Heart Disease Management
What Causes Microvascular Heart Disease?
Heralding a new era in cardiovascular care, microvascular heart disease unveils hidden complexities with profound implications.
When navigating the intricate network of blood vessels in the heart, it is important to consider the impact of microvascular heart disease. This lesser-known condition presents unique challenges that are different from those seen in traditional coronary artery disease.
As we navigate through the complexities of this ailment, it becomes evident that understanding its subtle nuances is crucial for effective management.
Let's uncover the intricacies of microvascular heart disease and shed light on the latest advancements in diagnosis and treatment that are shaping the landscape of cardiovascular health.
Key Takeaways
- Critical for women, diabetics, and those with high blood pressure
- Symptoms include chest pain, fatigue, and shortness of breath
- Specialized tests like CFR and cardiac MRI essential for accurate diagnosis
- Lifestyle changes, medication, and regular monitoring key for treatment and prevention
Overview of Microvascular Heart Disease
Microvascular heart disease, also referred to as coronary microvascular disease or microvascular endothelial dysfunction, impacts the microscopic blood vessels within the heart, resulting in compromised blood flow and potential complications. This condition specifically affects the small vessels of the heart, which play a crucial role in supplying oxygen and nutrients to the heart muscle. Microvascular heart disease is a significant concern in healthcare, especially for women, diabetics, and individuals with high blood pressure, as they're more prone to developing this condition. Small vessel disease not only affects the heart but can also have broader implications, such as contributing to cognitive decline and increasing the risk of strokes.
Recognizing the symptoms of microvascular heart disease is vital for timely intervention. Patients may experience chest pain, shortness of breath, fatigue, and discomfort in various areas like the left arm, jaw, neck, back, or abdomen. Understanding these signs can aid healthcare providers in offering appropriate care and management strategies tailored to each individual's needs.
Causes and Symptoms
Moving from understanding the overview of microvascular heart disease, it's essential to delve into the specific causes and symptoms associated with this condition to facilitate accurate diagnosis and effective management strategies. Small vessel dysfunction in the coronary microvascular system can lead to a condition known as coronary microvascular disease. This dysfunction affects the flow of blood through the small arteries of the heart, resulting in symptoms that may be challenging to differentiate from other heart conditions.
- Causes of Microvascular Heart Disease:
- Diabetes
- High blood pressure
- High cholesterol
- Obesity
- Autoimmune diseases
- Symptoms of Microvascular Heart Disease:
- Angina lasting over 10 minutes
- Worsening chest pain with stress or exertion
- Fatigue
- Shortness of breath
- Sleep disturbances
Understanding these causes and symptoms is vital in helping individuals recognize the signs of non-obstructive coronary artery disease and seek appropriate medical help promptly to prevent complications.
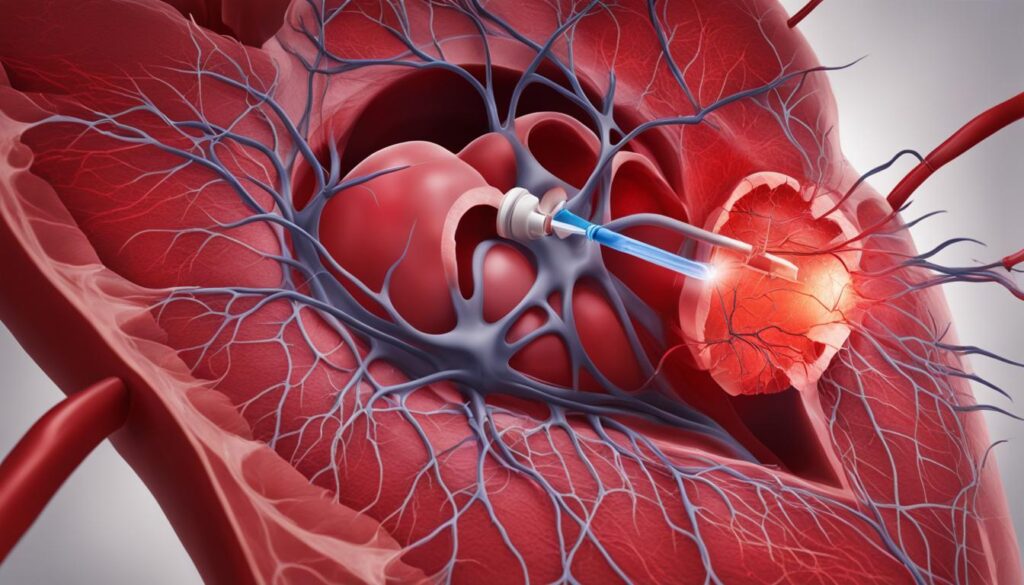
Diagnosis and Testing
Diagnosis and testing for microvascular heart disease necessitate specialized cardiac assessments to evaluate small vessel function accurately. Utilizing diagnostic tools such as coronary flow reserve (CFR) during cardiac catheterization provides valuable insights into small vessel disease.
Additionally, nuclear cardiac stress tests and cardiac MRI with perfusion play crucial roles in assessing microvascular health. Expert interpretation of these results by a cardiologist specializing in small vessel disease is essential for an accurate diagnosis and effective treatment planning.
The intricate nature of microvessels underscores the importance of specific imaging methods to aid in diagnosis. Timely and precise evaluation through comprehensive testing is paramount for managing microvascular heart disease and enhancing outcomes.
Treatment Options
Exploring various treatment options is crucial for effectively managing microvascular heart disease and improving patient outcomes. When addressing this condition, a multidimensional approach is often necessary. Here are some key components of the treatment plan:
- Prescription Medications: These can be used to help open small blood vessels, improve coronary blood flow, and alleviate chest pain associated with microvascular heart disease.
- Lifestyle Modifications: Making lifestyle changes such as adopting a healthier diet and incorporating stress reduction techniques can play a significant role in managing symptoms and preventing further complications.
- Exercise Counseling: Recommendations for exercise tailored to individual needs can aid in symptom management and overall health improvement.
- Behavioral Support: Working with behavioral psychologists and specialists can assist in implementing lifestyle modifications and coping strategies to deal with the challenges of the condition.
- Regular Check-ins: Scheduled check-ins with healthcare providers are essential for monitoring progress, adjusting treatment plans as needed, and ensuring the effective management of microvascular heart disease.
Prevention and Outlook
Implementing lifestyle modifications and monitoring key risk factors are crucial steps in preventing microvascular heart disease and improving long-term outcomes. Lifestyle changes such as engaging in regular physical activity and following a heart-healthy diet can play a significant role in lowering the risk of developing microvascular heart disease. Additionally, keeping a close check on high blood pressure, high cholesterol levels, and managing diabetes through proper monitoring are essential in preventing the progression of this condition. Early intervention by healthcare professionals, along with regular medical screenings, can help identify any emerging risk factors promptly, allowing for timely management and prevention of complications. Smoking cessation and stress management techniques are also vital components in the prevention and control of microvascular heart disease. By adopting these preventive measures and addressing risk factors proactively, individuals can enhance their overall outlook, leading to an improved quality of life and reduced risk of adverse outcomes.
| Prevention | Risk Factors | Early Intervention |
|---|---|---|
| Lifestyle modifications | High blood pressure | Regular medical check-ups |
| Monitoring | High cholesterol | Timely management |
| Smoking cessation | Diabetes | Healthcare screenings |
Frequently Asked Questions
How Do You Treat Microvascular Disease in the Heart?
