Have you ever considered that bones serve a greater purpose than just existing? Think again.
Osteoporosis specialists are the unsung heroes of bone health, dedicated to unraveling the mysteries of brittle bones and fractures.
But what exactly sets these specialists apart in the realm of healthcare?
Let's explore the pivotal role they play in transforming the landscape of osteoporosis management and discover the innovative strategies they employ to safeguard bone strength and resilience.
Key Takeaways
- Specialists diagnose osteoporosis using DEXA scans.
- Tailored treatment plans based on bone density tests are crucial.
- Regular consultations and early intervention are vital for proactive management.
- Osteoporosis specialists play a pivotal role in enhancing bone health outcomes.
Understanding Osteoporosis Specialists
When it comes to understanding osteoporosis specialists, it's essential to recognize their pivotal role in diagnosing and treating bone health issues. One crucial tool in their diagnostic arsenal is the bone density test. This test measures the strength and mineral density of your bones, helping specialists assess your risk of fractures and determine the presence of osteoporosis. By analyzing the results of a bone density test, osteoporosis specialists can tailor a personalized treatment plan to improve your bone health.
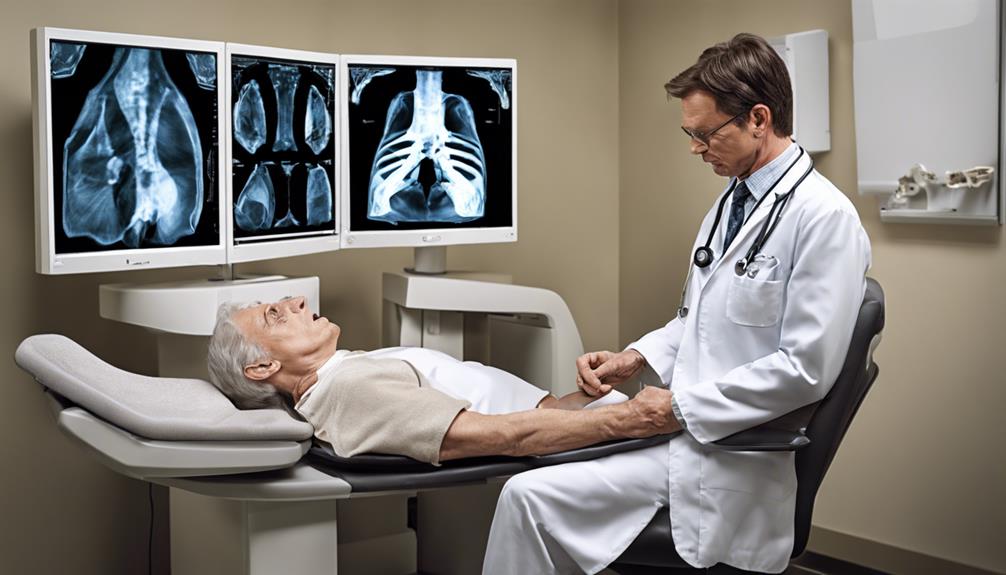
During a bone density test, you may be asked to lie on a padded table while a scanning machine passes over your body, measuring bone density in areas like the hip, spine, or forearm. The results provide valuable information that guides specialists in recommending lifestyle changes, medications, and monitoring to enhance your bone strength and reduce fracture risk.
Regular consultations with an osteoporosis specialist, who interprets the results of your bone density test, are essential for proactive bone health management and preventing debilitating fractures.
Importance of Osteoporosis Diagnosis
Understanding the importance of diagnosing osteoporosis early is crucial for preventing fractures and improving overall bone health. One of the key methods for diagnosing osteoporosis accurately is through bone density tests, such as DEXA scans. These tests measure the mineral content and density of bones, helping healthcare providers assess the strength and quality of the bones. Timely diagnosis based on these tests allows for early intervention and treatment to prevent further bone loss and reduce the risk of fractures. Those with risk factors, such as older adults, postmenopausal women, and individuals with a family history of osteoporosis, should prioritize osteoporosis screening to evaluate their bone health. Recognizing the significance of osteoporosis diagnosis can lead to better management strategies, improved quality of life, and a proactive approach to maintaining strong and healthy bones.
| Importance of Osteoporosis Diagnosis |
|---|
| Prevents fractures and improves bone health |
| Utilizes bone density tests like DEXA scans |
| Allows for early intervention and treatment |
| Prioritizes screening for at-risk individuals |
Role of Osteoporosis Specialists
Osteoporosis specialists, skilled in diagnosing and treating bone health concerns, offer personalized care plans tailored to individual needs. These specialists assess bone density through scans, enabling them to create targeted strategies to manage osteoporosis effectively. By evaluating risk factors and medical history, osteoporosis specialists develop comprehensive approaches that may include lifestyle adjustments, medications, and preventive measures.
Our role extends beyond treating osteoporosis; we educate patients on the importance of bone health and how it impacts overall well-being. Through open communication and detailed explanations, we help individuals understand the significance of maintaining strong bones to prevent fractures and maintain mobility.
With a focus on compassionate care, osteoporosis specialists empower patients to take control of their bone health journey. By emphasizing the value of early detection and proactive management, we strive to enhance the quality of life for those affected by osteoporosis.
Osteoporosis Risk Factors
As we address the topic of osteoporosis risk factors, it's crucial to understand that factors like age and gender play a significant role in determining one's susceptibility to this condition.
Additionally, having a family history of osteoporosis can heighten the risk of developing the disease.
These risk factors emphasize the importance of proactive measures and regular screenings to maintain bone health and prevent potential fractures.
Age and Gender
With advancing age, both men and women face an increased risk of developing osteoporosis, but postmenopausal women, in particular, are more susceptible to bone density loss. As we age, our bone mass naturally decreases, leading to a higher likelihood of developing osteoporosis. Women over 50, especially after menopause, are at a higher risk due to hormonal changes that accelerate bone loss.
Men also experience age-related bone loss, but typically at a slower rate than women. It's crucial to understand how age and gender impact bone health to take proactive steps in preventing osteoporosis. Regular screenings, a balanced diet rich in calcium and vitamin D, weight-bearing exercises, and avoiding smoking and excessive alcohol consumption are essential in maintaining bone strength and reducing the risk of fractures.
Family History
Our family's medical history often serves as a guiding light, illuminating potential health risks that we, too, may inherit. Understanding our family history is crucial when considering osteoporosis risk factors. Here are key points to consider regarding family history:
- Increased Risk: Having a family history of osteoporosis raises the likelihood of developing the condition.
- Parental Hip Fracture: Individuals with a parental hip fracture are at a higher risk of osteoporosis.
- Genetic Predisposition: Genetic factors significantly influence the risk of osteoporosis.
- Preventive Measures: Knowledge of family history enables early detection and preventive actions, such as regular screenings and lifestyle adjustments.
Being aware of our family's medical background empowers us to take proactive steps in managing our bone health and preventing osteoporosis.
Treatment Options for Osteoporosis

