Practical Support
Ask the Techspert: How to Cut the Cord? – Senior Planet From AARP
Kickstart your journey to cutting the cord and discover how to save money while enjoying tailored viewing options—your new entertainment awaits!

Cutting the cord can save you over $70 a month while providing a more personalized viewing experience. Start by evaluating your viewing habits to identify essential shows and channels. You'll need a reliable internet connection, at least 25 Mbps, and a smart TV or streaming device like Roku or Fire Stick. Consider using an indoor HD antenna for local channels. Compare streaming services to find bundles that fit your needs. Don't forget to tap into community resources for support and tips. There's plenty more insight available to help you make informed choices and enhance your streaming experience.
Key Takeaways
- Assess your viewing habits to identify essential shows and channels before selecting streaming services.
- Ensure a reliable internet connection of at least 25 Mbps for smooth streaming experiences.
- Use a smart TV or streaming device, and consider an indoor HD antenna for local channels.
- Research and compare streaming service options, including bundle deals to maximize content access and savings.
- Engage with community resources and groups to share experiences and gain tips on cutting the cord.
Benefits of Cutting the Cord
Cutting the cord can lead to significant savings and a more tailored viewing experience. You might be tired of paying over $200 a month for cable when you only watch a few channels.
With streaming services, you pay only for what you use, and you can cancel anytime without hassle. You'll enjoy fewer ads and gain access to exclusive original content, along with a vast library of on-demand options that enhance your viewing flexibility. Additionally, similar to how Bitcoin mining operates on a decentralized network, streaming services offer you the freedom to choose content without being tied to traditional cable providers. Just like using energy-efficient technology in heat pumps can reduce costs, cutting cable can also significantly lower your monthly expenses. Moreover, by evaluating your financial health, you can ensure that your spending aligns with your budget plan and helps you save more effectively. Research shows that many people experience increased satisfaction with their viewing choices after making the switch to streaming.
You could save over $70 monthly by ditching cable. Just be mindful not to subscribe to multiple services for specific shows; limit yourself to two streaming platforms for cost efficiency.
Analyze your viewing habits to maximize savings and increase your access to content you love. Furthermore, cutting the cord allows you to enjoy exclusive original content that enhances your overall viewing experience.
Essential Equipment for Streaming

To enjoy a seamless streaming experience, you'll need some essential equipment. First, make sure you have a reliable internet connection with at least 25 Mbps for smooth streaming, especially in 4K. AI technology can significantly enhance cybersecurity measures for your connected devices, ensuring a safer streaming environment.
Next, invest in a smart TV or a streaming device like a Roku, Fire Stick, or Chromecast to access your favorite services. If you want local channels, consider an indoor HD antenna; these can deliver high-definition signals. Additionally, having a home security system can enhance your overall home setup and peace of mind while streaming. A good choice for peace of mind is a top home security system that integrates with your smart home devices. For added comfort, consider using an air purifier to maintain clean air while you enjoy your streaming sessions.
You can connect multiple TVs to a single antenna using coaxial cables and splitters, but remember that the quality of these components affects signal strength. Retailers like Amazon and Walmart offer various antenna options, some of which are plug-and-play for easy installation. Additionally, having a reliable internet connection is crucial for optimal usage of streaming devices and services.
Get equipped, and you're set to start streaming!
Choosing Streaming Services

Selecting the right streaming services can greatly enhance your viewing experience. Start by evaluating your viewing habits and preferences.
Consider which shows and channels are must-haves for your household. Here are some tips to help you choose wisely:
- Create a list of essential programs for everyone in your home.
- Compare services based on your list and check for content availability.
- Look for bundle options that can save you money while providing diverse content. Additionally, many services are now utilizing machine learning to enhance user recommendations, making it easier to discover new shows based on your viewing history. This approach is similar to how predictive analytics helps businesses tailor their offerings by analyzing customer behavior patterns.
Accessing Local Channels

Accessing local channels is a crucial aspect of your cord-cutting journey, guaranteeing you don't miss out on news, sports, and favorite shows. You can easily access these channels through an indoor HD antenna or by using a streaming service that includes local programming. Here's a quick comparison to help you decide:
| Method | Pros |
|---|---|
| Indoor HD Antenna | Free local channels |
| Streaming Services | On-demand and live options |
| Outdoor Antenna | Better signal in rural areas |
| Cable Alternatives | Bundled local and premium channels |
| Smart TVs | Built-in apps for easy access |
Choosing the right method can enhance your viewing experience while keeping costs down. Evaluate your setup to guarantee you get the best local content!
Community Resources and Support

Finding local channels is just the beginning of your cord-cutting journey. As you navigate this shift, community resources can offer essential support. Connecting with others who've made the leap can help you avoid common pitfalls and discover new options.
Here are some ways to engage:
- Join local groups or forums focused on cord-cutting discussions.
- Follow newsletters from organizations like Senior Planet for updates and tips.
- Attend community events or workshops that cover technology and streaming services. Engaging in these events can foster a sense of community among those transitioning to new viewing habits. Additionally, sharing experiences can lead to enhanced productivity as you adapt to new technologies and routines.
These resources not only provide information but also foster connections with fellow cord-cutters. Embrace community support to enhance your experience and make informed choices as you explore the world of streaming and local channels. Additionally, understanding air quality concerns can be vital to creating a comfortable home environment while you enjoy your new streaming services.
Engaging in Technology Classes

Technology classes are a fantastic way to build your confidence and skills as you shift to streaming services. These courses cover essential topics, from setting up your smart TV to steering through various streaming platforms. By participating, you'll gain hands-on experience, making it easier to understand how to access your favorite shows and movies. Classes often include step-by-step instructions and troubleshooting tips, ensuring you're well-equipped to tackle any challenges. Additionally, you'll discover the importance of user engagement in optimizing your viewing habits through various platforms.
Furthermore, just like how large plants require specific care, ensuring you have the right equipment and knowledge can significantly enhance your streaming experience. Emotional alignment can also play a role in your enjoyment and satisfaction with the content you choose. Plus, you can connect with fellow learners, sharing insights and solutions as you set out on this cord-cutting journey together. Don't hesitate to explore options available through organizations like Senior Planet, which offer a range of tech workshops tailored to your needs. Additionally, many of these classes incorporate SEO-focused techniques that can help you discover new streaming content based on trending keywords and popular shows.
Moreover, understanding financial considerations for services like assisted living can help you budget effectively as you transition to streaming. Embrace learning and enhance your streaming experience!
Maintaining Health and Wellness