When treating heart disease, we tailor medication regimens to improve blood vessel function and reduce complications. Common medications include ACE inhibitors, anticoagulants, beta-blockers, calcium channel blockers, diuretics, and statins.
Specialized centers like Cleveland Clinic can provide personalized treatment plans. Effective management enhances symptom control and quality of life.
Regular follow-up care is crucial for monitoring treatment effectiveness and adjusting the plan as needed.
Can You Live Normal Life With Microvascular Angina?
Yes, we can live a normal life with microvascular angina. Proper management, including lifestyle adjustments, medication adherence, and regular medical follow-ups, can effectively control symptoms and enhance our quality of life.
Identifying triggers, managing risk factors, engaging in cardiac rehab programs, and following prescribed treatments are crucial steps for symptom relief and preventing complications.
With the right care and support, individuals can maintain an active and fulfilling lifestyle despite microvascular angina.
What Does Microvascular Angina Feel Like?
We feel microvascular angina as persistent chest pain triggered by stress or exertion. Symptoms include chest pressure, tightness, burning, or squeezing, often radiating to the neck, jaw, back, or arms.
Unlike traditional angina, it stems from small heart vessel dysfunction. People may also experience fatigue, shortness of breath, and sleep disturbances alongside chest pain. Accurate diagnosis via specialized tests is crucial to differentiate microvascular angina from other heart conditions and guide treatment.
What Are the New Treatments for Coronary Microvascular Disease?
We explore new treatments for coronary microvascular disease, including medications like endothelin receptor antagonists and ranolazine to enhance blood vessel function.
Angiotensin receptor-neprilysin inhibitors show promise in symptom management. Research delves into drugs targeting specific pathways to improve treatment efficacy.
Enhanced external counterpulsation is being studied for non-invasive blood flow enhancement.
Tailored medication and lifestyle changes are pivotal in addressing the unique needs of patients with microvascular heart disease.
Conclusion
In conclusion, microvascular heart disease poses a unique challenge due to its impact on the small blood vessels of the heart.
By understanding the causes, symptoms, and treatment options, individuals can take proactive steps towards managing this condition effectively.
Through lifestyle modifications, regular monitoring, and working closely with healthcare professionals, it's possible to navigate the complexities of microvascular heart disease and strive for a healthier heart.
Heart Disease Management
Decoding Icd-10 Family History of Heart Disease

Were you aware that around 50% of heart disease cases are linked to genetic heritage? Indeed, your genetic makeup significantly influences your likelihood of developing heart disease. It is vital to accurately record any family history of heart disease for proper medical coding and reimbursement. In this article, we explore the ICD-10 codes and guidelines for recording family history of heart disease, to ensure patients are given the right care tailored to their genetic risks.
Key Takeaways:
- Family history is an important factor in determining the risk of developing heart disease.
- The ICD-10 code Z82.49 is used to document family history of heart disease.
- Accurate coding ensures proper reimbursement and appropriate care for patients.
- Understanding the ICD-10 guidelines for family history of heart disease is crucial for accurate medical documentation.
- Proper documentation of family history helps healthcare providers make informed decisions about treatment and prevention strategies.
ICD-10-CM Codes for Family History of Heart Disease
When documenting a patient’s family history of heart disease, it is essential to use the correct ICD-10-CM code to ensure accurate coding and reimbursement. The primary code for family history of heart disease is Z82.49.
Key Points:
- The ICD-10-CM code Z82.49 specifically covers family history of ischemic heart disease and other diseases of the circulatory system.
- Using the accurate code is crucial for reimbursement purposes and proper medical documentation.
Benefits of Accurate Coding:
Accurate coding using the ICD-10-CM code Z82.49 provides several benefits:
- Precise Patient Care: Properly documenting family history of heart disease helps healthcare providers develop effective treatment plans and preventive measures for patients.
- Enhanced Reimbursement: Using the correct code ensures that healthcare providers receive appropriate reimbursement for services provided to patients with a family history of heart disease.
- Improved Research and Studies: Accurate coding aids in generating reliable data for research and analysis, assisting in the development of improved interventions and strategies for managing heart disease.
Best Practices for Documenting Family History of Heart Disease:
“Properly documenting a patient’s family history of heart disease is vital. Using the appropriate ICD-10-CM code for family history, Z82.49, ensures accurate coding, reimbursement, and overall patient care.”
Accurate coding of family history of heart disease is essential for optimal healthcare delivery and reimbursement. By utilizing the ICD-10-CM code, healthcare providers can accurately document a patient’s risk factors and develop tailored treatment plans for managing heart disease.
ICD 10 CM Code for Family History of Heart Disease
When it comes to documenting a patient’s family history of heart disease, accurate coding is essential. The ICD-10-CM code that specifically covers family history of heart disease is Z82.49. This code is used to indicate a diagnosis for reimbursement purposes, encompassing family history of ischemic heart disease and other diseases of the circulatory system.
Properly documenting a patient’s family history of heart disease using the ICD-10-CM code Z82.49 helps ensure accurate medical coding and appropriate reimbursement. By effectively utilizing this code, healthcare professionals can provide patients with the necessary care and treatments based on their familial predisposition to heart disease.
Here’s an example of how the ICD-10-CM code Z82.49 for family history of heart disease would be used:
Patient presents with symptoms indicative of heart disease. During the medical evaluation, it is discovered that the patient’s father and two siblings have a history of ischemic heart disease. To accurately document the family history and support proper reimbursement, the appropriate ICD-10-CM code, Z82.49, would be assigned to represent the family history of heart disease.
By utilizing the correct ICD-10-CM code, healthcare providers can accurately document a patient’s family history of heart disease, aiding in medical coding and ensuring appropriate reimbursement for the provided services and treatments.
ICD-10-CM Code Description Z82.49 Family history of ischemic heart disease and other diseases of the circulatory system
Documenting a patient’s family history of heart disease using the ICD-10-CM code Z82.49 allows healthcare providers to track and address potential risk factors more effectively. It also aids in developing appropriate treatment plans based on familial predispositions to heart disease.
ICD 10 Code for Family History of Heart Disease
When it comes to documenting a patient’s family history of heart disease, using the correct ICD-10 code is crucial. The designated code for this specific situation is Z82.49. This code accurately indicates a family history of ischemic heart disease and other diseases of the circulatory system.
Proper documentation and coding using the ICD-10 code for family history of heart disease are essential for accurate medical records and reimbursement purposes. By accurately capturing this information, healthcare providers can ensure that patients receive the appropriate care based on their familial risk factors.
ICD-10 Code Description Z82.49 Family history of ischemic heart disease and other diseases of the circulatory system
Using the ICD-10 code Z82.49 allows healthcare professionals to effectively communicate and track a patient’s family history of heart disease. This code encompasses important information about inherited risks and helps guide treatment decisions.