When addressing osteoporosis treatment options, we focus on a multifaceted approach.
Medications such as alendronate and risedronate are commonly prescribed to strengthen bones, complemented by lifestyle modifications and dietary adjustments rich in calcium and vitamin D.
Additionally, weight-bearing exercises like walking and stationary biking play a crucial role in improving bone health and reducing the risk of fractures.
Medication for Osteoporosis
Medications for osteoporosis play a crucial role in preventing bone loss and strengthening bones, offering various treatment options tailored to individual needs. When considering medication for osteoporosis, it's essential to understand the options available. Here are some common medications used to treat osteoporosis and improve bone density:
- Bisphosphonates: Such as alendronate and risedronate, help prevent bone loss by inhibiting bone breakdown.
- Selective Estrogen Receptor Modulators (SERMs): Like raloxifene, can increase bone density and reduce fracture risk in postmenopausal women.
- Teriparatide: A parathyroid hormone that stimulates new bone formation, often prescribed for severe osteoporosis cases.
- Denosumab: Inhibits bone breakdown and is administered through injections every six months, aiding in bone density maintenance.
Lifestyle Changes
To effectively address osteoporosis, implementing lifestyle changes is imperative, as they play a pivotal role in improving bone health and reducing the risk of fractures. Regular weight-bearing exercises such as walking, jogging, and dancing are beneficial for increasing bone density. Adequate calcium and vitamin D intake, either through diet or supplements, are crucial for maintaining bone strength and preventing osteoporosis.
Avoiding smoking and excessive alcohol consumption can also help decrease the risk of fractures. Additionally, maintaining a healthy body weight and proper nutrition supports bone health. Engaging in balance and strength training exercises further enhances stability, reducing the likelihood of falls that can lead to fractures in individuals with osteoporosis.
Exercise Recommendations
Regularly engaging in a variety of exercises tailored to your needs and preferences is essential for managing osteoporosis and improving bone health. Here are some exercise recommendations to help enhance bone density and overall well-being:
- Weight-Bearing Exercises: Activities like walking, dancing, and hiking strengthen bones, reducing the risk of fractures.
- Resistance Training: Using weights or resistance bands improves bone density and muscle strength.
- Balance Exercises: Practices like tai chi and yoga enhance stability, reducing the likelihood of falls and fractures.
- Aerobic Activities: Engaging in regular aerobic exercises like swimming or cycling boosts overall health.
Remember to consult with a healthcare provider or physical therapist to create a personalized exercise plan that considers your specific needs and limitations related to osteoporosis.
Diagnostic Tests for Osteoporosis

