When delving into the topic of bone health, we frequently come across osteoarthritis and osteoporosis, both of which bring distinct challenges and effects on the body. Learn more about these conditions and their impact on our health. Come along on this informative journey!
While both conditions affect the skeletal system, their underlying mechanisms and consequences diverge significantly, prompting a closer examination to discern their distinguishing features.
Let's unravel the complexities of osteoarthritis versus osteoporosis and uncover the nuances that shape their management and impact on individuals' well-being.
Key Takeaways
- Osteoarthritis affects joints, causing discomfort; osteoporosis weakens bones, increasing fracture risk.
- Prevention involves lifestyle changes like exercise, diet, and avoiding risk factors.
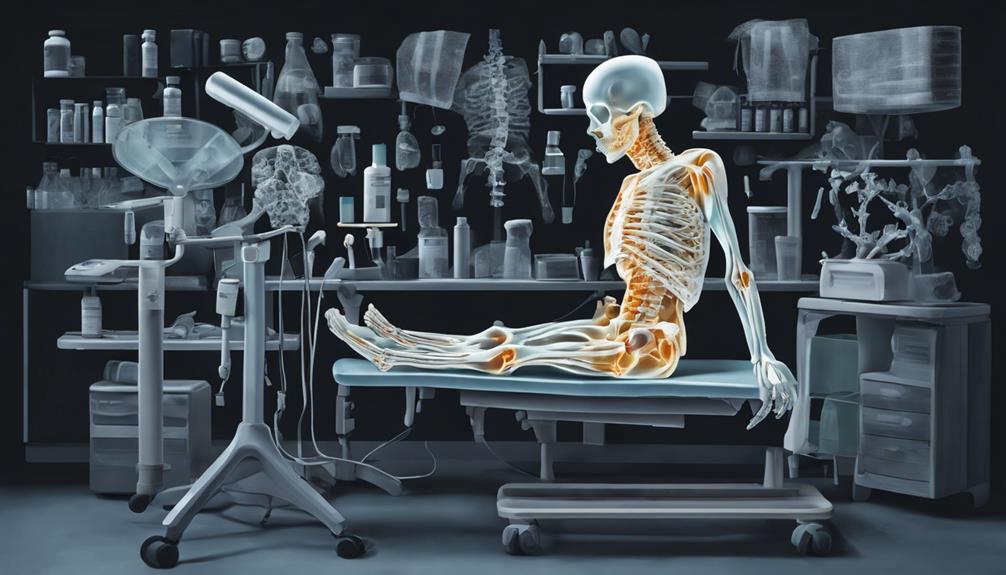
- Diagnosis methods differ: joint x-ray for osteoarthritis, DXA scan for osteoporosis.
- Treatment includes pain management, physical therapy, medications, and personalized plans for both conditions.
Key Differences Between Osteoarthritis and Osteoporosis
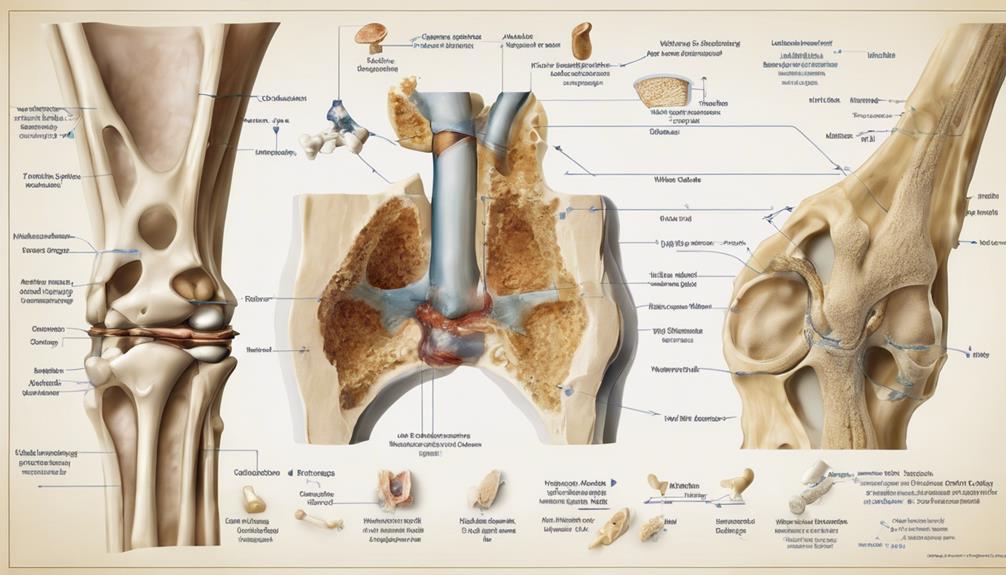
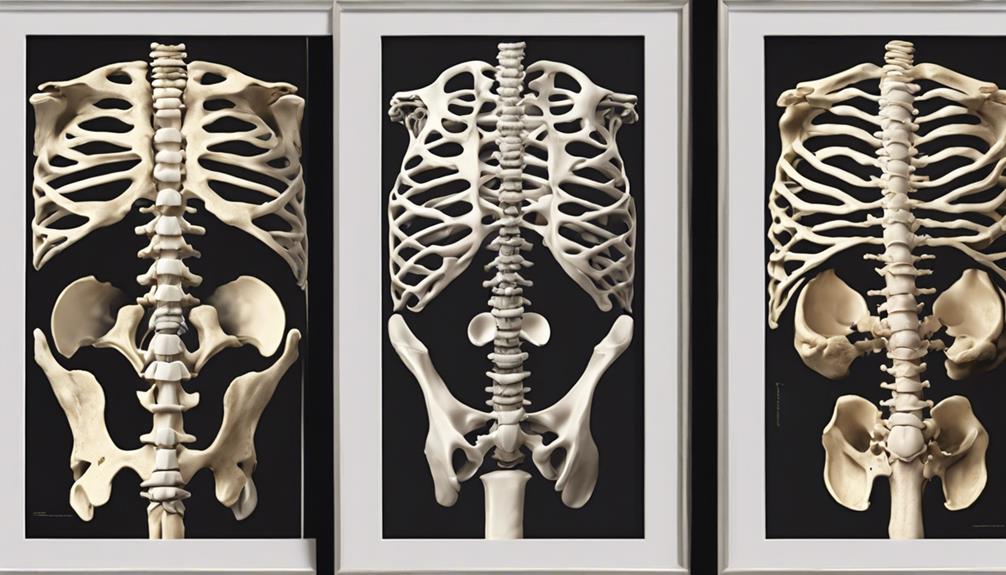
When distinguishing between osteoarthritis and osteoporosis, one crucial difference lies in their primary effects on the body. Osteoarthritis primarily impacts joints, leading to discomfort, stiffness, and decreased range of motion, particularly in weight-bearing joints like knees and hips. On the other hand, osteoporosis weakens bones, increasing the risk of fractures, especially in areas such as the hip, spine, and wrist. Maintaining bone health is vital in both conditions, but the focus shifts towards joint health in osteoarthritis and bone strength in osteoporosis.
