As healthcare professionals, we recognize the significance of precise coding in guaranteeing adequate patient care and streamlining billing procedures, despite the initial challenges of comprehending the intricacies of ICD-10 Congenital Heart Disease.
The classification of CHD in the ICD-10 system provides a structured approach to identifying and managing these conditions, but what about the challenges that come along with it?
Stay tuned to discover how navigating through these challenges can ultimately lead to improved outcomes for patients with congenital heart disease.
Key Takeaways
- Proper ICD-10 coding crucial for accurate CHD diagnosis.
- Detailed classification aids in precise documentation and treatment planning.
- Accurate coding supports billing, reimbursement, and resource allocation.
- Continuous education essential to overcome coding challenges and improve patient care.
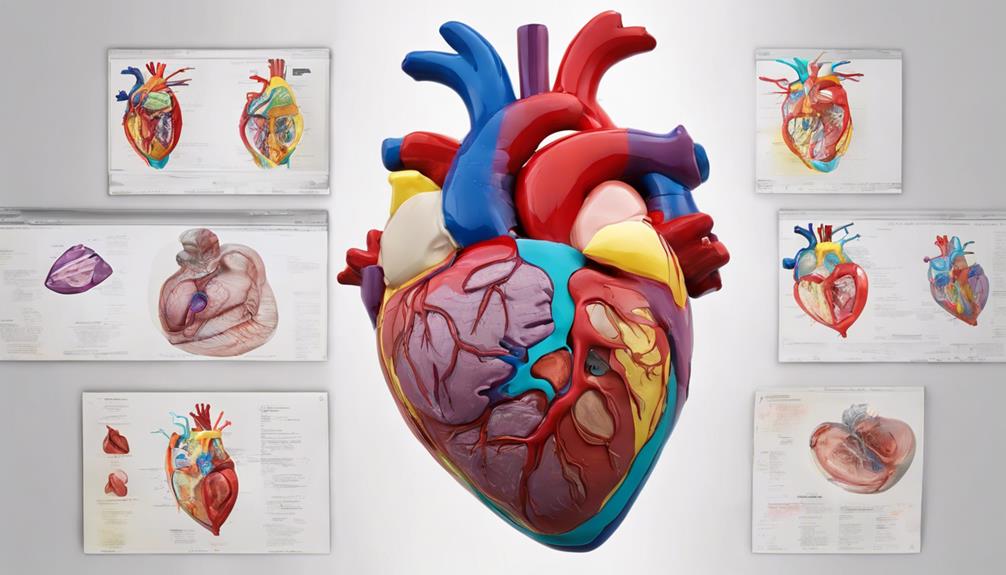
Overview of ICD-10 Codes for CHD
In our examination of the ICD-10 codes for Congenital Heart Disease (CHD), we delve into the intricate classification system that guides the diagnosis and treatment of this complex cardiac condition.
The ICD-10-CM code Q24.9 is a vital component in the classification of congenital malformations of the heart, providing detailed information on the specific type of malformation present. This code plays a crucial role in aiding healthcare professionals to accurately diagnose CHD and plan appropriate treatment strategies.
By understanding and correctly utilizing the ICD-10-CM code for congenital heart disease, healthcare providers can ensure effective coding, billing, and tracking of patient data related to CHD cases. The standardized documentation and reporting facilitated by this code are essential for maintaining consistency in handling congenital heart conditions across different healthcare settings.
Moreover, the ICD-10-CM code serves as a fundamental tool in enhancing communication among healthcare providers, insurers, and researchers involved in managing cases of congenital heart disease.
Classification of CHD in ICD-10

Classifying Congenital Heart Disease (CHD) in the ICD-10 system involves categorizing a diverse range of cardiac anomalies under specific codes from Q20 to Q28. These codes are crucial for accurately documenting congenital malformations of the heart. For instance, code Q24.9 represents 'Congenital malformation of heart, unspecified' in the ICD-10 classification. The ICD-10-CM offers detailed coding guidelines to ensure precise coding of CHD conditions. By utilizing these codes, healthcare providers can effectively track and monitor various cardiac anomalies, aiding in the diagnosis and treatment of patients with CHD.
Understanding the classification of CHD in the ICD-10 system is paramount for healthcare professionals involved in medical coding and billing processes. Proper classification enables accurate reimbursement, facilitates research on CHD prevalence and outcomes, and ensures appropriate treatment planning for individuals with congenital heart anomalies. Therefore, familiarity with the Q20-Q28 codes in the ICD-10 system is fundamental for providing quality care to patients with CHD.
Importance of Accurate Coding
Accurate coding plays a pivotal role in ensuring the effective tracking of patient conditions and treatment outcomes for congenital heart disease. When it comes to congenital malformations, precise coding is crucial for several reasons:
- Assessment of Prevalence: Proper coding enables healthcare providers to accurately assess the prevalence of congenital heart disease within populations. This data is essential for understanding the impact of these conditions on public health.