As you embrace the shift to streaming services, maintaining your health and wellness becomes equally important.
Finding balance in your daily routine will help you enjoy your new entertainment options without neglecting your well-being.
Consider incorporating these practices into your lifestyle:
- Stay Active: Engage in regular exercise, whether it's a brisk walk, yoga, or online fitness classes. For a fun option, try hula hooping to increase your cardiovascular fitness while having a good time. Additionally, regular physical activity can promote mobility and reduce feelings of isolation, while also helping to enhance self-awareness through mindfulness practices.
- Mind Your Diet: Prepare nutritious meals while watching your favorite shows, making healthy eating a habit.
- Connect Socially: Join virtual classes or community groups to foster connections and support your mental health.
- Incorporate Outdoor Activities: Spend time outdoors with your dogs to enhance both physical activity and socialization opportunities.
Frequently Asked Questions
How Can I Troubleshoot Streaming Issues on My Device?
To troubleshoot streaming issues, check your internet connection, restart your device, and update apps. If problems persist, clear the cache or reinstall the app. Verify your device meets the minimum speed requirements for seamless streaming.
What Should I Do if My Internet Connection Is Unstable?
If your internet's acting like a dial-up connection, check your router placement first. Restart it, and if that doesn't help, contact your provider to resolve any outages or upgrade your plan for better stability.
Are There Parental Controls Available on Streaming Services?
Yes, most streaming services offer parental controls. You can set restrictions based on content ratings, create profiles for kids, and monitor their viewing habits, ensuring a safe and age-appropriate experience for your family.
Can I Watch Sports Without a Cable Subscription?
Yes, you can watch sports without a cable subscription! Many streaming services offer live sports channels. Just guarantee you subscribe to the right services and check for local games available via an HD antenna.
How Can I Find User Reviews for Streaming Devices?
To find user reviews for streaming devices, check online retailers, tech forums, and dedicated review sites. You'll uncover real experiences and tips, helping you choose the best device for your streaming needs.
Conclusion
Cutting the cord is like shedding a heavy winter coat, freeing you to explore a vibrant world of streaming possibilities. With a bit of guidance, you'll navigate this journey effortlessly, discovering tailored content that warms your heart and sparks joy. Embrace the flexibility and savings, and watch your viewing experience blossom like a garden in spring. Remember, you're not alone; community resources and classes are here to support you, guiding you toward a brighter, more enjoyable entertainment landscape.
Albert brings a wealth of knowledge and expertise to our writing team. With a background in caregiving and a deep understanding of the challenges faced by caregivers, Albert’s writing resonates with authenticity and empathy. He is committed to delivering high-quality content that empowers and supports caregivers on their journey.
Osteoporosis Care
What Can a Specialist for Osteoporosis Do for You?
Leverage the expertise of a Specialist for Osteoporosis to enhance your bone health journey and reduce fracture risks.
When it comes to healthcare, it is typical to find specialists for different conditions. If you are facing osteoporosis, consulting with an Osteoporosis Specialist can greatly improve your journey toward better bone health.
From understanding the intricacies of bone density to tailoring personalized treatment plans, these experts play a crucial role in enhancing bone strength and reducing fracture risks.
But what are the specific qualifications and expertise that differentiate them in this field? Let's explore the nuances of these specialists and how they contribute to managing osteoporosis effectively.
Key Takeaways
- Rheumatologists and endocrinologists interpret bone density test results.
- Gynecologists focus on women's health related to osteoporosis.
- Primary care providers conduct screenings and treatments for osteoporosis.
- Collaboration with specialists is crucial for personalized osteoporosis treatment plans.
Types of Specialists for Osteoporosis
When seeking specialized care for osteoporosis, individuals may consult various types of specialists, including rheumatologists, endocrinologists, geriatricians, gynecologists, and orthopedic surgeons.
Rheumatologists play a crucial role in the management of osteoporosis as they specialize in bone, joint, and muscle disorders, making them well-equipped to diagnose and treat osteoporosis effectively.
Endocrinologists, on the other hand, focus on hormonal imbalances that contribute to osteoporosis, offering targeted treatment options to address these underlying issues.
Geriatricians bring expertise in managing osteoporosis in older adults, considering age-related factors and tailoring care plans to meet the specific needs of this demographic.
Gynecologists specialize in addressing osteoporosis concerns in women, especially those related to menopause and hormonal changes that can impact bone health.
While orthopedic surgeons may not be the first line of defense in osteoporosis treatment, they're crucial in managing fractures and other bone-related issues that may arise due to this condition.
Each specialist brings a unique perspective and skill set to the comprehensive care of individuals with osteoporosis.
Roles of Healthcare Providers

Specialized healthcare providers, such as rheumatologists, endocrinologists, geriatricians, and gynecologists, play distinct roles in the comprehensive management of osteoporosis, each contributing expertise tailored to specific aspects of the condition.
- Bone Density Test: Rheumatologists and endocrinologists are skilled in interpreting bone density test results to assess bone health and diagnose osteoporosis accurately.
- Risk Factors: Geriatricians focus on identifying individual risk factors, such as advanced age or certain medications, that predispose patients to osteoporosis.
- Prevent Bone Loss: Gynecologists work with women to implement preventive strategies, like hormone therapy or lifestyle modifications, to prevent bone loss associated with menopause.
These specialists collaborate with primary care providers who conduct osteoporosis screenings, initiate treatments, and coordinate care plans. By leveraging their unique expertise and focusing on specific aspects of osteoporosis management, these healthcare providers ensure that patients receive comprehensive care tailored to their individual needs, family history, and lifestyle factors.
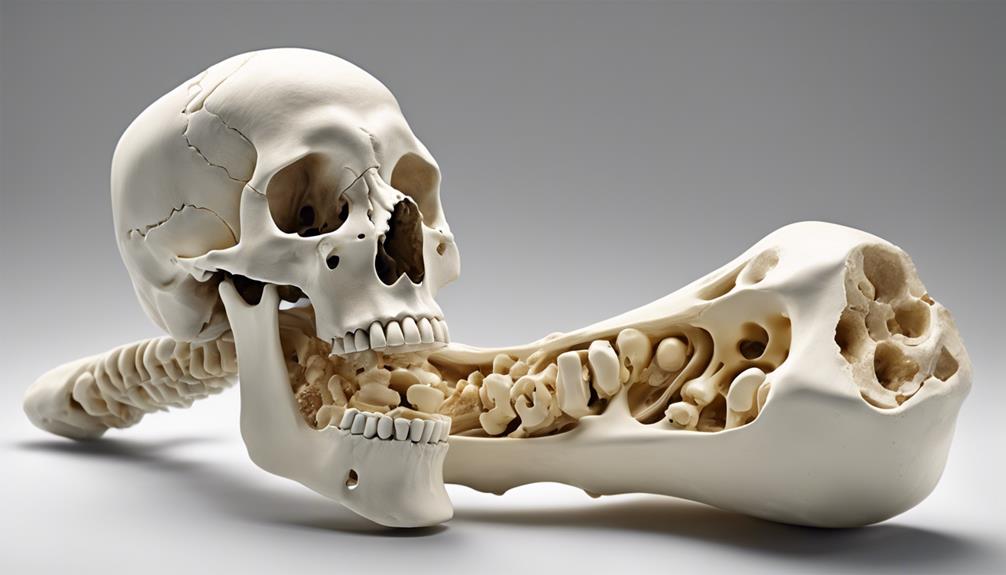
Osteoporosis Diagnosis Process
The Osteoporosis diagnosis process entails a comprehensive assessment of medical history, physical examinations, and specialized tests to evaluate bone health and fracture risk. Screening for osteoporosis often involves bone density scans, such as DEXA scans, to measure bone mineral density and assess fracture risk.
Additionally, blood or urine tests may be conducted to evaluate calcium levels, hormonal imbalances, and other factors relevant to bone health. Imaging tests like X-rays can help identify fractures or bone abnormalities associated with osteoporosis.
In cases where there's a family history of osteoporosis, genetic testing may be recommended to assess the risk of developing the condition based on genetic factors. It's essential for individuals to undergo these diagnostic procedures as part of their annual physical to identify potential issues early on and take preventive measures to maintain bone health.
Regular assessments and early detection can significantly help in preventing bone fractures and managing osteoporosis effectively.
Treatment Options for Osteoporosis