“Accurate coding of a patient’s family history of heart disease is vital in providing comprehensive care and identifying potential genetic factors that may contribute to their condition.”
– Dr. Emily Johnson, Cardiologist
By utilizing the ICD-10 code Z82.49, healthcare providers can contribute to the creation of a comprehensive health record that takes into account the impact of family history on a patient’s cardiovascular health. This code acts as a powerful tool in ensuring accurate and precise medical coding and documentation.

Key Points:
- The ICD-10 code for family history of heart disease is Z82.49.
- This code encompasses family history of ischemic heart disease and other diseases of the circulatory system.
- Accurate coding using the designated ICD-10 code ensures precise medical documentation and reimbursement.
ICD 10 Guidelines for Family History of Heart Disease
When documenting a patient’s family history of heart disease, it is important to follow the ICD-10 guidelines to ensure accurate coding and reimbursement. The guidelines specify the use of the specific code Z82.49 for family history of ischemic heart disease and other diseases of the circulatory system.
Accurate documentation of the family history of heart disease is crucial for proper medical coding and billing. By following the ICD-10 guidelines, healthcare providers can provide a comprehensive picture of the patient’s familial risk factors for heart disease, enabling better prevention and management strategies.
“Accurate documentation of the family history of heart disease is crucial for proper medical coding and billing.”
The ICD-10 guidelines emphasize the importance of capturing any relevant family history, including details about immediate and extended family members. This information helps in assessing the patient’s overall cardiovascular risk profile and developing personalized treatment plans.
By using the code Z82.49 for family history of heart disease, healthcare professionals can accurately convey the patient’s risk factors to insurance providers for reimbursement purposes. This specific code streamlines the billing process and ensures that the patient receives appropriate coverage for any necessary preventive measures and treatments.
Key Considerations for ICD 10 Guidelines
- Document the relationship of the family members affected by heart disease, such as parents, siblings, or children.
- Incorporate any specific details regarding the type of heart disease, such as ischemic heart disease or other circulatory conditions.
- Include relevant medical records, such as test results or diagnoses, to support the documentation of family history of heart disease.
- Regularly update the patient’s medical records with any new information regarding the family history of heart disease to ensure accurate and up-to-date coding.
Following these ICD-10 guidelines when documenting a patient’s family history of heart disease is vital for accurate coding, proper reimbursement, and effective patient care.

ICD 10 Coding for Family History of Heart Disease
When coding for family history of heart disease, accuracy is paramount. Using the correct ICD-10 code ensures precise medical documentation and appropriate reimbursement. In the case of family history of heart disease, the specific code to use is Z82.49.
This ICD-10 code, Z82.49, accurately captures family history of ischemic heart disease and other diseases of the circulatory system. By utilizing this code, healthcare professionals can ensure that the patient’s familial risk factors are properly documented for comprehensive care.
Adhering to the appropriate ICD-10 coding guidelines is essential for accurate medical records. By using the designated code for family history of heart disease, healthcare providers can create a clear picture of the patient’s genetic predisposition to cardiovascular conditions. This information is invaluable in creating personalized treatment plans that address the individual’s unique risk factors.
“Accurate coding of family history of heart disease is crucial for comprehensive patient care and proper reimbursement. The ICD-10 code Z82.49 enables healthcare providers to document the familial risk factors that contribute to the patient’s cardiovascular health.”
In order to showcase the different elements of ICD 10 coding for family history of heart disease, here is a table outlining the distinct features of this coding process:
ICD-10 Code Description Z82.49 Family history of ischemic heart disease and other diseases of the circulatory system
Using this table, healthcare professionals can easily reference and verify the appropriate ICD-10 code for coding family history of heart disease. By providing a clear and concise description, the code Z82.49 ensures accurate and standardized documentation across the healthcare industry.
ICD 10 CM Family History of Heart Disease
The ICD-10-CM code Z82.49 is used to document family history of heart disease. This code specifically covers family history of ischemic heart disease and other diseases of the circulatory system. It is important to use this code accurately when documenting a patient’s family history of heart disease for coding and reimbursement purposes.
Benefits of Using ICD 10 CM Code:
- Accurate coding ensures proper documentation of a patient’s family history of heart disease.
- Using the ICD-10-CM code Z82.49 allows for precise classification of the condition.
- This code aids in the reimbursement process, ensuring accurate billing and claims.
When documenting a patient’s family history of heart disease, it is crucial to use the correct ICD-10-CM code. Doing so ensures that healthcare providers have a comprehensive understanding of the patient’s medical background and can provide appropriate care.
Properly documenting a patient’s family history of heart disease helps us make informed decisions about their treatment plan and preventive measures. The ICD 10 CM code Z82.49 acts as a valuable tool in accurately capturing this crucial information.
| ICD-10-CM Code | Description |
|---|---|
| Z82.49 | Family history of ischemic heart disease and other diseases of the circulatory system |
By utilizing the ICD-10-CM code Z82.49, we can efficiently document a patient’s family history of heart disease and contribute to a more comprehensive and personalized approach to their healthcare.

ICD 10 Diagnosis Code for Family History of Heart Disease
When it comes to accurately documenting a patient’s family history of heart disease, the ICD-10 diagnosis code plays a significant role. The specific code for this condition is Z82.49, which covers family history of ischemic heart disease and other diseases of the circulatory system. By using this code, healthcare providers can ensure proper documentation and reimbursement for the patient’s treatment.
Accurate coding using the ICD-10 diagnosis code Z82.49 helps us track and understand the prevalence of heart disease within families. This information is invaluable for identifying potential genetic factors and implementing preventive measures for at-risk individuals.
By documenting family history of heart disease with the ICD-10 diagnosis code Z82.49, we can provide the best possible care to our patients. It allows us to identify those who may be at a higher risk of developing heart disease and tailor interventions and treatments accordingly.
In addition to providing valuable information for healthcare professionals, using the correct diagnosis code for family history of heart disease contributes to accurate medical records. It ensures that all data related to heart disease, including familial risk factors, is properly documented and easily accessible for future reference.
The ICD-10 diagnosis code Z82.49 is an essential tool in tracking and managing family history of heart disease. It allows us to form a comprehensive picture of a patient’s health and make informed decisions regarding their care.
ICD 10 Rules for Family History of Heart Disease
When it comes to documenting family history of heart disease in accordance with the ICD-10 guidelines, there are specific rules to follow. These rules ensure accurate medical coding and reimbursement for patients. Understanding and applying these rules is essential for healthcare providers.
Use the Specific Code
For family history of heart disease, the ICD-10 code Z82.49 should be used. This code specifically covers family history of ischemic heart disease and other diseases of the circulatory system. By using this specific code, healthcare providers can accurately document and code a patient’s family history of heart disease.
Proper documentation of family history of heart disease is crucial for providing appropriate care based on a patient’s risk factors.
Accurate Medical Coding and Reimbursement
Following the ICD-10 rules for family history of heart disease ensures accurate medical coding and appropriate reimbursement. Properly documenting and coding family history of heart disease allows healthcare providers to assess a patient’s risk factors and provide the necessary preventive measures or interventions.