When it comes to diagnosing osteoporosis, the gold standard test is a bone density scan, also known as a DEXA scan. This test measures bone mineral density using low levels of radiation to assess bone strength and the risk for fractures. DEXA scans provide results in the form of T-scores, which compare bone density to that of a young adult. Detecting osteoporosis early through DEXA scans is crucial as it allows for timely intervention and management. In addition to DEXA scans, other diagnostic tests for osteoporosis include ultrasound measurements of the heel and quantitative computed tomography (QCT) scans.
| Diagnostic Test | Methodology | Benefits |
|---|---|---|
| DEXA Scan (Bone Density) | Measures bone mineral density using low radiation | Gold standard for osteoporosis diagnosis |
| Heel Ultrasound | Assesses bone density in the heel bone | Portable and non-invasive test |
| QCT Scan | Provides detailed 3D images of bone density | Useful for assessing spine strength |
Lifestyle Changes for Osteoporosis

Exploring lifestyle changes for osteoporosis management reveals crucial steps individuals can take to strengthen their bones and reduce fracture risk. To improve bone health, consider the following recommendations:
- Regular Weight-Bearing Exercises: Engage in activities like walking, jogging, or dancing to enhance bone strength and lower the risk of osteoporosis.
- Adequate Calcium and Vitamin D Intake: Ensure you consume enough calcium and vitamin D either through your diet or supplements to support optimal bone health.
- Avoid Smoking and Excessive Alcohol: By steering clear of smoking and limiting alcohol intake, you can prevent bone loss and reduce the chances of fractures.
- Balance and Strength Training: Incorporate exercises that focus on balance and strength to enhance stability, reducing the likelihood of falls and fractures.
Medications for Osteoporosis