Treatment options for osteoporosis encompass a variety of medications, lifestyle modifications, and surgical interventions aimed at preventing bone loss and reducing fracture risk. When considering the best approach for managing osteoporosis, it's crucial to tailor the treatment plan to each individual's needs. Here are some key strategies:
- Medications: Bisphosphonates like alendronate and risedronate, along with denosumab, are commonly prescribed to help prevent bone loss and decrease fracture risk in osteoporosis patients.
- Hormone Therapy: Particularly beneficial for postmenopausal women, hormone therapy can improve bone density and strengthen bones, reducing the likelihood of fractures.
- Supplements and Lifestyle Changes: Calcium and vitamin D supplements are essential for supporting bone health. Additionally, incorporating weight-bearing exercises, quitting smoking, and moderating alcohol intake are recommended to manage osteoporosis effectively.
In severe cases, surgical interventions performed by orthopedic surgeons may be necessary to repair fractures and enhance bone health in patients with advanced osteoporosis. It's important to consult with healthcare providers to determine the most suitable treatment plan for each individual's unique needs and circumstances.
Finding the Right Healthcare Provider
When seeking optimal care for osteoporosis, identifying a competent healthcare provider is paramount for effective management and treatment. Consulting a primary care provider initially can lead to referrals to specialists such as rheumatologists, endocrinologists, gynecologists, geriatricians, physical therapists, and orthopedic surgeons, all of whom play crucial roles in treating osteoporosis.
The Bone Health & Osteoporosis Foundation's website can aid in locating knowledgeable healthcare providers in your area. Physical therapists can offer exercises to boost bone density and improve safety in daily activities, reducing the risk of bone fractures. Rheumatologists and endocrinologists are particularly skilled in diagnosing and treating osteoporosis effectively.
At Methodist West and other reputable medical centers, you can find a multidisciplinary team of specialists dedicated to providing comprehensive care for individuals with osteoporosis. By collaborating with these experts, you can ensure a tailored treatment plan that addresses your specific needs and promotes bone health.
Frequently Asked Questions
What Is the Best Doctor to See for Osteoporosis?
For osteoporosis, we recommend consulting with a specialist like a rheumatologist, endocrinologist, geriatrician, or gynecologist based on individual needs. Each specialist brings unique expertise to address specific aspects of the condition.
Rheumatologists focus on bone, joint, and muscle health, while endocrinologists excel in hormonal imbalances. Geriatricians cater well to older adults, and gynecologists are apt for women, especially those navigating menopausal challenges.
Choosing the right specialist ensures personalized care for optimal osteoporosis management.
What Does an Endocrinologist Do for Osteoporosis?
For osteoporosis, endocrinologists evaluate bone health, order bone density scans, and suggest treatments. Medications prescribed by endocrinologists can help slow bone loss and lower fracture risk. These specialists manage hormonal influences on bone density and overall skeletal health.
Working collaboratively with healthcare teams, endocrinologists develop comprehensive care plans tailored to each patient's needs. Their expertise in hormonal imbalances makes them vital in addressing osteoporosis and mitigating its effects.
How Does a Rheumatologist Treat Osteoporosis?
When treating osteoporosis, we prescribe medications like bisphosphonates, denosumab, and hormone therapy to slow bone loss and reduce fracture risk.
We guide patients on lifestyle changes, such as weight-bearing exercises and dietary adjustments, to enhance bone health.
Calcium and vitamin D supplements may be recommended to support bone strength.
Regular monitoring and collaboration with other healthcare providers help us assess treatment efficacy and provide comprehensive care for individuals with osteoporosis.
What Is the Newest Treatment for Osteoporosis?
The newest treatment for osteoporosis involves medications like Romosozumab, a monoclonal antibody that enhances bone formation and reduces fracture risk.
Approved for postmenopausal women with a high fracture risk or who've failed other treatments, Romosozumab boosts bone mass and strength by affecting both formation and resorption.
Administered via monthly injections for up to 12 months, it transitions to another medication afterward.
Clinical trials demonstrate its efficacy in reducing vertebral and nonvertebral fractures.
Conclusion
In conclusion, finding the right specialist for osteoporosis is crucial for effective management of this condition. Just like a skilled navigator guides a ship through turbulent waters, a knowledgeable healthcare provider can steer patients towards better bone health and reduced fracture risk.
By collaborating with these experts, individuals can navigate the complexities of osteoporosis treatment and embark on a journey towards stronger, healthier bones.
Osteoporosis Care
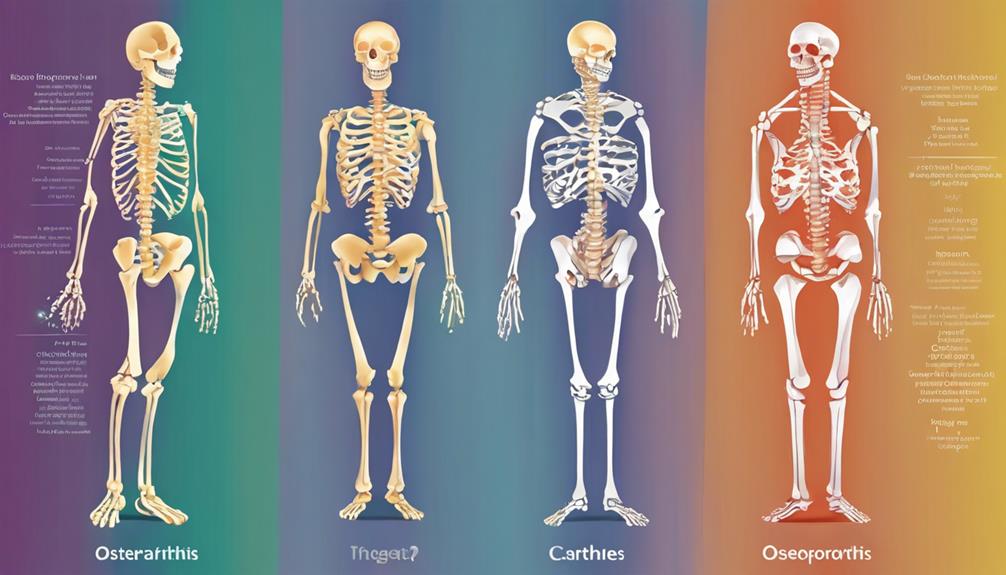
Osteoporosis Vs Osteoarthritis: Understanding the Key Differences
A deep dive into the differences between osteoporosis and osteoarthritis will enlighten you on how to distinguish these conditions accurately.