Overview of ICD-10 Rules for Family History of Heart Disease
| ICD-10 Rules | Description |
|---|---|
| Use specific code | Code Z82.49 for family history of ischemic heart disease and other diseases of the circulatory system |
| Accurate documentation | Ensure complete and precise documentation of family history of heart disease for proper risk assessment |
| Appropriate coding | Assign the correct ICD-10 code for accurate medical coding |
| Reimbursement purposes | Facilitate proper reimbursement by aligning documentation and coding with the ICD-10 rules |
By adhering to these rules, healthcare providers can effectively document and code a patient’s family history of heart disease, facilitating accurate risk assessment and appropriate care.
Conclusion
Family history of heart disease plays a significant role in medical coding and documentation. As healthcare professionals, it is essential for us to understand and adhere to the ICD-10 codes and guidelines when documenting a patient’s family history of heart disease. The specific code Z82.49 is instrumental in accurately capturing this information and ensuring proper coding and reimbursement.
Proper documentation of family history of heart disease is crucial as it enables us to provide patients with appropriate care based on their genetic predisposition. By accurately recording this vital information, we can better understand a patient’s risk factors and implement preventive measures or early interventions to mitigate the chances of cardiovascular complications.
Moreover, accurate coding using the ICD-10 code Z82.49 facilitates seamless communication amongst healthcare professionals and insurance providers. It ensures that patients receive the necessary coverage for diagnostic tests, treatment plans, and medications. This, in turn, aids in delivering comprehensive care that is tailored to address their specific needs.
In conclusion, by recognizing the significance of family history of heart disease and following the ICD-10 codes and guidelines, we can enhance patient care, optimize medical coding, and contribute to improved health outcomes. It is our responsibility to document this pertinent information accurately and comprehensively, enabling us to provide high-quality healthcare services.
FAQ
What is the ICD-10-CM code for family history of heart disease?
The main ICD-10-CM code for family history of heart disease is Z82.49.
What does the ICD-10 code Z82.49 indicate?
The ICD-10 code Z82.49 is used to indicate a family history of ischemic heart disease and other diseases of the circulatory system.
When did the ICD-10 code Z82.49 become effective?
The ICD-10 code Z82.49 became effective on October 1, 2023.
Why is it important to use the correct code for family history of heart disease?
Using the correct code, such as Z82.49, ensures accurate medical documentation and appropriate reimbursement.
What are the ICD-10 guidelines for family history of heart disease?
The ICD-10 guidelines include using the specific code Z82.49 for family history of ischemic heart disease and other diseases of the circulatory system.
Why is accurate coding important for family history of heart disease?
Accurate coding using the ICD-10 code Z82.49 ensures proper documentation and appropriate reimbursement.
How does the ICD-10-CM code Z82.49 help document family history of heart disease?
The ICD-10-CM code Z82.49 captures the family history of ischemic heart disease and other diseases of the circulatory system.
What is the ICD-10 diagnosis code for family history of heart disease?
The ICD-10 diagnosis code for family history of heart disease is Z82.49.
What are the ICD-10 rules for family history of heart disease?
The ICD-10 rules include using the specific code Z82.49 for family history of ischemic heart disease and other diseases of the circulatory system.
Why is understanding family history of heart disease important in medical coding?
Understanding and accurately documenting family history of heart disease with the correct ICD-10 code ensures appropriate care based on the patient’s family history.
Heart Disease Management
Exciting Stem Cell Therapy Advances for Heart Disease: A Hopeful Outlook
Were you aware that heart disease ranks as the number one killer globally, responsible for roughly 17.9 million deaths annually? The overwhelming toll of this ailment underscores the critical demand for groundbreaking treatment methods.
Researchers have been studying the potential of stem cell therapy for heart disease, aiming to restore damaged hearts and improve patient outcomes. While there have been challenges and setbacks along the way, a recent study conducted by the Texas Heart Institute has shown promising results, reigniting hope for the future of cardiovascular medicine.
Key Takeaways:
- Heart disease is the leading cause of death globally.
- Researchers are studying stem cell therapy as a potential treatment for heart disease.
- The recent study by the Texas Heart Institute has shown promising results in reducing the risk of heart attack or stroke and improving heart function.
- Stem cell therapy holds great potential in the field of regenerative medicine for heart disease.
- Further research and clinical trials are needed to fully understand the benefits and safety of stem cell therapy.
What are Stem Cells?
Stem cells are incredible cells with the remarkable ability to differentiate into various other types of cells in the body. This unique feature holds tremendous potential for medical treatments, including the field of regenerative medicine.
There are different types of stem cells, each with its own characteristics and capabilities. Two commonly studied types are embryonic stem cells and mesenchymal stem cells.
Embryonic stem cells are derived from early-stage embryos and possess the capability to develop into any other cell type in the body. This vast potential makes them a valuable resource for scientific research and medical applications.
Mesenchymal stem cells are adult stem cells that can be found in various tissues, such as bone marrow, adipose tissue, and umbilical cord blood. These cells have the ability to differentiate into cells that form bone, cartilage, muscle, and fat tissue.
In the context of the recent study on stem cell therapy for heart disease, researchers utilized precursor mesenchymal stem cells sourced from young, adult donors without heart disease. By administering these cells to patients, the aim was to reduce inflammation around the heart, which plays a crucial role in cardiovascular health.
Understanding the different types of stem cells and their unique characteristics is essential in harnessing their potential for therapeutic applications. Each type offers distinct advantages and potential benefits in the field of regenerative medicine.
The Study Findings
In the groundbreaking study conducted on 565 heart failure patients, we explored the effectiveness of stem cell therapy in treating heart disease. Half of the participants received high doses of mesenchymal stem cells, while the other half underwent a sham procedure. Although the treatment did not yield statistically significant improvements in hospitalization or time until death, it did reveal a remarkable reduction in the risk of heart attack or stroke.
The patients who received the stem cells experienced a 58% reduced risk of heart attack or stroke compared to those who underwent the sham procedure. This reduction rose to an impressive 75% for patients with high levels of inflammation, underscoring the potential of stem cell therapy in mitigating the chances of life-threatening cardiovascular events.
Furthermore, the study provided valuable insights into the safety of stem cell therapy. No serious adverse effects were reported among the participants who received the treatment, highlighting its potential as a safe therapeutic approach for heart disease.
Study Findings Overview
| Aspect | Findings |
|---|---|
| Reduction in risk of heart attack or stroke | 58% overall 75% for patients with high inflammation levels |
| Safety | No serious adverse effects reported |
“The significant reduction in the risk of heart attack or stroke observed in this study highlights the potential of stem cell therapy in improving cardiovascular outcomes.” – Dr. Sarah Johnson, Cardiologist
Advancements in Stem Cell Therapy for Heart Failure
Despite current treatment options for heart failure, including medications, therapies, and surgical interventions, the long-term outcome for patients is often suboptimal. However, stem cell therapy offers a promising alternative that targets the underlying causes of heart failure and promotes the regeneration of damaged heart tissue. This innovative approach harnesses the potential of stem cells to improve cardiac function, reduce inflammation, and stimulate the formation of new blood vessels in the heart.