Risk factors for osteoarthritis include age, obesity, joint overuse, and genetics, while osteoporosis is influenced by factors such as age, gender (more prevalent in women), family history, and hormonal changes. Physical activity plays a crucial role in managing both conditions. In osteoarthritis, targeted exercises can help improve joint function and reduce pain. For osteoporosis, weight-bearing exercises are essential in maintaining bone density and strength. Understanding these distinctions is key in providing effective care and support for individuals dealing with these conditions.
Causes and Risk Factors
Moving from the discussion on the key differences between osteoarthritis and osteoporosis, it's essential to explore the causes and risk factors associated with these musculoskeletal conditions to understand their implications better.
Osteoarthritis is often linked to joint overuse, family history, inactivity, and excess weight, while osteoporosis is influenced by factors such as low bone mineral density, older age, previous fractures, history of falls, and certain medications.
Women face a higher risk of developing osteoporosis compared to men, highlighting the importance of understanding gender variations in bone health. Genetics, race, and lifestyle choices also play significant roles in determining the likelihood of developing both osteoarthritis and osteoporosis.
Recognizing these specific risk factors is crucial for prevention and the effective management of these conditions, as they directly impact bone loss, joint health, and overall physical well-being. By addressing these risk factors proactively, individuals can take steps to maintain healthier bones and joints for improved long-term physical health.
Symptoms and Progression
Symptoms of osteoarthritis manifest as joint pain and stiffness, impacting daily activities and mobility. The gradual progression of this condition can lead to decreased range of motion and difficulty in performing routine tasks.