When it comes to bone and joint health, it is important to recognize the differences between osteoporosis and osteoarthritis in order to effectively manage these prevalent conditions.
While both impact bones and joints, the way they manifest and require treatment differs significantly. Let's explore the nuances between these two conditions and how recognizing their unique characteristics can empower us to make informed decisions about our health.
Key Takeaways
- Osteoporosis linked to bone loss, fractures, post-menopausal women.
- Osteoarthritis due to joint degeneration, pain, stiffness, aging.
- Osteoporosis prevention: bone density preservation strategies.
- Osteoarthritis treatment includes medications, joint replacements, lifestyle modifications.
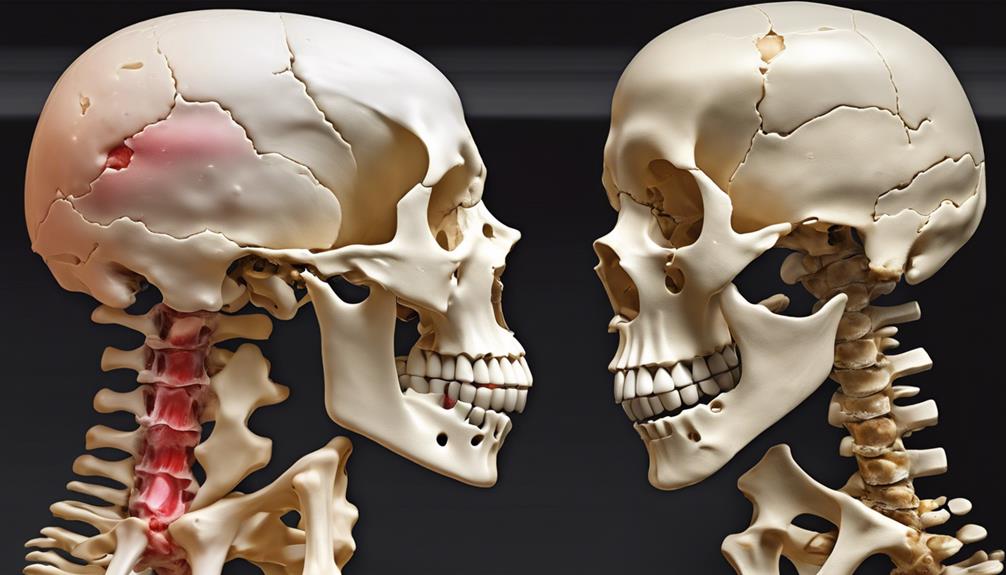
Key Differences in Causes
Comparing the causes of osteoporosis and osteoarthritis reveals distinct mechanisms underlying these prevalent musculoskeletal conditions. Osteoporosis primarily stems from bone loss and fragility, increasing the risk of fractures. Women, especially post-menopause, are more susceptible due to hormonal changes affecting bone density. On the other hand, osteoarthritis is mainly driven by degenerative joint processes, characterized by cartilage breakdown and bone spurs due to joint wear and tear. This condition is commonly linked to aging, joint overuse, or injury, affecting joint structure.
Factors contributing to osteoporosis include genetics, age, low calcium intake, and hormonal fluctuations. In contrast, osteoarthritis risk factors involve joint stress, obesity, and prior joint injuries. Understanding these distinctions is crucial for tailored prevention and management strategies. While osteoporosis focuses on preserving bone density to prevent fractures, osteoarthritis management often revolves around pain relief, improving joint function, and potentially surgical interventions to address severe joint damage. By recognizing these diverse causes, healthcare providers can offer more effective care to individuals affected by these conditions.
Symptoms of Osteoporosis

Bone density loss in osteoporosis can go unnoticed until a fracture risk increases significantly.
Back pain is a common symptom indicating potential bone weakening and fracture susceptibility.
Understanding these early signs is crucial for timely intervention and prevention of debilitating fractures.
Bone Density Loss
In osteoporosis, the loss of bone density often remains asymptomatic until a fracture occurs in critical areas such as the hip, spine, or wrist. Risk factors for osteoporosis include age, genetics, hormonal imbalances, and lifestyle choices like smoking and excessive alcohol consumption.
Low bone mineral density is a key indicator of osteoporosis, making bone density screenings crucial for early detection and effective management. Fractures in osteoporosis can be triggered by simple movements like bending or even sneezing due to weakened bones.
Diagnosis involves bone mineral density tests focusing on the spine and hip. Individuals with low bone mineral density face a significant risk of osteoporotic fractures, emphasizing the importance of proactive measures to prevent such occurrences.
Fracture Risk Increases
Considering the increased fracture risk associated with osteoporosis, early detection through bone mineral density testing is imperative for effective management and prevention strategies. Osteoporosis significantly raises the likelihood of fractures, particularly in weight-bearing bones like the hip, spine, and wrist.
Even minor actions such as bending or sneezing can lead to fractures due to compromised bone mass. Since osteoporosis is often asymptomatic until a fracture occurs, assessing bone density through specialized testing becomes crucial.
Fractures resulting from osteoporosis not only cause severe pain but also restrict mobility, impacting overall quality of life. Therefore, understanding and addressing fracture risk through proactive measures like bone mineral density testing are essential in combating the debilitating effects of osteoporosis.
Back Pain Common
Symptoms of osteoporosis commonly manifest as back pain, often indicating the presence of spinal fractures. This back pain is a result of weakened vertebrae due to bone loss, which can lead to sudden and severe discomfort.
Osteoporosis-related back pain may worsen with movement or certain positions, affecting daily activities. Recognizing these symptoms is crucial as early detection and treatment of osteoporosis can help prevent debilitating back pain and fractures.
Monitoring bone health through regular check-ups and lifestyle modifications can aid in reducing the risk of spinal fractures and associated back pain. Understanding the connection between bone health and back pain is essential for maintaining overall well-being and quality of life.
Symptoms of Osteoarthritis

When experiencing osteoarthritis, individuals may notice joint pain, stiffness, swelling, and a reduced range of motion as common symptoms. Osteoarthritis predominantly affects joints such as the hips, knees, fingers, feet, and spine.
The joint pain associated with osteoarthritis often worsens after physical activity or towards the end of the day. This condition can also lead to the development of bony growths or bone spurs within the affected joints, further exacerbating the discomfort experienced by individuals.
It's crucial to recognize that the symptoms of osteoarthritis can be easily overlooked or mistaken for general joint discomfort, highlighting the importance of accurate diagnosis and appropriate management strategies. By understanding these physical manifestations of osteoarthritis, individuals and healthcare providers can work together to effectively address and alleviate the challenges posed by this common joint condition.
Diagnosing Osteoporosis
An essential component of diagnosing osteoporosis involves conducting a bone mineral density test, commonly referred to as a DXA scan, to evaluate bone density in specific areas like the spine and hip. This test helps determine the presence of low bone mineral density, a key indicator of osteoporosis.
By comparing the patient's bone density to that of a young adult reference population, healthcare providers can assess the risk of fractures associated with osteoporosis. In addition to the DXA scan, blood tests may be included in the diagnostic process to rule out other conditions that could contribute to bone loss.
The World Health Organization defines osteoporosis based on bone mineral density T-scores, with values below -2.5 indicating the presence of osteoporosis. Early diagnosis plays a critical role in preventing fractures and effectively managing bone health, highlighting the importance of timely and accurate osteoporosis diagnosis.
Diagnosing Osteoarthritis