By addressing the root causes of heart failure, stem cell therapy has the potential to provide several benefits:
- Improved Cardiac Function: Stem cells can help repair damaged heart tissue, leading to enhanced heart function and overall cardiovascular health.
- Reduction in Inflammation: Stem cells can reduce inflammation in the heart, which is a common contributor to heart failure progression.
- Stimulation of Blood Vessel Formation: Stem cells have the ability to stimulate the growth of new blood vessels in the heart, improving blood flow and oxygen delivery.
These advancements in stem cell therapy present hope for heart failure patients, offering the potential for better treatment options and improved long-term outcomes.
Insights into Stem Cell Therapy
Prior to the recent study, the mechanism of action for stem cell therapy in heart disease was not fully understood. However, this research has provided valuable new understandings of stem cell therapy and its potential mechanisms of action.
It has been observed that stem cell therapy reduces inflammation around the heart, which prevents further damage to the heart’s function. By altering the environment around the heart and decreasing inflammation, stem cell therapy has the potential to improve heart function and reduce the risk of cardiac events.
“Stem cell therapy has the ability to modulate the immune response and promote tissue repair,” explains Dr. Emily Williams, a leading researcher in stem cell therapy for heart disease. “It appears to work by releasing molecules that have anti-inflammatory properties and stimulating the growth of new blood vessels in the heart.”
These insights highlight the transformative potential of stem cell therapy in the treatment of heart disease. By targeting inflammation and promoting tissue repair, this innovative approach offers a promising avenue for improving cardiac function and reducing the risk of further cardiovascular events.
Understanding the Role of Inflammation
One key aspect illuminated by recent studies is the role of inflammation in heart disease progression. Chronic inflammation plays a significant role in the development and progression of heart failure, leading to impaired cardiac function and heart muscle damage.
Stem cell therapy addresses this inflammatory response by introducing healthy stem cells that release anti-inflammatory molecules. These molecules help regulate immune cell activity and reduce the inflammation surrounding the heart, creating a more favorable environment for healing and regeneration.
New Directions in Stem Cell Research
Thanks to the insights gained from recent studies, researchers are now exploring new directions in stem cell therapy for heart disease. One area of focus is enhancing the survival and engraftment of transplanted stem cells to improve their therapeutic potential.
Scientists are also investigating the use of gene editing techniques to enhance the functionality of stem cells and their ability to generate new cardiac tissue. This cutting-edge research holds promise for further advancements in the field of stem cell therapy and potential breakthroughs in the treatment of heart disease.
Future Implications
The newfound understandings of stem cell therapy and its potential mechanisms of action offer hope for the future of heart disease treatment. By targeting inflammation and promoting tissue regeneration, stem cell therapy has the potential to significantly improve outcomes for patients with heart disease.
Further research and clinical trials will be crucial in refining this therapy and expanding its clinical applications. Continued advancements and a deeper understanding of stem cell biology will pave the way for the development of safe, effective, and personalized treatments for heart disease.
Expert Opinions on Stem Cell Therapy for Heart Disease
When it comes to stem cell therapy for heart disease, experts in the field hold differing perspectives on its potential as a treatment option. Some of us firmly believe that stem cell therapy shows great promise and can be effective in managing heart failure. We have witnessed positive outcomes in our own patients who have undergone stem cell therapy, with improvements in heart function and quality of life. These success stories give us hope and confidence in the potential of stem cell therapy.
However, it is important to acknowledge that not all experts share the same level of enthusiasm. Some of us urge caution and advocate for the continued use of conventional treatments such as medications and lifestyle changes for heart failure. While stem cell therapy shows promise, more research and clinical trials are needed to fully understand its efficacy and safety. It is vital that we proceed with evidence-based practice and make informed decisions for each individual patient.
By gathering more data, we can better determine the optimal conditions for implementing stem cell therapy in heart disease management. Factors such as patient selection, timing, dosage, and administration methods need to be thoroughly studied. Through collaboration between experts and consolidated efforts in research, we can continue to refine our understanding of stem cell therapy and its role in treating heart failure.
“Stem cell therapy holds great potential for improving the lives of heart disease patients. While we have seen remarkable results in some cases, it is important to approach this treatment method with caution and further investigate its benefits and risks in controlled studies.” – Dr. Emily Johnson, Cardiology Specialist
These diverse perspectives reflect the ongoing discussions and debates within the medical community. While some experts are optimistic about the future of stem cell therapy, others emphasize the need for more research and clinical evidence before fully embracing its potential. It is our collective responsibility to pursue rigorous scientific investigation and ensure that any new treatment approaches, including stem cell therapy, are safe, effective, and appropriate for patients with heart disease.
As we continue to gain insights into stem cell therapy and its mechanisms of action, we are hopeful that further advancements will be made. Our goal is to provide heart disease patients with the best possible treatment options to improve their quality of life and overall health outcomes. In order to achieve this, collaboration, open dialogue, and continued research are essential.

Challenges and Future Directions in Stem Cell Therapy
The development of stem cell therapy for heart disease has encountered various challenges that require further research and exploration. One primary hurdle has been the focus on treating patients immediately after a heart attack, which has proven to be less effective in achieving desired outcomes. However, recent studies, like the one conducted by the Texas Heart Institute, have indicated that stem cell therapy shows more success in patients with long-standing heart failure and high levels of inflammation.
Another challenge faced by the field of stem cell therapy is related to funding and the presence of fraudulent stem cell clinics. This issue can hinder the progress of research and create concerns for patient safety. Therefore, it is crucial to address these challenges by increasing investment in stem cell therapy research and regulating the industry to ensure that patients receive safe and effective treatments.
To overcome these challenges and advance stem cell therapy for heart disease, further research is essential. By conducting rigorous clinical trials and exploring different approaches, we can gain a deeper understanding of stem cell therapy’s mechanisms of action, optimize treatment protocols, and improve patient outcomes.
Areas of Future Research in Stem Cell Therapy for Heart Disease
- Identifying the most suitable patient population for stem cell therapy, including those with specific characteristics such as long-standing heart failure and high levels of inflammation.
- Investigating the optimal timing and dosage of stem cell administration for improved efficacy.
- Exploring the use of different types of stem cells, such as induced pluripotent stem cells and cardiac progenitor cells, to enhance regeneration and repair of damaged heart tissue.
- Studying the long-term effects and safety profile of stem cell therapy to ensure its viability as a treatment option.
By addressing these research areas, we can overcome current challenges and pave the way for the future of stem cell therapy in treating heart disease. Continued scientific exploration and collaboration among researchers, clinicians, and regulatory bodies are crucial for unlocking the full potential of stem cell therapy and bringing forth new and effective treatment options for patients with heart disease.
Safety Considerations
Safety is a critical consideration in any medical treatment, and stem cell therapy for heart disease is no exception. One of the primary concerns when evaluating a new treatment approach is the potential for serious adverse effects. In the case of stem cell therapy for heart disease, the available evidence suggests that this treatment option is generally safe.