As we discuss medications for osteoporosis, it's crucial to understand the common drugs available, potential side effects, and recommended treatment durations.
Each medication, from bisphosphonates to teriparatide, plays a specific role in strengthening bones and reducing fracture risk.
Being well-informed about these aspects can empower individuals to make informed decisions in managing their osteoporosis effectively.
Common Osteoporosis Drugs
Numerous medications are available to treat osteoporosis, each with specific mechanisms of action to help prevent bone loss and reduce fracture risk. These medications include:
- Bisphosphonates: Alendronate and risedronate are examples that help prevent bone loss by inhibiting bone breakdown.
- Calcitonin: This medication regulates calcium levels and can be administered through a nasal spray or injection to aid in managing bone loss.
- Selective estrogen receptor modulators (SERMs): Raloxifene mimics estrogen's bone-protective effects, especially in postmenopausal women with osteoporosis.
- Teriparatide: Used in severe cases, teriparatide stimulates new bone formation, aiming to address bone loss effectively.
These drugs play vital roles in managing osteoporosis and reducing the risk of fractures, contributing to improved bone health and overall well-being.
Side Effects Overview
When considering osteoporosis medications, it's crucial to be aware of the potential side effects that can accompany these treatments, affecting various aspects of the body's functioning and requiring careful monitoring. Some common side effects of these medications include gastrointestinal issues such as nausea and stomach upset, as well as muscle or joint pain. Specific drugs like bisphosphonates may rarely lead to osteonecrosis of the jaw, while hormone therapy can increase the risk of blood clots or breast cancer.
Injectable osteoporosis medications might cause injection site reactions like redness or swelling. Monitoring bone density and discussing any concerning symptoms with healthcare providers are essential to managing these side effects effectively and ensuring the best possible outcomes for patients.
Treatment Duration Guidelines
Discussing the appropriate duration for osteoporosis medication treatment involves considering individual response, fracture risk, and regular monitoring by healthcare providers. When determining treatment duration, factors such as bone mass and fracture risk play a crucial role. Here are some guidelines to consider:
- Medication Type: Different medications may have varying recommended durations of use.
- Individual Response: Response to treatment can vary, influencing how long medication should be continued.
- Fracture Risk: The level of risk for fractures helps determine the appropriate duration of treatment.
- Regular Monitoring: Healthcare providers monitor bone mass changes and adjust treatment duration as needed.
Nutritional Recommendations for Osteoporosis

Ensuring adequate intake of essential nutrients like calcium and vitamin D is crucial for supporting bone health and preventing osteoporosis. Calcium is a key mineral that contributes to bone density, and daily recommendations vary based on age and gender. Vitamin D is essential for calcium absorption and bone strength, with deficiency increasing the risk of osteoporosis. Including foods rich in calcium such as dairy products, leafy greens, almonds, and fortified foods in your diet can help meet daily requirements. Additionally, magnesium, vitamin K, and phosphorus are also important for bone health and should be part of a balanced diet to support bone density. To maintain optimal bone health and reduce the risk of osteoporosis, it is advisable to limit consumption of caffeine, soda, excessive salt, and alcohol.
| Nutrients | Food Sources |
|---|---|
| Calcium | Dairy products, leafy greens |
| Vitamin D | Fatty fish, egg yolks |
| Magnesium | Nuts, seeds, whole grains |
| Vitamin K | Kale, spinach, broccoli |
Exercise Guidelines for Osteoporosis

To effectively manage osteoporosis and promote bone health, incorporating tailored exercise guidelines into your routine is essential. Here are some guidelines to help improve bone density and overall bone health:
- Weight-Bearing Exercises: Activities like walking, jogging, and dancing are beneficial as they help strengthen bones and reduce the risk of fractures in individuals with osteoporosis.
- Resistance Training: Incorporating weight lifting or resistance band exercises into your routine can improve bone density and muscle strength, contributing to better bone health over time.
- Balance Exercises: Engaging in activities such as yoga and tai chi can enhance stability and coordination, reducing the risk of falls and fractures in individuals with osteoporosis.
- Low-Impact Activities: Swimming and cycling are excellent options for cardiovascular benefits without exerting excessive strain on the bones, making them suitable for those with osteoporosis.
Surgical Interventions for Osteoporosis