To accurately diagnose osteoarthritis, healthcare providers conduct a thorough review of the patient's medical history to evaluate joint symptoms and identify potential risk factors. Physical examinations play a crucial role in the diagnostic process, involving joint assessments and range of motion tests to assess the extent of joint damage and functional limitations.
Additionally, X-rays are commonly utilized to visualize specific changes associated with osteoarthritis, such as joint damage, bone spurs, and narrowing of joint spaces. Unlike some other conditions, blood tests are typically not necessary for diagnosing osteoarthritis, as the diagnosis primarily relies on clinical findings and imaging studies.
Risk Factors for Osteoporosis

A crucial factor in determining the susceptibility to osteoporosis fractures is low bone mineral density. Individuals with lower bone mineral density are at a higher risk of experiencing fractures due to weakened bones. Other significant risk factors for osteoporosis include older age, prior fractures, history of falls, certain medications such as corticosteroids, and a family history of fragility fractures.
Additionally, lifestyle factors like inadequate calcium or vitamin D intake, sedentary habits, and the use of certain medications can also increase the risk of developing osteoporosis.
To address these risk factors effectively, it's essential to promote bone health through adequate nutrition, regular weight-bearing exercise, and lifestyle modifications. Healthcare providers play a crucial role in educating individuals about these risks and guiding them towards preventive measures.
Understanding and addressing these risk factors are fundamental steps in the prevention and management of osteoporosis, ultimately leading to better bone health and reduced fracture risk.
Risk Factors for Osteoarthritis

In considering the risk factors for osteoarthritis, familial history emerges as a significant determinant. Understanding these risk factors is crucial in managing and preventing the development of this condition.
Here are four key factors to be aware of:
- Family History: Individuals with a family history of osteoarthritis are at a higher risk due to genetic predispositions that may affect bone mass and the health of affected joints.
- Physical Inactivity and Excess Weight: Sedentary lifestyles and obesity contribute to the risk of osteoarthritis by putting extra strain on the joints, leading to wear and tear.
- Joint Overuse: Occupations or activities that involve repetitive movements can increase the likelihood of osteoarthritis by putting stress on the affected joints over time.
- Medication Use: Certain medications, such as corticosteroids, can elevate the risk of developing osteoarthritis by impacting bone health and joint function.
Being mindful of these risk factors and taking proactive steps to address them can help in the prevention and management of osteoarthritis.
Treatment Options for Osteoporosis

Familial history, along with lifestyle modifications and pharmacological interventions, plays a significant role in the comprehensive treatment approach for osteoporosis. Treatment options for osteoporosis encompass various strategies aimed at improving bone health and reducing fracture risk.
Incorporating weight-bearing exercises into daily routines is crucial as they help strengthen bones and improve overall bone density. Additionally, medications such as Actonel, Fosamax, and Prolia are commonly prescribed to increase bone density and decrease the likelihood of fractures in individuals with osteoporosis.
Calcium and vitamin D supplementation are essential components of osteoporosis treatment to support bone health. Surgical interventions like kyphoplasty and vertebroplasty may be considered in severe cases to stabilize fractures and relieve pain.
Consulting with a specialist is highly recommended to develop personalized treatment plans tailored to individual needs and ensure ongoing management of osteoporosis. By combining lifestyle adjustments, pharmacological support, and medical guidance, individuals can effectively manage osteoporosis and reduce its impact on daily life.
Treatment Options for Osteoarthritis

Implementing a multifaceted approach that combines non-pharmacological methods, medications, and surgical interventions forms the core of treatment options for osteoarthritis. When addressing osteoarthritis, here are key strategies to consider:
- Non-Pharmacological Approaches: Exercise, weight management, and physical therapy play crucial roles in managing osteoarthritis symptoms and improving joint function.
- Medications for Symptom Relief: Commonly used medications like acetaminophen, NSAIDs, and corticosteroid injections can help alleviate pain and inflammation associated with osteoarthritis.
- Surgical Interventions: In severe cases where conservative measures fail, surgical options such as joint replacement or arthroplasty may be recommended to restore joint function.
- Hyaluronic Acid Injections: These injections can provide temporary relief by lubricating and cushioning the affected joint, offering a complementary treatment option for osteoarthritis management.
Managing Both Conditions Together

When managing both osteoporosis and osteoarthritis concurrently, it's crucial to focus on exercise for strength and maintaining joint mobility.
A balanced diet rich in calcium and vitamin D is essential to support bone health and overall well-being.
Exercise for Strength
Engaging in a diverse range of targeted exercises plays a crucial role in enhancing muscle strength, joint stability, and overall physical well-being for individuals concurrently managing osteoporosis and osteoarthritis. Here are four key exercise strategies to consider for improving strength and mobility while dealing with both conditions:
- Weight-bearing Exercises: Activities like walking, hiking, and dancing can help improve bone density and strengthen muscles.
- Resistance Training: Using light weights or resistance bands can assist in building muscle mass, supporting joint stability, and reducing the risk of falls.
- Tai Chi and Yoga: These practices enhance balance, flexibility, and coordination, which can improve joint mobility and alleviate pain.
- Water-Based Activities: Swimming or aqua aerobics provide low-impact options that support joint movement and muscle strength without straining bones.
Balanced Diet Importance
Enhancing muscle strength and joint stability through targeted exercises is foundational, and equally important is the role of a balanced diet rich in essential nutrients like calcium and vitamin D when managing both osteoporosis and osteoarthritis.
Calcium is crucial for maintaining bone mass, reducing fracture risk in osteoporosis, and supporting joint health in osteoarthritis. Vitamin D aids in calcium absorption, benefiting bone strength and joint function. Including omega-3 fatty acids, antioxidants, and anti-inflammatory foods can help alleviate inflammation and pain in osteoarthritis while supporting bone health in osteoporosis.
Additionally, maintaining a healthy weight through a balanced diet can ease pressure on arthritic joints and lower fracture risks. A well-rounded diet plays a key role in managing both conditions effectively.
Improving Bone Health

To enhance bone health effectively, incorporating weight-bearing exercises such as walking, dancing, and weightlifting into a regular routine is crucial. These activities help improve bone density and reduce the risk of osteoporosis.
To further support bone health, adequate intake of calcium and vitamin D through diet or supplements is essential. Additionally, resistance training, like using resistance bands or lifting weights, can help build muscle strength, which in turn supports bone health.
Avoiding smoking and excessive alcohol consumption is also crucial in preventing bone loss and maintaining overall bone health.
Tips for Improving Bone Health:
- Incorporate weight-bearing exercises like walking, dancing, and weightlifting into your routine.
- Ensure adequate intake of calcium and vitamin D through diet or supplements.
- Include resistance training in your workouts to build muscle strength and support bone health.
- Avoid smoking and excessive alcohol consumption to prevent bone loss.
Understanding Joint and Cartilage Problems