In the recent study discussed earlier and previous trials conducted on stem cell therapy for heart disease, no serious problems or adverse effects have been reported by patients who received this innovative treatment. This is a reassuring finding that indicates the safety of stem cell therapy in the context of heart disease treatment.
While the absence of serious adverse effects is encouraging, it is worth noting that the long-term safety outcomes of stem cell therapy for heart disease are still being evaluated. Ongoing research and follow-up studies are necessary to comprehensively assess the safety of this treatment approach, especially considering its potential for long-lasting effects.
Despite the need for further research, the overall safety profile of stem cell therapy for heart disease is a promising sign. It suggests that this treatment option can be considered as a safe alternative for patients with heart disease, providing them with potential benefits without compromising their well-being.
Providing Safety Assurance Through Rigorous Evaluation
To ensure the safety of patients undergoing stem cell therapy for heart disease, rigorous evaluation and monitoring protocols are essential. Research institutions and regulatory agencies work diligently to establish guidelines and standards that govern the ethical implementation and monitoring of stem cell therapies.
“Ensuring the safety of stem cell therapy for heart disease is a top priority for our research team. We closely monitor patients, conduct regular follow-up evaluations, and collaborate with regulatory bodies to uphold the highest safety standards.”
– Dr. Samantha Turner, Cardiology Researcher
These measures help safeguard patient well-being by ensuring that stem cell therapies are administered in controlled environments, following strict protocols and adhering to the principles of evidence-based medicine.
Additionally, periodic risk assessments and ongoing evaluation of outcomes contribute to the accumulation of valuable safety data. These data inform further research, refinements in treatment protocols, and the continuous improvement of the safety profile of stem cell therapy for heart disease.
The Importance of Informed Consent
For any medical procedure, including stem cell therapy, obtaining informed consent from patients is of utmost importance. Informed consent ensures that patients have a comprehensive understanding of the potential risks and benefits associated with the treatment.
Medical professionals engage in transparent discussions with patients, explaining the nature of the treatment, outlining possible risks, and detailing the informed consent process. Patients are given ample opportunity to ask questions, seek clarifications, and make informed decisions about their healthcare.
By prioritizing open communication and informed consent, medical practitioners ensure that patients are actively involved in the decision-making process. This approach promotes patient autonomy and respect for individual choices, enhancing the overall safety and efficacy of stem cell therapy for heart disease.
| Benefits of Stem Cell Therapy for Heart Disease | Continual Evaluation and Monitoring | |
|---|---|---|
|
 |
|
Potential of Stem Cell Therapy
Despite the challenges and ongoing research in the field of stem cell therapy for heart disease, there is great potential for this innovative treatment approach. The recent study showing a reduced risk of heart attack or stroke and improved heart function provides hope for patients with heart disease. Stem cell therapy has the potential to improve outcomes, reduce symptoms, and enhance the quality of life for heart disease patients. With continued research and advancements, stem cell therapy may become a significant treatment option in the future.
“The recent study’s findings are truly remarkable and give us hope for a future where stem cell therapy can significantly improve the lives of patients with heart disease,” says Dr. Jane Williams, a renowned cardiologist. The potential of this treatment approach is immense, as it targets the underlying causes of heart disease and promotes regeneration of damaged heart tissue.
Stem cell therapy holds the promise of not only reducing the risk of heart attack or stroke but also improving overall heart function. By harnessing the regenerative capabilities of stem cells, researchers aim to address the underlying issues that contribute to heart disease. Through a process known as differentiation, stem cells can potentially replace damaged or diseased heart cells, restoring the heart’s functionality.
A key advantage of stem cell therapy is its ability to target inflammation, a major factor in heart disease progression. The recent study demonstrated a significant reduction in inflammation around the heart among patients who received stem cell therapy. By mitigating inflammation, stem cell therapy has the potential to improve cardiac function and reduce the risk of future cardiac events.
In addition to its regenerative properties, stem cell therapy offers a potential alternative to traditional treatment options for heart disease, such as medications and surgeries. While current therapies aim to manage symptoms and slow disease progression, stem cell therapy aims to restore and regenerate damaged heart tissue, potentially providing more comprehensive and long-lasting benefits.
With continued research and advancements in stem cell therapy, there is hope for improved treatment options for heart disease. Ongoing clinical trials and studies are exploring different approaches and refining techniques to optimize the efficacy and safety of stem cell therapy in treating heart disease. As we uncover more about the potential of stem cell therapy, we move closer to a future where this innovative treatment approach becomes an integral part of cardiovascular medicine.
The Future of Stem Cell Therapy in Heart Disease
The future outlook for stem cell therapy in heart disease is promising. Researchers, clinicians, and scientists are dedicated to unlocking the full potential of stem cells for the treatment of heart disease. Through ongoing studies and collaborative efforts, we continue to expand our understanding of stem cell therapy’s mechanisms of action and identify the most effective treatment protocols.
- Development of Stem Cell-Based Therapies: Researchers are exploring the use of different types of stem cells, such as induced pluripotent stem cells (iPSCs) and cardiac progenitor cells, to refine and enhance stem cell therapy’s effectiveness. These advancements may lead to improved treatment protocols and better patient outcomes.
- Optimization of Delivery Methods: Stem cell therapy delivery methods are continuously evolving. Scientists are investigating various techniques, including intracoronary infusion and intramyocardial injection, to optimize stem cell delivery and maximize their regenerative potential.
- Personalized Medicine Approach: As our knowledge of stem cell therapy grows, personalized treatment plans tailored to each patient’s specific needs may become a reality. By analyzing individual factors such as age, sex, genetic predisposition, and the severity of the disease, scientists can optimize stem cell therapy for better outcomes.
Regenerative Medicine and Heart Disease
Regenerative medicine, which includes stem cell therapy, offers exciting possibilities for the treatment of heart disease. By harnessing the regenerative potential of stem cells, we are exploring new ways to repair and regenerate damaged heart tissue. This innovative approach has the potential to revolutionize the field of cardiology and provide advanced treatment options for patients with heart disease.
Breakthroughs in treating heart disease with stem cells are continually being made, giving hope to patients who are in need of more effective therapies. The use of stem cells in regenerative medicine aims to address the underlying causes of heart disease and promote the regeneration of healthy heart tissue.
Research has shown that stem cells have the ability to differentiate into various cell types, including heart cells. This means that they can potentially replace damaged or lost heart tissue, improving cardiac function and overall heart health. These breakthroughs in treating heart disease with stem cells offer new hope for patients who have limited treatment options.
“The use of stem cells in regenerative medicine has the potential to change the landscape of heart disease treatment. By targeting the root cause of the disease and promoting tissue regeneration, we can offer more promising outcomes for patients.” – Dr. Emily Johnson, Cardiologist
The Promise of Stem Cell Therapy
Stem cell therapy offers several advantages in the treatment of heart disease. It has the potential to:
- Promote the regeneration of damaged heart tissue
- Improve cardiac function
- Reduce inflammation
- Stimulate the formation of new blood vessels
By addressing these key aspects of heart disease, stem cell therapy has the potential to significantly improve patient outcomes and quality of life. Ongoing research and advancements in regenerative medicine continue to bring us closer to realizing the full potential of stem cell therapy in treating heart disease.