The following imagery highlights the challenges individuals may face:
- Morning stiffness in the joints, making it hard to get out of bed.
- Pain worsening with physical activity, limiting the ability to exercise or engage in hobbies.
- Swelling and tenderness around the affected joints, hindering simple movements like grasping objects.
As osteoarthritis affects the bone and joint structures, the risk of disability increases with time. Without proper management, the physical limitations imposed by this condition can significantly impact one's quality of life. Understanding these symptoms and their progression is crucial in seeking timely interventions to alleviate discomfort and maintain functional independence.
Diagnosis Methods

When it comes to diagnosing osteoarthritis, we typically start with a joint x-ray to visualize any joint damage present.
On the other hand, for osteoporosis, a bone density scan, also known as a DXA scan, is crucial in assessing bone strength and density.
Additionally, blood tests may be employed to measure specific markers related to bone health and turnover in osteoporosis cases.
X-Ray for Osteoarthritis
Utilizing X-rays in the diagnostic process of osteoarthritis provides healthcare professionals with crucial insights into joint damage and structural changes indicative of the condition's progression. When analyzing X-ray images for osteoarthritis, we focus on specific features such as:
- Bone Spurs: These bony projections at the joint margins are often visible on X-rays, indicating abnormal bone growth.
- Joint Degeneration: X-rays help identify the extent of joint degeneration, showcasing the severity of osteoarthritis.
- Narrowing of Joint Spaces: X-ray images reveal any narrowing of joint spaces, a common sign of cartilage loss in osteoarthritis.
These details obtained from X-rays play a vital role in diagnosing and monitoring osteoarthritis effectively.
Bone Density Scan
A bone density scan, commonly referred to as a DXA scan, is a fundamental diagnostic tool used to assess osteoporosis by measuring bone mineral density. The scan is a painless procedure that involves minimal radiation exposure, ensuring a safe method to evaluate bone health. Results from this scan are crucial in determining the risk of fractures and guiding treatment decisions for osteoporosis. Focusing on key areas like the hip and spine, where osteoporosis-related fractures are most common, the bone density scan aids in the early detection and monitoring of bone loss. This, in turn, plays a significant role in the prevention and management of osteoporosis.
| Bone Density Scan Facts | |
|---|---|
| Commonly known as | DXA scan |
| Purpose | Diagnose osteoporosis |
| Method | Measure bone mineral density |
Blood Tests for Osteoporosis
Blood tests for osteoporosis serve as supplementary tools in assessing bone health markers, offering valuable insights when combined with imaging tests for a comprehensive diagnosis. While bone density testing, like Dual-energy X-ray absorptiometry (DXA), remains the gold standard for diagnosing osteoporosis, blood tests can provide additional information. These tests may measure levels of calcium, phosphate, alkaline phosphatase, and vitamin D, offering indirect indicators of bone health.
Specifically, a blood test measuring C-terminal telopeptide (CTX) can offer insights into bone resorption rates, aiding in assessing osteoporosis risk. Additionally, evaluating parathyroid hormone (PTH) levels can help understand how calcium and phosphorus regulation influences bone density. When interpreted alongside imaging results, blood tests play a crucial role in a comprehensive osteoporosis evaluation.
Treatment Approaches for Osteoarthritis
When managing osteoarthritis, we focus on several key treatment approaches.
Pain management strategies, such as medications, play a crucial role in alleviating discomfort.
Physical therapy and tailored exercise programs are essential to strengthen the muscles supporting affected joints.
Pain Management Strategies
Utilizing a combination of non-pharmacological interventions, medication options, and sometimes surgical procedures forms the cornerstone of effective pain management strategies for osteoarthritis. When addressing osteoarthritis pain, consider:
- Exercise: Regular physical activity can help improve joint flexibility and strength.
- Weight Management: Maintaining a healthy weight reduces stress on the joints, decreasing pain.
- Medications: Acetaminophen, NSAIDs, and corticosteroid injections are commonly used to alleviate osteoarthritis discomfort.
These interventions, tailored to individual needs, play a crucial role in managing osteoarthritis pain. Customized treatment plans, integrating these approaches, are vital for enhancing the quality of life for individuals with osteoarthritis.