When managing severe cases of osteoporosis with multiple fractures or spinal deformities, surgical interventions become a crucial consideration. In such situations, procedures like vertebroplasty and kyphoplasty play a vital role in stabilizing vertebral fractures, reducing pain, and improving bone density. Additionally, spinal fusion surgery may be recommended to enhance spinal alignment and stability in advanced osteoporosis cases. These surgical treatments aim to alleviate pain, restore function, and prevent further bone deterioration in patients with osteoporosis.
To provide a clearer picture, let's look at a comparison table outlining some common surgical interventions for osteoporosis:
| Surgical Intervention | Purpose |
|---|---|
| Vertebroplasty | Stabilize vertebral fractures |
| Kyphoplasty | Reduce pain and improve bone density |
| Spinal Fusion Surgery | Enhance spinal alignment and stability |
| Osteotomy | Correct deformities and improve bone density |
Follow-Up Care With Osteoporosis Specialists

Working closely with osteoporosis specialists for follow-up care is essential in maintaining optimal bone health and preventing fractures. These specialists provide personalized treatment plans tailored to individual risk factors and bone density assessments.
Here are four key aspects of follow-up care with osteoporosis specialists:
- Medication Management: Osteoporosis specialists oversee the effectiveness of prescribed medications and make adjustments as needed to ensure the best outcomes for bone health.
- Lifestyle Modifications: They offer guidance on lifestyle changes such as exercise routines, dietary adjustments, and fall prevention strategies to support bone strength and reduce fracture risks.
- Monitoring Bone Density Changes: Regular assessments of bone density help track progress and determine the effectiveness of treatments, allowing for timely interventions if needed.
- Educating Patients: Osteoporosis specialists emphasize the importance of adhering to treatment plans and attending follow-up appointments for continued support in maintaining bone health and overall well-being.
Osteoporosis Management Strategies

Implementing comprehensive osteoporosis management strategies involves integrating a balanced diet, weight-bearing exercises, and appropriate medications to support bone health and reduce fracture risks. A diet rich in calcium and vitamin D is essential for maintaining strong bones. Weight-bearing exercises such as walking, jogging, and resistance training help improve bone density and reduce the chances of fractures.
Medications like alendronate and risedronate are commonly prescribed to prevent bone loss and enhance bone strength in individuals with osteoporosis. Fall prevention measures, like decluttering living spaces and ensuring good lighting, play a crucial role in osteoporosis management by reducing the risk of falls and subsequent fractures.
Regular screenings to monitor bone density levels and consistent follow-up appointments with an osteoporosis specialist are important for assessing progress and adjusting treatment plans accordingly. By focusing on these strategies, we can work towards better bone health and overall well-being for individuals dealing with osteoporosis.
Osteoporosis Research and Innovations

We're excited to share the latest advancements in osteoporosis treatment, including promising research findings and technological breakthroughs.
Our focus is on improving bone density, preventing fractures, and assessing bone quality through cutting-edge imaging techniques.
Latest Treatment Advancements
Recent advancements in osteoporosis treatment are revolutionizing the way we approach bone health and fracture prevention.
- Medications: New drugs aim to strengthen bones and lower fracture risk.
- Targeted Therapies: Innovative treatments address specific bone density concerns.
- Imaging Techniques: Advanced scans help detect changes in bone density early in osteoporosis patients.
- Exercise Studies: Research delves into the effects of exercise on bone health and fracture prevention in individuals with osteoporosis.
These developments offer hope for improved outcomes in managing osteoporosis and enhancing bone strength.
As specialists, we strive to integrate these cutting-edge treatments into personalized care plans, ensuring our patients receive the best possible support for their bone health needs.
Promising Research Findings
In the realm of osteoporosis research and innovations, we uncover promising findings that hold potential for transforming bone health outcomes. Recent studies have revealed new drug therapies targeting specific pathways to enhance bone density in osteoporosis patients. Innovations in bone imaging technology, including high-resolution CT scans and MRI techniques, offer more precise assessments of bone health. Combining medications with lifestyle changes like exercise and dietary adjustments has shown promising results in managing osteoporosis. Ongoing clinical trials are investigating the effectiveness of novel treatments such as sclerostin inhibitors and Wnt pathway modulators in preventing bone loss. Personalized medicine approaches tailored to individual genetic factors and disease progression are also being explored to improve bone density outcomes.
| Research Findings | Impact on Bone Density |
|---|---|
| New drug therapies | Enhance bone density |
| Advanced bone imaging technology | Provide accurate assessments |
| Combined medication and lifestyle interventions | Improve osteoporosis management |
| Novel treatments in clinical trials | Potential for preventing bone loss |
Technological Breakthroughs in Osteoporosis
Technological advancements in the field of osteoporosis are revolutionizing bone health assessment and treatment options for patients. These breakthroughs include:
- Advanced imaging techniques such as high-resolution peripheral quantitative computed tomography (HR-pQCT) that assess bone microarchitecture, providing detailed insights into bone density.
- Development of new bone turnover markers for more precise monitoring of bone health, crucial in managing osteoporosis effectively.
- Virtual bone biopsies using microindentation offer valuable information on bone strength and quality, aiding in the diagnosis and treatment of osteoporosis.
- Utilization of 3D printing technology to create personalized implants for orthopedic surgeries in patients with severe osteoporosis-related fractures, enhancing treatment outcomes and recovery.
Finding an Osteoporosis Specialist