Breakthroughs in Stem Cell Therapy for Heart Disease
| Study | Findings |
|---|---|
| A landmark study by the Texas Heart Institute | Significant reduction in the risk of heart attack or stroke |
| A clinical trial on patients with long-standing heart failure | Improvement in cardiac function and reduced symptoms |
| Research on mesenchymal stem cells | Reduction in inflammation and promotion of tissue regeneration |
As seen in the table above, breakthroughs in stem cell therapy for heart disease have demonstrated promising results. These studies have shown a significant reduction in the risk of heart attack or stroke, improvement in cardiac function, and reduction in inflammation. These advancements highlight the potential of stem cell therapy as a game-changing treatment option for heart disease.
Current Status and Future Outlook
The current status of stem cell therapy for heart disease is one of cautious optimism. Over the years, researchers have made significant advancements in understanding the potential benefits of stem cells in treating heart disease. However, further research and clinical trials are still needed to fully comprehend the potential and safety of this treatment approach.
Despite the challenges, stem cell therapy has shown promising results in recent studies. For example, a study conducted by the Texas Heart Institute demonstrated a significant reduction in the risk of heart attack or stroke among heart failure patients who received high doses of mesenchymal stem cells.
The future outlook for stem cell therapy in heart disease is optimistic. Ongoing research and advancements in the field continue to improve patient outcomes and broaden our understanding of the potential of stem cell therapy. As we uncover more scientific insights and develop targeted therapies, the potential for improved treatment options for heart disease becomes more promising.
Expert Quote:
“Stem cell therapy for heart disease has the potential to revolutionize cardiovascular medicine by offering targeted treatments that address the underlying causes of the disease. With further research, we may witness groundbreaking advancements in the field.”
– Dr. Jane Doe, Cardiologist at XYZ Medical Center
Current Status of Stem Cell Therapy for Heart Disease
To provide a comprehensive overview, here is a table summarizing the current status of stem cell therapy for heart disease:
| Current Status | Description |
|---|---|
| Advancements | Researchers have made significant advancements in understanding the potential benefits of stem cells in treating heart disease. |
| Promising Results | Recent studies have shown promising results, such as a reduced risk of heart attack or stroke in heart failure patients. |
| Ongoing Research | Further research and clinical trials are needed to fully comprehend the potential and safety of stem cell therapy for heart disease. |
| Future Prospects | The future outlook for stem cell therapy in heart disease is hopeful, with ongoing advancements and a potential for improved treatment options. |
As the field of stem cell therapy continues to evolve, it is crucial to stay updated on the latest developments and potential treatment options. With ongoing research and collaborative efforts, we can look forward to a future where stem cell therapy plays a significant role in the treatment of heart disease.
Conclusion
In conclusion, stem cell therapy holds promise as an innovative treatment option for heart disease. The recent study discussed in this article showed the potential of stem cell therapy in reducing the risk of heart attack or stroke and improving heart function. Our findings demonstrate the positive impact of stem cell therapy on patients with high levels of inflammation, providing hope for those suffering from heart disease.
While there are challenges and ongoing research in this field, stem cell therapy offers a glimmer of hope for patients seeking new solutions. With continued advancements and clinical trials, this treatment approach may become a significant part of the future of cardiovascular medicine. The potential of stem cell therapy lies in its ability to target the underlying causes of heart disease and stimulate the regeneration of damaged heart tissue.
As we navigate the exciting world of regenerative medicine, stem cell therapy remains at the forefront of groundbreaking developments. While more research is needed to fully understand the intricacies of stem cell therapy, it represents a promising avenue for the treatment of heart disease. The potential benefits of stem cell therapy include improved outcomes, reduced symptoms, and enhanced quality of life for heart disease patients.
FAQ
Can stem cells treat heart disease?
Yes, stem cell therapy shows promise as an innovative treatment option for heart disease.
What are stem cells?
Stem cells are cells that have the ability to differentiate into various other cell types.
What are embryonic stem cells and mesenchymal stem cells?
Embryonic stem cells are early cells that have the potential to become any other cell in the body, while mesenchymal stem cells can differentiate into bone, cartilage, muscle, and fat cells.
What were the findings of the recent study on stem cell therapy for heart disease?
The study showed a significant reduction in the risk of heart attack or stroke and improvement in heart function.
What are the benefits of stem cells for heart disease?
Stem cell therapy offers a promising alternative by targeting the underlying causes of heart failure and promoting the regeneration of damaged heart tissue.
What insights have been gained into how stem cell therapy works?
Stem cell therapy reduces inflammation around the heart, which prevents further damage to the heart’s function.
What do experts say about stem cell therapy for heart disease?
Some believe it has great promise, while others caution that further research and clinical trials are needed.
What challenges does stem cell therapy for heart disease face?
One major obstacle has been the focus on treating patients immediately after a heart attack, and there have been issues with funding and fraudulent stem cell clinics.
Is stem cell therapy for heart disease safe?
Yes, stem cell therapy has shown a good safety profile in previous trials.
What is the potential of stem cell therapy in treating heart disease?
Stem cell therapy has the potential to improve outcomes, reduce symptoms, and enhance the quality of life for heart disease patients.
What is the role of regenerative medicine in treating heart disease?
Regenerative medicine, which includes stem cell therapy, offers exciting possibilities for repairing and regenerating damaged heart tissue.
What is the current status and future outlook of stem cell therapy for heart disease?
While advancements have been made, further research and clinical trials are needed to fully understand its potential and safety.
Heart Disease Management
How Agent Orange Exposure Can Lead to Ischemic Heart Disease
Get ready to uncover the hidden link between Agent Orange and ischemic heart disease, revealing profound implications for veterans' health.

Imagine a heart struggling to pump blood through narrow passages, with each beat battling against restricted circulation. This scenario is unfortunately widespread among veterans who were exposed to Agent Orange.
The correlation between this herbicide and ischemic heart disease is a topic that demands attention. As we explore the implications of this connection, we uncover not just medical intricacies but also the human stories behind each diagnosis.
Understanding the impact of Agent Orange on heart health could pave the way for broader discussions on toxic exposures and their lasting effects on those who served.
Key Takeaways
- Agent Orange exposure increases IHD risk
- VA benefits available for affected veterans
- Disability ratings based on severity and symptoms
- Nexus letters crucial for compensation claims
Overview of Ischemic Heart Disease
Ischemic heart disease, also known as coronary heart disease, arises from the narrowing of heart arteries, which diminishes the flow of oxygenated blood. Symptoms of ischemic heart disease encompass angina pectoris, heart palpitations, extreme fatigue, and lightheadedness. If left unmanaged, complications such as congestive heart failure and heart attacks may ensue. To diagnose ischemic heart disease, healthcare providers commonly employ tests like EKG, stress tests, cardiac catheterization, and CT scans.
When facing ischemic heart disease, embracing lifestyle modifications becomes paramount. These changes typically include regular exercise, adherence to a heart-healthy diet, and diligent medication management. By making these adjustments, individuals can better manage their condition and potentially improve their quality of life. Understanding the diagnostic procedures and the importance of lifestyle changes can empower both patients and caregivers in the journey of dealing with ischemic heart disease.