Understanding joint and cartilage problems involves delving into the complexities of osteoarthritis, which encompasses joint deterioration and bone-on-bone issues in various areas such as fingers, knees, hips, spine, neck, and shoulders. Osteoarthritis is linked to the loss of bone mass and affects millions worldwide. The relationship between osteoarthritis and bone health is crucial, as the condition leads to a gradual breakdown of cartilage, causing pain, stiffness, and reduced function in the affected joints. Excess body weight can exacerbate osteoarthritis, making it essential to manage weight to alleviate symptoms. Diagnosis includes a comprehensive evaluation, including medical history, physical examination, and imaging studies. X-rays often reveal joint narrowing and bone spurs, characteristic of osteoarthritis. Treatment focuses on symptom management through weight management, exercise, pain relief strategies, and in severe cases, surgical interventions like joint replacement. By understanding these joint and cartilage problems, individuals can take proactive steps to address and alleviate the impact of osteoarthritis on their daily lives.
| Key Points | Details | Importance |
|---|---|---|
| Joint Deterioration | Gradual breakdown of cartilage in joints | Manage symptoms |
| Bone-on-Bone Issues | Direct contact between bone ends | Pain and reduced mobility |
| Excess Body Weight | Exacerbates osteoarthritis symptoms | Weight management crucial |
Effective Bone Health Treatments
Effective treatments for osteoporosis encompass a range of strategies, including lifestyle adjustments, medication options like Actonel and Fosamax, and surgical interventions such as kyphoplasty and vertebroplasty. When managing osteoporosis, it's essential to prioritize bone health through weight-bearing exercises and proper nutrition. Here are four key components of effective bone health treatments:
- Lifestyle Adjustments: Incorporating weight-bearing exercises into daily routines can help strengthen bones and reduce the risk of fractures associated with osteoporosis.
- Medication Options: Medications like Actonel and Fosamax are prescribed to slow down bone loss and improve bone density in individuals with osteoporosis.
- Calcium and Vitamin D Supplementation: Adequate calcium and vitamin D intake is crucial for maintaining bone health and supporting the effectiveness of other osteoporosis treatments.
- Surgical Interventions: Procedures such as kyphoplasty and vertebroplasty may be recommended to stabilize fractures and relieve pain in individuals with severe osteoporosis.
Consulting with a specialist can help tailor a treatment plan that addresses individual needs and ensures optimal management of osteoporosis.
Protecting Joints and Bones
Weight-bearing and strength training exercises play a crucial role in safeguarding bones and joints in both osteoporosis and osteoarthritis. Maintaining a healthy weight is essential to reduce joint stress and prevent bone loss in these conditions.
Implementing joint protection techniques and avoiding overuse can help alleviate symptoms and preserve joint function.
Bone Density Importance
Maintaining optimal bone density is a critical factor in safeguarding joint health and preventing the risks associated with osteoporosis and osteoarthritis. Here are four essential points to consider:
- Monitoring bone density is crucial for protecting joints and bones from the risks of osteoporosis and osteoarthritis.
- Low bone density can increase the likelihood of fractures in individuals with osteoporosis, impacting joint health.
- Bone density tests such as DXA scans offer vital information on bone strength and density, guiding preventive measures.
- Optimal bone density maintenance supports joint function and minimizes the effects of degenerative joint diseases.
Understanding bone density levels facilitates early detection and interventions for managing risks associated with osteoporosis and osteoarthritis.
Joint Mobility Exercises
Monitoring bone density is crucial for protecting joints and bones from the risks of osteoporosis and osteoarthritis. Incorporating joint mobility exercises is a key strategy in maintaining optimal joint health and function. Joint mobility exercises play a vital role in enhancing flexibility, reducing stiffness, and preserving range of motion, essential for managing osteoarthritis and osteoporosis.
Engaging in weight-bearing activities such as walking, dancing, or stair climbing can effectively strengthen bones and support overall joint health. Furthermore, gentle stretches and low-impact exercises like yoga or tai chi can improve balance and coordination, reducing the risk of falls and injuries.
Regular physical activity is imperative for sustaining joint function and preventing bone loss in individuals with osteoarthritis and osteoporosis.
Tips for Better Bone Health
To optimize bone health, it's crucial to prioritize a balanced diet rich in calcium and vitamin D to support bone strength and density. Here are four tips for better bone health:
- Ensure Adequate Calcium and Vitamin D Intake: Incorporate dairy products, leafy greens, and fortified cereals into your diet to support bone density and reduce the risk of hip fractures.
- Engage in Weight-Bearing Exercises: Activities like walking, dancing, or weightlifting can help strengthen bones and lower the chances of developing osteoporosis.
- Avoid Smoking and Limit Alcohol: These habits can weaken bones, increasing the risk of fractures. By cutting down on smoking and moderating alcohol intake, you can maintain bone health.
- Incorporate Resistance and Balance Training: Including resistance exercises and balance training in your routine can enhance muscle strength and stability, reducing the likelihood of falls and fractures.
Frequently Asked Questions
What Is Difference Between Osteoarthritis and Osteoporosis?
When comparing osteoarthritis and osteoporosis, it's crucial to note that osteoarthritis primarily affects joints, leading to pain and reduced mobility, while osteoporosis is characterized by low bone mass, increasing fracture risk.
This distinction is vital in understanding the differing impacts these conditions have on the body. By recognizing these differences, healthcare providers can tailor treatments to address each condition effectively.
What Are the 4 Stages of Osteoarthritis?
In the realm of osteoarthritis, the progression unfolds through four distinct stages: mild, moderate, severe, and end-stage. Each stage showcases varying degrees of joint cartilage degradation, resulting in escalating levels of pain, stiffness, and reduced mobility.
From the initial mild discomfort to the debilitating end-stage symptoms necessitating surgical remedies, the journey through these phases underscores the impactful nature of osteoarthritis on joint health.
What Are 5 Symptoms of Osteoporosis?
We can't stress enough the importance of recognizing the symptoms of osteoporosis. These signs can include back pain, height loss, a stooped posture, and bone fractures from minor stress.
Fractures often affect the spine, hip, or wrist. As bone fragility increases, so does the risk of fractures. Osteoporosis is stealthy; it may hide until a sudden break shows its presence.
Early detection is key for managing this condition.
What Is the Difference Between Osteoporosis and Degenerative Bone Disease?
When comparing osteoporosis to degenerative bone diseases, the key difference lies in the areas they affect. Osteoporosis primarily impacts bone strength and density, leading to increased fracture risk.
In contrast, degenerative bone diseases like osteoarthritis target joint function and mobility, resulting in pain and stiffness.
Understanding these distinctions is crucial for accurate diagnosis and appropriate treatment interventions to improve patient outcomes and quality of life.
Conclusion
In conclusion, the stark contrast between osteoporosis and osteoarthritis is undeniable. While osteoporosis threatens to turn our bones into fragile, brittle shells waiting to shatter at the slightest touch, osteoarthritis mercilessly attacks our joints, causing excruciating pain and stiffness.
Understanding the nuances of these conditions is crucial in managing and treating them effectively. Let's arm ourselves with knowledge and take proactive steps to protect our bones and joints for a healthier future.
Osteoporosis Care
What Are the Symptoms of Senile Osteoporosis?
Mysteries abound in the realm of Senile Osteoporosis, offering a tantalizing glimpse into the intricate web of factors shaping this silent bone enemy.