Physical Therapy Options
Physical therapy plays a pivotal role in enhancing joint function, reducing pain, and improving mobility for individuals managing osteoarthritis. Therapeutic exercises aim to strengthen muscles around affected joints, providing better support. Manual therapy techniques like joint mobilization and manipulation can alleviate stiffness and enhance range of motion. Modalities such as heat, ice, ultrasound, or electrical stimulation are utilized to manage pain and inflammation effectively. Below is a helpful table outlining the different components of physical therapy for osteoarthritis:
| Physical Therapy Components | Description |
|---|---|
| Therapeutic Exercises | Strengthen muscles for support |
| Manual Therapy Techniques | Mobilize joints for improved motion |
| Modalities | Manage pain and inflammation |
Surgical Interventions Available
Surgical interventions available for osteoarthritis, such as joint replacement surgeries and arthroscopy, are crucial treatment approaches aimed at improving joint function and alleviating pain in individuals with advanced joint degeneration.
These interventions offer hope for those struggling with osteoarthritis, providing tailored solutions to address the specific needs of each patient. Some surgical options include:
- Joint replacement surgeries: like hip or knee replacements
- Arthroscopy: a minimally invasive procedure to smooth joint surfaces or remove damaged cartilage
- Osteotomy: a surgical realignment of bones to relieve pressure on the affected joint
Each of these procedures plays a vital role in relieving pain, enhancing joint mobility, and ultimately improving the quality of life for individuals battling osteoarthritis.
Treatment Approaches for Osteoporosis

In managing osteoporosis, a combination of lifestyle adjustments, medication regimens, and tailored exercise routines is essential for optimizing bone health and reducing fracture risk. Bisphosphonates like Fosamax and Actonel are commonly prescribed to reduce bone loss and fracture risk. These medications work by slowing down bone breakdown and increasing bone density.
Additionally, engaging in weight-bearing exercises such as walking, dancing, or weightlifting can help strengthen bones and improve bone density. Surgical options like kyphoplasty or vertebroplasty may be considered for severe vertebral fractures to stabilize the spine. It's crucial to have regular follow-up appointments with healthcare providers to monitor bone health, adjust medications as needed, and assess fracture risk.
Lifestyle Modifications and Prevention

Implementing lifestyle modifications and preventive strategies plays a crucial role in reducing the risk of developing osteoporosis and osteoarthritis. To prevent these conditions effectively, consider the following:
- Maintain a Balanced Diet: Consuming foods rich in calcium and vitamin D can support bone health and prevent osteoporosis and osteoarthritis.
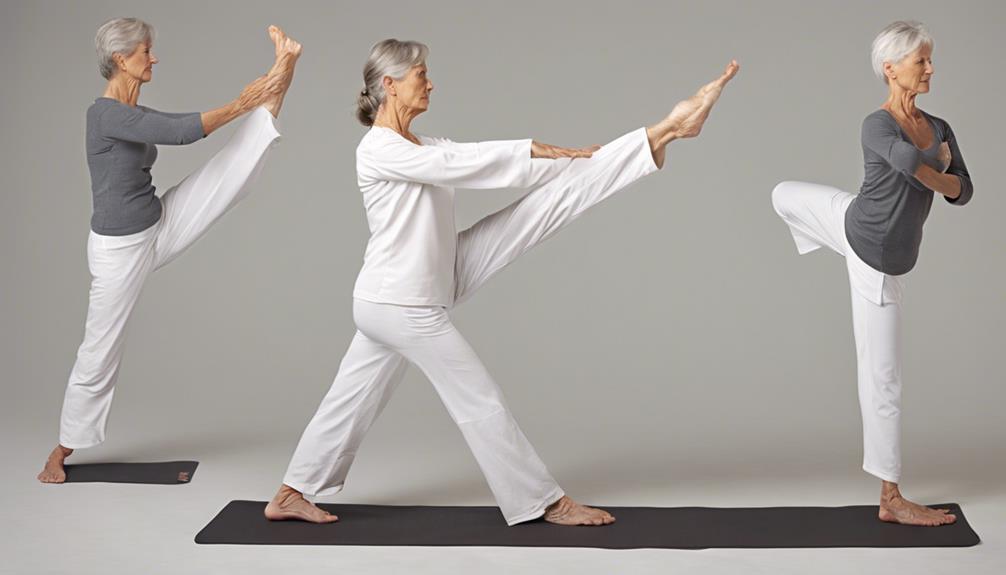
- Engage in Weight-Bearing Exercise: Regular activities like walking or strength training help strengthen bones and joints, improving bone density and reducing the risk of both osteoporosis and osteoarthritis.