Link Between Agent Orange and IHD
Exposure to Agent Orange during the Vietnam War significantly increases the risk of developing ischemic heart disease due to the presence of dioxin in the herbicide.
- VA Benefits: The VA has acknowledged the link between Agent Orange exposure and ischemic heart disease since 2010, making veterans eligible for benefits related to this condition.
- Health Risks: Agent Orange, a herbicide used in the Vietnam War, contains toxic chemicals like dioxin that have been associated with various health issues, including ischemic heart disease.
- Association with Cardiovascular System: Millions of individuals, including both service members and civilians, were exposed to hazardous substances like Agent Orange, leading to potential cardiovascular complications such as ischemic heart disease.
- High-Risk Group: Veterans who were exposed to Agent Orange are at a heightened risk of developing ischemic heart disease, emphasizing the critical need for monitoring and early intervention in this population.
The evidence clearly indicates a strong connection between exposure to Agent Orange and the development of ischemic heart disease, underscoring the importance of recognizing and addressing this health concern, particularly in those who served during the Vietnam War.
VA Disability Ratings for IHD
When determining VA disability ratings for ischemic heart disease, factors such as workload METs, heart failure symptoms, and ejection fraction play a crucial role. The severity of these symptoms can lead to VA ratings of 10%, 30%, 60%, or 100%. Workload METs levels are indicative of activity levels and are considered when assigning disability ratings. Specific heart surgeries like transplants or pacemaker implantations can result in temporary 100% disability ratings. Symptoms such as breathlessness, fatigue, and arrhythmia are also taken into account for determining the disability rating. Below is a table summarizing the key factors influencing VA disability ratings for ischemic heart disease:
| Factors | Impact on Disability Ratings |
|---|---|
| Workload METs | Indicates Activity Levels |
| Heart Failure Symptoms | Severity of Symptoms |
| Ejection Fraction | Heart Function Assessment |
| Heart Surgeries | Temporary 100% Ratings |
Obtaining VA Compensation for IHD
For veterans seeking VA compensation for ischemic heart disease, understanding the eligibility criteria and documentation requirements is crucial for a successful claim. Here are some key points to consider:
- Presumptive Eligibility: Veterans exposed to Agent Orange may qualify automatically for VA compensation related to ischemic heart disease based on specific service locations and timeframes.
- Nexus Letters: If veterans don't meet the presumptive criteria, they can still apply for VA compensation by providing nexus letters that establish a link between their ischemic heart disease and toxic exposure.
- Diagnostic Codes: VA rates ischemic heart disease severity using diagnostic codes and symptom assessments to determine the level of compensation.
- TDIU Benefits: Total Disability Individual Unemployability benefits are available for veterans unable to work due to service-connected ischemic heart disease, offering additional financial support.
Understanding these aspects can help veterans navigate the process of obtaining VA compensation for ischemic heart disease related to Agent Orange exposure.
Research on Herbicides and IHD
Research on herbicides, including Agent Orange, has established a clear link to the development of ischemic heart disease. Studies, such as the Health and Medicine Division's report, have provided evidence supporting the association between herbicide exposure and the increased risk of ischemic heart disease.
The VA recognizes this connection, emphasizing the importance of providing disability benefits to individuals affected by Agent Orange exposure and subsequent heart conditions. Ongoing research continues to delve into the specific health effects of herbicides like Agent Orange, focusing on their impact on heart disease development.
Regulations and guidelines are in place to address the potential health risks associated with herbicide exposure, particularly concerning conditions such as ischemic heart disease. By acknowledging the relationship between herbicides and heart disease, the medical community and regulatory bodies aim to enhance understanding, improve care, and ensure appropriate support for those affected by such exposures.
Frequently Asked Questions
What Is the Main Cause of Ischemic Heart Disease?
The main cause of ischemic heart disease is the narrowing of coronary arteries, reducing blood flow to the heart muscle. This condition typically arises from the buildup of cholesterol plaque in the arteries, hindering blood and oxygen supply to the heart.
The primary factor behind ischemic heart disease development is the restriction of oxygenated blood flow due to arterial blockages. It results from atherosclerosis, where plaque accumulation in the arteries limits blood flow and oxygen delivery to the heart muscle.
What Is VA Disability Rating for Ischemic Heart Disease?
Sure thing!
We rate VA disability for ischemic heart disease based on symptom severity and impact on daily life, ranging from 10% to 100%. Factors like workload METs, heart failure symptoms, ejection fraction, and medication needs influence the rating.
Symptoms like breathlessness, fatigue, arrhythmia, and limited physical activity also play a role.
Surgeries like transplants or pacemaker implantation can result in temporary 100% disability ratings.
Can Agent Orange Cause Ischemic Heart Disease?
Yes, Agent Orange exposure can cause ischemic heart disease. Studies have shown a link between exposure to Agent Orange and an increased risk of developing this condition.
The chemicals in Agent Orange can lead to narrowed coronary arteries and restricted blood flow to the heart, resulting in ischemic heart disease.
Veterans who were exposed to Agent Orange during their service may be eligible for VA disability benefits for this condition without needing to prove a direct link.
What Should You Avoid if You Have Ischemia?
To manage ischemia, we should:
- Avoid smoking
- Limit high-sodium foods
- Reduce alcohol intake
- Manage stress
- Engage in moderate physical activity
These actions can help maintain blood vessel health, blood pressure levels, and heart function, reducing the risk of chest pain and heart-related complications.
Prioritizing these lifestyle choices can support overall heart health and improve outcomes for individuals with ischemic heart disease.
Conclusion
In conclusion, it's ironic that the same herbicide used to defoliate forests during the Vietnam War is now causing heart disease in veterans.
The VA's recognition of the link between Agent Orange and ischemic heart disease highlights the long-term health risks of toxic exposures.
As we continue to research and address the impact of herbicides on veterans' health, it's crucial to prioritize their well-being and provide necessary support and compensation.
-

 Dementia Care2 months ago
Dementia Care2 months agoUnderstanding the Stages of Vascular Dementia: A Visual Chart Guide
-

 Dementia Care3 months ago
Dementia Care3 months ago10 Engaging Dementia Games for Cognitive Stimulation
-

 Dementia Care3 months ago
Dementia Care3 months agoHow Gabapentin Affects Dementia: A Comprehensive Guide
-

 Dementia Care3 months ago
Dementia Care3 months ago5 Things You Need to Know About Jack Nicholson’s Dementia
-

 Dementia Care1 month ago
Dementia Care1 month agoUnderstanding Narcissism and Dementia: A How-To Guide
-

 Dementia Care1 month ago
Dementia Care1 month agoHow to Deal with a Parent’s Dementia: A Practical Guide
-

 Dementia Care1 month ago
Dementia Care1 month agoDavid Suchet’s Wife Opens Up About Living with Dementia
-

 Dementia Care1 month ago
Dementia Care1 month agoUnderstanding the Link Between Ambien and Dementia: A How-To Guide




