When looking to find an osteoporosis specialist, consider seeking recommendations from your primary care physician or consulting with a local hospital's referral service. These specialists are doctors with specialized training in diagnosing and treating bone health conditions like osteoporosis. They utilize advanced diagnostic tools such as bone density scans to assess bone health accurately.
By consulting with an osteoporosis specialist, individuals can receive personalized treatment plans aimed at managing and preventing fractures, ultimately improving outcomes and quality of life. These specialists prioritize the well-being of their patients and work diligently to address their specific bone health needs. Seeking care from an osteoporosis specialist can make a significant difference in managing this condition effectively.
If you or a loved one are concerned about bone health or have been diagnosed with osteoporosis, reaching out to an osteoporosis specialist is a proactive step towards better bone health management. Their expertise and focus on bone density-related issues can provide valuable support and guidance in your journey towards improved bone health.
Frequently Asked Questions
What Is the Best Doctor to See for Osteoporosis?
When looking for the best doctor to manage osteoporosis, specialists like endocrinologists or rheumatologists are ideal choices. Endocrinologists focus on hormone-related bone health issues, while rheumatologists specialize in musculoskeletal conditions, including osteoporosis. These experts can conduct detailed assessments, order bone density scans, and create personalized treatment plans.
Seeking care from such specialists ensures access to the latest treatments and comprehensive approaches to managing osteoporosis effectively.
What Will an Endocrinologist Do for Osteoporosis?
To tackle osteoporosis, an endocrinologist will assess hormone levels, order bone density tests like DEXA scans, and create tailored treatment plans. They prescribe medications to prevent bone loss, reduce fracture risk, and enhance bone density.
What Does a Rheumatologist Do for Osteoporosis?
When managing osteoporosis, we rheumatologists assess bone density, evaluate fracture risk, and develop personalized treatment plans. Our focus is on medication, lifestyle adjustments, and prevention of complications like fractures.
Monitoring and adjusting treatment plans are key to improving bone health and enhancing quality of life for osteoporosis patients. We play a vital role in addressing underlying factors contributing to bone loss and ensuring effective management of this condition.
What Is the Very Best Treatment for Osteoporosis?
The very best treatment for osteoporosis involves a comprehensive approach that combines lifestyle adjustments, medication, and regular monitoring.
Key components include calcium, vitamin D supplements, and medications like bisphosphonates, denosumab, and teriparatide.
Engaging in weight-bearing exercises, balance training, and fall prevention strategies are crucial for managing osteoporosis effectively.
It's essential to have regular follow-up appointments to evaluate treatment progress and make necessary adjustments to the plan.
Conclusion
In conclusion, working with an osteoporosis specialist can be a game-changer in managing this condition. They're like skilled architects, building a strong foundation for our bones and guiding us towards better bone health.
With their expertise, compassion, and dedication, they help us navigate the complexities of osteoporosis, ensuring we receive the best care possible. Trusting in their knowledge and guidance can lead to a brighter, stronger future for those living with this condition.