As we get older, senile osteoporosis silently undermines our bone strength, acting like a sneaky foe.
As we explore the intricate mechanisms underlying this condition, we unravel a tapestry of factors influencing its onset and progression.
From the subtle changes in bone architecture to the clinical manifestations that often go unnoticed, the complexities of senile osteoporosis beckon us to delve deeper into its mysteries, shedding light on how we can better understand and manage this silent threat to our skeletal health.
Key Takeaways
- Hormonal shifts and reduced estrogen play a significant role.
- Exercise diversity crucial for bone health maintenance.
- Genetic predisposition and zinc deficiency are risk factors.
- Support groups and online resources aid in coping and education.
Causes of Senile Osteoporosis
Senile osteoporosis, a condition primarily caused by age-related bone loss and slower bone growth, significantly increases the susceptibility to fractures. Hormonal shifts, particularly in women, contribute to the development of senile osteoporosis. These shifts, such as reduced estrogen levels during menopause, can accelerate bone loss. Factors like body size, race, family history, diet, and lifestyle also play essential roles in the risk of developing this condition. For instance, individuals with a family history of osteoporosis or those with a diet lacking in calcium are at higher risk.
To maintain bone health and reduce the risk of senile osteoporosis, regular weight-bearing exercises are crucial. Exercises like walking, dancing, or weight training help improve bone density and strength. Understanding these causes of senile osteoporosis is vital for effective prevention and management strategies. By addressing these risk factors early on through lifestyle modifications, proper nutrition, and medical interventions when necessary, we can work towards reducing the prevalence and impact of this condition.
Symptoms and Signs

As bone mass decreases and fragility increases with age, individuals may start experiencing subtle changes that signal the onset of osteoporosis. Senile osteoporosis, characterized by progressive loss of bone mass, manifests through various symptoms and signs:
- Increased Risk of Fractures: Fragile bones in senile osteoporosis are more prone to fractures, even from minor incidents, leading to significant pain and immobility.
- Vertebral Fractures: Senile osteoporosis often results in vertebral fractures, causing severe back pain, height loss, and a hunched posture, impacting daily activities and overall quality of life.
- Chronic Symptoms: Symptoms of senile osteoporosis can be chronic and debilitating, affecting independence and overall health in older individuals. Managing these symptoms early on is crucial to prevent further bone deterioration and reduce the risk of fractures.
Proper intervention and care are essential to improve outcomes and enhance the well-being of individuals affected by senile osteoporosis.
Diagnostic Approaches
Utilizing a combination of advanced imaging techniques and clinical assessments, healthcare providers employ a comprehensive approach to diagnose and evaluate senile osteoporosis accurately.
Bone mineral density (BMD) measurements through dual-energy X-ray absorptiometry (DEXA) are crucial in identifying low bone mass and diagnosing osteoporosis in older individuals. The FRAX tool plays a vital role in estimating the 10-year probability of major osteoporotic fractures and hip fractures based on clinical risk factors, aiding in treatment decisions.
Blood tests measuring calcium, vitamin D levels, and bone turnover markers provide valuable information for diagnosing and assessing the severity of senile osteoporosis. Imaging studies such as X-rays, CT scans, and MRI help detect fractures, evaluate bone structure, and monitor disease progression in seniors.
Furthermore, clinical evaluation by healthcare providers, including assessing risk factors, medical history, physical examination, and symptom review, is essential for an accurate diagnosis of senile osteoporosis, ensuring appropriate management and care for affected individuals.
Risk Factors to Consider

Considering the multitude of factors that contribute to the risk of senile osteoporosis, it's imperative to acknowledge and address specific key elements that significantly impact bone health in older individuals.
When evaluating the risk of senile osteoporosis, it's crucial to consider:
- Age: As individuals age, the risk of developing osteoporosis increases due to natural bone density loss and decreased bone regeneration processes.
- Low Body Mass Index (BMI): Low BMI is associated with reduced bone density and an increased risk of fractures, making it a critical factor to consider in assessing osteoporosis risk.
- Genetic Factors: Genetic predisposition, including factors like race, age, body weight, and gender, can significantly influence an individual's susceptibility to senile osteoporosis.
These factors, coupled with zinc deficiency, inadequate calcium intake, poor vitamin D absorption, and peak bone mass levels, all play essential roles in determining bone density and overall bone health in aging individuals.
Treatment Options Available
Our approach to treating senile osteoporosis involves a combination of hormonal therapy, calcium supplementation, and vitamin D therapy to enhance bone formation and decrease bone resorption. Hormonal therapy helps maintain bone density by balancing hormone levels, reducing the risk of fractures in individuals with senile osteoporosis. Calcium supplementation is crucial as aging bodies may struggle to absorb enough calcium from diet alone, supporting bone strength and density. Vitamin D therapy aids in calcium absorption, promoting bone health and reducing fracture risk.
In addition to these foundational treatments, bisphosphonates are commonly prescribed to manage senile osteoporosis. These medications help to prevent bone loss, improve bone density, and reduce the risk of fractures in elderly individuals. Alongside pharmacological interventions, non-pharmacological approaches like modified diet and exercise play a vital role in treatment and prevention. Ensuring adequate intake of calcium and vitamin D3 is essential for supporting bone health and preventing further bone deterioration in individuals with senile osteoporosis.
Ongoing research into the anabolic effects of certain medications on bone offers promising avenues for future treatment options.
Importance of Nutrition

Exploring the role of nutrition in senile osteoporosis management reveals its crucial impact on preventing bone loss and promoting overall bone health. Adequate intake of calcium and vitamin D is essential for maintaining bone health in senile osteoporosis. Here's why nutrition is vital:
- Calcium-Rich Foods: Incorporating dark green vegetables, dairy products, and fish into the diet can help support bone density.
- Vitamin D Sources: Consuming fatty fish, egg yolks, and fortified foods is beneficial for calcium absorption and bone strength.
- Supplements: Individuals who don't receive sufficient vitamin D through diet and sunlight exposure may require supplements to meet their needs.
A balanced diet, along with weight-bearing exercises and lifestyle modifications, plays a significant role in supporting bone health and reducing the risk of fractures in senile osteoporosis. By focusing on nutrition and ensuring adequate intake of essential nutrients, individuals can take proactive steps towards maintaining strong and healthy bones in their postmenopausal years.
Exercise Recommendations

Engage in regular weight-bearing exercises like walking, dancing, or weight lifting to enhance bone density and strength for individuals managing senile osteoporosis. These activities are crucial for improving bone health and reducing the risk of fractures in seniors. Additionally, incorporating strength training exercises into your routine can help maintain muscle mass and bone strength. Balance exercises are also essential to prevent falls, which can lead to serious injuries in individuals with osteoporosis.
Consider incorporating high-impact exercises like jumping or running, as these activities stimulate bone formation and reduce bone loss in older adults with senile osteoporosis. Moreover, activities such as tai chi or yoga can enhance flexibility, posture, and overall bone health.
Following a well-rounded exercise program that includes aerobic, strength training, and balance exercises is recommended for seniors with osteoporosis to promote bone density, mobility, and independence. By prioritizing regular physical activity, individuals can take proactive steps to manage senile osteoporosis and improve their quality of life.
Lifestyle Modifications
To optimize bone health and reduce the risk of fractures in individuals managing senile osteoporosis, incorporating lifestyle modifications such as regular weight-bearing exercises and a balanced diet rich in calcium and vitamin D is crucial. These changes aid in improving bone density, reducing the risk of fractures, and enhancing overall quality of life.
Here are three essential lifestyle modifications for individuals dealing with senile osteoporosis:
- Regular Weight-Bearing Exercises: Engaging in activities like walking, dancing, or stair climbing can help strengthen bones, improve balance, and reduce the risk of falls.
- Balanced Diet with Calcium and Vitamin D: Consuming foods high in calcium and vitamin D supports bone health, enhances calcium absorption, and reduces the likelihood of low bone mass and fractures.
- Preventive Measures to Avoid Falls: Using assistive devices, wearing appropriate footwear, and being cautious on slippery surfaces can significantly decrease the risk of falls and subsequent fractures.
Complications and Consequences

