagnostic procedures and tests play a vital role in the evaluation of patients with ductal dependent lesions and neonatal heart defects:
- Echocardiography: This imaging technique allows for detailed visualization of the heart's structure and function, providing essential information for diagnosing and monitoring ductal dependent congenital heart disease.
- Doppler studies: By assessing the direction and velocity of blood flow within the heart and blood vessels, Doppler studies help determine the severity and impact of ductal dependent lesions on circulation.
- Cardiac catheterization: This invasive procedure aids in obtaining precise hemodynamic measurements and anatomical details of the heart, guiding treatment decisions for patients with complex ductal dependent lesions.
These diagnostic tools, along with other modalities like MRI, pulse oximetry, and ECG, contribute to a comprehensive assessment of patients with ductal dependent congenital heart disease, enabling healthcare providers to deliver optimal care based on accurate and detailed information.
Treatment Options and Interventions
Implementing targeted therapeutic strategies is essential in managing neonates with ductus-dependent congenital heart disease to ensure optimal outcomes and hemodynamic stability. PGE1 infusion serves as a cornerstone in treatment, maintaining ductal patency crucial for neonates with this condition.
Monitoring oxygen saturation and pressure post-PGE1 administration is imperative to assess treatment effectiveness and optimize oxygenation levels. Complications such as fever, leukocytosis, edema, and potential side effects like apnea and convulsions may arise during PGE1 therapy, necessitating careful monitoring and intervention.
Gradual weaning off PGE1 once optimal oxygenation levels are achieved is recommended to minimize side effects and complications. Echocardiography plays a pivotal role in monitoring the effect of PGE1 on ductus arteriosus patency, guiding treatment adjustments in neonates with critical congenital heart disease.
Regular monitoring, prompt recognition of complications, and appropriate treatment adjustments are essential components in the comprehensive care of neonates with ductus-dependent congenital heart disease.
Frequently Asked Questions
What Drug Is Used for Duct Dependent Congenital Heart Disease?
We use Prostaglandin E1 (PGE1) to manage duct-dependent congenital heart disease in neonates. PGE1 helps keep the ductus arteriosus open, crucial for circulation in certain heart defects.
Its infusion stabilizes infants with severe cyanosis or shock. Accurate dosing and monitoring are essential for optimizing oxygenation and hemodynamic stability.
Early detection of duct-dependent CHD and prompt PGE1 therapy initiation significantly impact outcomes in affected newborns.
What Does Ductal Dependent Mean?
Ductal dependent refers to a condition where a specific blood vessel called the ductus arteriosus is vital for proper blood flow in the body. This dependency means that the ductus arteriosus must remain open to ensure adequate circulation.
Failure to keep it open can result in serious complications like low oxygen levels, shock, or organ damage.
Managing ductal dependent conditions promptly is essential for the well-being and survival of affected individuals.
Is Tetralogy of Fallot Ductal Dependent?
Yes, Tetralogy of Fallot isn't ductal dependent. It doesn't rely on a patent ductus arteriosus (PDA) for proper oxygenation. Blood flow to the lungs and body in Tetralogy of Fallot is maintained independently of a PDA.
Corrective surgeries are often necessary to address the structural issues in this condition. Understanding this non-ductal dependency is vital for accurate diagnosis and treatment planning in affected individuals.
What Is the Life Expectancy for a Child With Congenital Heart Defect?
When it comes to the life expectancy of a child with a congenital heart defect, various factors come into play. These include the specific type and severity of the defect, timely diagnosis, access to specialized care, and overall health status.
Advances in medical technology and surgical interventions have significantly improved outcomes and increased life expectancy for many children with these conditions. Proper management, early detection, appropriate interventions, and comprehensive care are crucial for maximizing life expectancy and quality of life.
Conclusion
In conclusion, navigating the intricate pathways of ductal dependent congenital heart disease requires swift action and precise interventions. Like skilled conductors orchestrating a symphony, healthcare providers must harmonize the delicate balance of blood flow in these vulnerable newborns.
With early recognition and targeted treatments, we can guide these tiny hearts towards optimal outcomes, ensuring a melody of health and vitality for their future.