- Avoid Harmful Habits: Steering clear of smoking and excessive alcohol consumption can help maintain bone density and joint health, lowering the chances of developing osteoporosis and osteoarthritis.
Managing Both Conditions Simultaneously
To effectively manage both osteoarthritis and osteoporosis simultaneously, individuals must adhere to personalized management plans that address their specific needs and conditions, incorporating tailored exercise programs and joint mobility strategies. When dealing with joint limitations caused by osteoarthritis, exercise modifications become crucial. Specially trained physiotherapists can play a pivotal role in designing safe and effective exercise routines that accommodate the challenges posed by both conditions. By focusing on maintaining joint mobility and bone strength through targeted exercises, individuals can better manage the progression of osteoarthritis and osteoporosis.
A comprehensive management plan is essential for individuals dealing with both osteoarthritis and osteoporosis, ensuring a holistic approach to their care. This plan should include regular monitoring, adjustments to exercise routines based on individual progress, and ongoing support to address any emerging issues. By following a well-rounded strategy that considers the unique needs of each condition, individuals can enhance their quality of life and better cope with the challenges presented by osteoarthritis and osteoporosis.
Resources and Support for Patients

Exploring available resources and support for patients with osteoarthritis and osteoporosis is crucial for comprehensive management of these conditions. When it comes to seeking guidance and assistance, organizations like The Arthritis Society and Osteoporosis Canada are invaluable resources.
Here are some key resources for patients:
- The Arthritis Society: Contact them at 1-800-321-1433 or visit www.arthritis.ca for comprehensive arthritis-related assistance.
- Osteoporosis Canada: Reach out to them through their toll-free line at 1-800-463-6842 for up-to-date information and counseling on osteoporosis.
- Support and Information: Both organizations offer support and information on managing osteoarthritis and osteoporosis, providing valuable insights on joint health, bone mass preservation, and reducing the risk associated with these conditions.
Frequently Asked Questions
What Is the Difference Between Osteoarthritis and Osteoporosis?
When comparing osteoarthritis and osteoporosis, it's crucial to understand their distinct impacts on the body.
Osteoarthritis primarily affects joints, causing pain and stiffness, while osteoporosis weakens bones, increasing fracture risk.
While osteoarthritis targets joints directly, osteoporosis impacts bone density.
These conditions require different management strategies due to their unique effects on the body.
Understanding these differences is vital for proper diagnosis and treatment.
What Are the 4 Stages of Osteoarthritis?
In the four stages of osteoarthritis, progression begins with minor cartilage breakdown, leading to minimal discomfort.
As it advances, joint pain, stiffness, and limited motion become noticeable.
Moderate osteoarthritis brings increased pain, inflammation, and reduced function, while severe cases result in significant joint damage, severe pain, deformity, and limited mobility.
These stages represent a continuum of deterioration that impacts one's quality of life and mobility.
What Are 5 Symptoms of Osteoporosis?
We mightn't notice osteoporosis until a fracture occurs. Symptoms include back pain, height loss, stooped posture, and fractures with minimal trauma.
Lung capacity can decrease, and fractures often affect the hip, spine, and wrist. Interestingly, about 70% of women over 80 have osteoporosis.
These silent symptoms can lead to serious complications, making awareness crucial for prevention and early intervention.
What Is the Treatment for Osteoarthritis?
For osteoarthritis treatment, we employ various strategies. Pain management includes medications, physical therapy, and occupational therapy to enhance joint mobility.
Injections like corticosteroids or hyaluronic acid may alleviate inflammation. Severe cases may require joint replacement surgery.
Lifestyle changes are crucial, such as weight management, exercise, and joint protection techniques. Each approach aims to reduce discomfort, improve function, and enhance overall quality of life for individuals with osteoarthritis.
Conclusion
In conclusion, managing osteoarthritis and osteoporosis requires a multifaceted approach tailored to individual needs. As the saying goes, 'prevention is better than cure.'
By staying proactive with lifestyle modifications, regular screenings, and adherence to treatment plans, we can strive to maintain our bone health and joint function. Remember, taking small steps now can lead to significant improvements in the long run.
Stay informed, stay active, and prioritize your musculoskeletal health.