Senile osteoporosis poses significant risks of debilitating fractures in key areas of the body, such as the spine, hip, proximal humerus, and distal forearm. Vertebral fractures, a common consequence of this condition, can lead to severe back pain, height loss, and an increased risk of future fractures. Fragility fractures in senile osteoporosis are especially concerning as bones become more susceptible to breaking from minor incidents due to decreased bone mass and strength.
The chronic impact of bone mass loss in senile osteoporosis can manifest in various ways, affecting daily life and mobility. Over time, the progressive nature of this condition can result in a significant decrease in the quality of life for those affected, emphasizing the importance of early detection and management to mitigate the risk of these debilitating fractures.
It's crucial to address these complications to prevent further deterioration and enhance the overall well-being of individuals dealing with senile osteoporosis.
Prevention Strategies

In safeguarding against senile osteoporosis, prioritizing regular weight-bearing exercises remains a cornerstone in fortifying bone density and strength. Engaging in activities like walking, dancing, or weight training can make a significant impact on bone health. Additionally, ensuring an adequate intake of calcium and vitamin D through a balanced diet or supplements is crucial for maintaining strong bones. Here are three essential strategies to prevent senile osteoporosis:
- Fall Prevention: Implement strategies such as keeping homes well-lit, decluttered, using handrails, and wearing appropriate footwear to reduce the risk of falls and fractures in seniors with osteoporosis.
- Regular Health Check-ups: Schedule routine check-ups, including bone density scans, to detect osteoporosis early, allowing for timely interventions that can improve outcomes and reduce complications.
- Lifestyle Modifications: Make positive changes like quitting smoking, moderating alcohol intake, and maintaining a healthy weight to prevent senile osteoporosis and preserve bone health. These adjustments can have a significant impact on overall well-being and quality of life.
Support and Resources

We understand the importance of support and resources in managing senile osteoporosis. Support groups tailored for seniors provide a platform for sharing experiences and coping strategies.
Online osteoporosis resources offer valuable information on treatments and lifestyle adjustments for individuals dealing with this condition.
Support Groups for Seniors
Support groups for seniors with senile osteoporosis play a vital role in providing emotional support, education, and valuable resources for managing the condition effectively. These groups offer a sense of community and understanding among individuals facing similar challenges with bone health.
Participants can share experiences, coping strategies, and tips for improving bone strength and preventing falls. Support groups often organize educational sessions, guest speakers, and social activities to enhance overall well-being.
Joining a support group for senile osteoporosis can empower seniors to take control of their health and improve their quality of life. It's a safe space where individuals can find encouragement, information, and companionship on their journey towards better bone health.
Online Osteoporosis Resources
Navigating the realm of online osteoporosis resources opens a gateway to a wealth of support, information, and tools for individuals managing senile osteoporosis. These online resources provide access to educational materials, research articles, and valuable information to help understand and cope with senile osteoporosis.
Support groups and forums offer emotional support and a platform to connect and share experiences with others facing similar challenges. Websites dedicated to osteoporosis offer practical tips on lifestyle modifications, exercise routines, and nutritional guidance tailored to seniors.
Frequently Asked Questions
How Do You Treat Severe Senile Osteoporosis?
We treat severe senile osteoporosis by combining pharmacological interventions like bisphosphonates to decrease bone resorption and improve density. Calcium and vitamin D3 supplementation are crucial for bone health.
Non-pharmacological methods include a calcium-rich diet and weight-bearing exercise. Our goal is to slow bone loss, improve strength, and reduce fracture risk.
Early intervention with medication, nutrition, and lifestyle changes is vital for effective management.
What Is the Life Expectancy of a Person With Osteoporosis?
We understand the concern about life expectancy in individuals with osteoporosis.
It's important to emphasize that timely diagnosis, proper management, and preventive measures can significantly impact longevity.
By prioritizing bone health through lifestyle changes, medication, and regular monitoring, we can reduce the risk of fractures and improve overall quality of life.
Taking proactive steps to address osteoporosis can lead to a longer, healthier, and more fulfilling life.
Can Vitamin D Reverse Osteoporosis?
Yes, vitamin D can potentially help reverse osteoporosis by supporting bone health and strength. Adequate levels of vitamin D are crucial for maintaining bone density and reducing the progression of osteoporosis, especially in older individuals.
Studies suggest that vitamin D supplementation can aid in preventing and treating osteoporosis by promoting bone mineralization and lowering fracture risk. Including vitamin D-rich foods in the diet or taking supplements under medical guidance may assist in managing osteoporosis effectively.
What Are the 5 Stages of Osteoporosis?
Sure!
The five stages of osteoporosis progress from normal bone density to severe bone weakness and complications. Beginning with optimal bone health, one moves through osteopenia, early, moderate, and advanced osteoporosis, where fracture risk increases significantly.
How can we best support individuals transitioning through these stages with compassion and evidence-based care? Let's explore ways to serve those affected by this condition with understanding and knowledge.
Conclusion
In conclusion, senile osteoporosis is a complex condition that requires attention and care. By understanding the causes, symptoms, and treatment options available, individuals can take proactive steps to manage their bone health.
Remember, 'an ounce of prevention is worth a pound of cure.' With proper lifestyle modifications, support, and resources, we can work towards preventing fractures and maintaining strong bones as we age.
Let's prioritize our bone health for a brighter, healthier future.
-

 Dementia Care2 weeks ago
Dementia Care2 weeks agoUnderstanding the Stages of Vascular Dementia: A Visual Chart Guide
-

 Dementia Care2 weeks ago
Dementia Care2 weeks agoHow Gabapentin Affects Dementia: A Comprehensive Guide
-

 Dementia Care2 weeks ago
Dementia Care2 weeks ago10 Engaging Dementia Games for Cognitive Stimulation
-

 Dementia Care3 weeks ago
Dementia Care3 weeks ago5 Things You Need to Know About Jack Nicholson’s Dementia
-

 Dementia Care1 week ago
Dementia Care1 week agoUnderstanding Narcissism and Dementia: A How-To Guide
-

 Dementia Care1 week ago
Dementia Care1 week agoDavid Suchet’s Wife Opens Up About Living with Dementia
-

 Dementia Care1 week ago
Dementia Care1 week agoHow to Deal with a Parent’s Dementia: A Practical Guide
-

 Dementia Care5 days ago
Dementia Care5 days agoUnderstanding the Link Between Ambien and Dementia: A How-To Guide