- Resource Allocation: Accurate coding supports appropriate billing, reimbursement, and resource allocation for congenital heart disease care. Properly coded information helps ensure that healthcare resources are allocated efficiently to meet the needs of patients with congenital heart conditions.
- Quality Improvement: Consistent and precise coding practices are essential for effective communication among healthcare professionals and accurate documentation of patient care. This documentation is critical for quality improvement efforts aimed at enhancing patient outcomes and overall healthcare delivery.
Challenges in Coding CHD

Navigating the intricate landscape of coding congenital heart disease (CHD) presents a myriad of challenges due to the diverse array of anomalies and complexities associated with various CHD types. One of the key challenges in accurately coding CHD lies in interpreting and applying the coding guidelines effectively. Understanding the intricate details of these guidelines is crucial for selecting the appropriate ICD-10-CM codes that reflect the specific CHD condition.
Moreover, staying abreast of the ever-evolving coding guidelines is essential to ensure compliance and accuracy in CHD coding practices. With the continuous updates and revisions in the guidelines, it becomes imperative for coding professionals to remain vigilant and informed about these changes to avoid coding errors and inaccuracies.
Furthermore, the complexity of CHD cases often requires a deep understanding of the nuances of the condition, making it challenging to assign the correct codes without a comprehensive grasp of the coding guidelines. Therefore, continuous education and training on coding practices related to CHD are vital for overcoming these challenges and ensuring precise coding in healthcare settings.
Enhancing Patient Care With ICD-10
Enhancing patient care with ICD-10 involves leveraging its detailed classification system to improve tracking of patient outcomes and treatment efficacy in congenital heart disease cases.
- Enhanced Tracking: By utilizing ICD-10 coding, healthcare providers can precisely document and code congenital heart diseases, allowing for better monitoring of patient progress and treatment effectiveness.
- Accurate Billing and Reimbursement: The improved specificity in ICD-10 enables accurate billing and reimbursement for treatments related to congenital heart disease, ensuring that healthcare facilities are appropriately compensated for the care provided.
- Improved Communication: ICD-10's detailed classification system aids in identifying specific types and severity of congenital heart defects, facilitating clearer communication among healthcare providers and ensuring consistent data reporting for better-coordinated patient care.
Through the meticulous application of ICD-10 in managing heart disease cases, healthcare professionals can significantly enhance the quality of care provided to individuals with congenital heart conditions.
Frequently Asked Questions
What Is the ICD-10 Code for Congenital Heart Disease Unspecified?
When identifying Congenital Heart Disease Unspecified, the ICD-10 code is Q24.9.
This code, falling under the category of Congenital Malformation of Heart, is utilized when the specific type of malformation isn't specified or known.
It's crucial for accurate medical coding and billing to employ the correct code, like Q24.9, to classify cases of congenital heart diseases with unspecified details.
The ICD-10-CM system offers detailed guidelines to ensure proper documentation and reimbursement.
What Is the ICD-10 Code for Congenital Heart Disease 2023?
We've got the answer you need for 2023!
The ICD-10 code for Congenital Heart Disease is Q24.9. This code specifies an unspecified congenital malformation of the heart, falling under the category of Congenital malformations in the ICD-10-CM coding system.
It's essential for accurate medical recordkeeping and helps medical professionals classify cases of congenital heart disease during diagnosis, treatment, and billing. Trust this standardized code for precise documentation.
What Is the Diagnosis of Congenital Heart Disease?
When diagnosing congenital heart disease, a comprehensive physical exam is crucial, involving careful listening for abnormal heart sounds and murmurs.
Diagnostic tools like echocardiograms, ECGs, and chest X-rays are commonly utilized to assess heart abnormalities. Additional tests such as cardiac catheterization and MRI provide detailed heart structure and function information.
Genetic testing may reveal underlying genetic causes. A team of specialists including pediatric cardiologists, cardiac surgeons, and genetic counselors work together for accurate diagnosis and treatment planning.
What Is the ICD-10 for Congenital Disease?
When looking at the ICD-10 for congenital disease, it's crucial to pinpoint the precise code for accurate classification. This aids healthcare providers in diagnosing, treating, and documenting cases effectively.
The ICD-10 coding system offers specific codes like Q24.9 for congenital malformations of the heart. Understanding these codes is essential for ensuring proper care and reporting of congenital heart conditions.
Conclusion
In conclusion, the utilization of the ICD-10-CM code Q24.9 for Congenital Malformation of Heart plays a vital role in accurately documenting and billing for cases of unspecified heart malformations.
By adhering to the guidelines and descriptors provided, healthcare professionals can effectively diagnose and manage congenital heart conditions.
Embracing the intricacies of coding CHD enhances the quality of patient care and contributes to improved outcomes in the realm of congenital heart disease management.