Exploring the 2022 guidelines for osteoporosis management is akin to embarking on a voyage into unknown territory, led by a compass directing towards optimal bone health. Delving into these recommendations reveals numerous evidence-based strategies aimed at enhancing the durability and robustness of the skeletal system.
From the shores of prevention to the horizon of pharmacological interventions, every aspect of osteoporosis management beckons us to unravel its complexities and embrace a holistic approach toward wellness. Curiosity piqued? Let's venture forth into the realm of osteoporosis care together.
Importance of Osteoporosis Treatment
Understanding the significance of osteoporosis treatment is paramount in safeguarding bone health and reducing fracture risk in individuals, particularly those undergoing glucocorticoid therapy. Following treatment guidelines is crucial, starting with an initial fracture risk assessment for adults beginning glucocorticoid therapy. Factors such as dosage and duration play a critical role in determining the level of risk. For those at medium to very high risk, pharmacologic treatment is strongly recommended.
Oral bisphosphonates are the preferred option for high-risk patients due to their effectiveness. In cases where higher risk necessitates it, anabolic agents like denosumab, teriparatide, and romosozumab may be considered, although conditionally. Additionally, guidelines stress the importance of calcium and vitamin D supplementation, lifestyle adjustments, and regular monitoring for all patients on chronic glucocorticoid therapy.
Key Recommendations for Fracture Prevention

When considering fracture prevention, our guidelines stress the importance of conducting initial fracture risk assessments for adults commencing glucocorticoid treatment, taking into account various factors such as dose and duration of use.
Regular reassessment every 1 to 2 years is recommended for those on chronic glucocorticoid therapy, involving a comprehensive evaluation including clinical history, FRAX scores, bone mineral density, and imaging studies.
For individuals at medium to very high fracture risk levels, pharmacologic interventions play a crucial role, with oral bisphosphonates being the preferred choice for those at high and very high risk categories.
Fracture Risk Assessment
Conducting an initial fracture risk assessment is a crucial step for adults initiating glucocorticoid (GC) treatment, considering factors like dose, duration, and pattern of GC use. For ongoing therapy, reassessment every 1 to 2 years is recommended, incorporating clinical history, FRAX scores, bone mineral density (BMD) values, and imaging.
Specific thresholds for FRAX scores, BMD values, and hip fracture risk percentages help categorize individuals into moderate and low fracture risk groups. Pharmacologic treatment is strongly advised for medium to very high fracture risk, with oral bisphosphonates as the preferred choice for those at high and very high risk. Anabolic agents are conditionally recommended for high and very high fracture risk situations, with denosumab, teriparatide, and romosozumab as alternative options based on individual risk levels.
Pharmacological Treatment Options
In high and very high fracture risk scenarios for postmenopausal women, oral bisphosphonates are the primary choice for pharmacological treatment. These medications help in reducing the risk of fractures by maintaining bone density.
Anabolic agents like teriparatide are conditionally recommended for women at very high risk of fractures, promoting bone formation.
Denosumab, teriparatide, and romosozumab are alternative options for treatment based on individual risk levels.
Regular reassessment of fracture risk is advised after 3-5 years of bisphosphonate treatment.
Shared decision-making plays a crucial role in tailoring the most effective pharmacological therapy for osteoporosis, considering individual patient factors. By involving patients in the decision-making process, healthcare providers can ensure personalized and optimal treatment outcomes.
Strategies for Bone Health Maintenance
Implementing a comprehensive regimen of weight-bearing exercises and muscle-strengthening routines is fundamental for preserving bone health and minimizing the risk of fractures in individuals vulnerable to osteoporosis. To maintain optimal bone health and reduce the likelihood of fractures, consider the following strategies:
- Ensure Proper Calcium and Vitamin D Intake: Adequate levels of calcium and vitamin D are essential for bone strength and density.
- Adopt a Balanced Diet: A diet rich in nutrients supports overall bone health and aids in preventing osteoporosis-related fractures.
- Incorporate Fall Prevention Measures: Implement strategies such as home safety assessments and balance training to reduce the risk of falls and subsequent fractures.
- Regular Bone Mineral Density Monitoring: Stay proactive by scheduling screenings and assessments to track changes in bone health and assess the effectiveness of preventive measures.
Pharmacological Treatments Overview
Our approach to examining the pharmacological treatments for osteoporosis focuses on outlining the recommended therapies for individuals at varying levels of fracture risk. Bisphosphonates are the cornerstone of treatment, particularly for high-risk postmenopausal women.
Anabolic therapy is reserved for those at very high fracture risk. Denosumab, Teriparatide, Abaloparatide, and Romosozumab are among the pharmacological options recommended for postmenopausal women with elevated fracture risk.
Guidelines stress the importance of regular reassessment of fracture risk, especially after 3-5 years of bisphosphonate therapy. Tailored pharmacological therapies play a vital role in optimizing treatment outcomes by matching interventions with individual risk profiles.
Non-Pharmacological Approaches
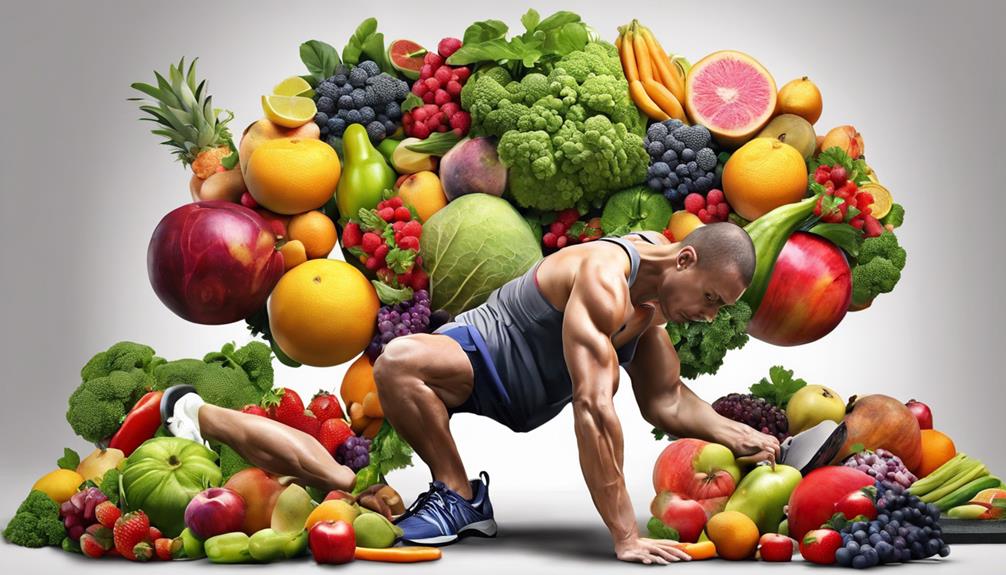
To comprehensively address osteoporosis management, exploring non-pharmacological approaches becomes imperative, focusing on lifestyle modifications, exercise regimens, and dietary considerations crucial for enhancing bone health and reducing fracture risk.
- Weight-Bearing Exercises: Incorporating activities like walking, jogging, and dancing can strengthen bones and decrease the likelihood of fractures.
- Balance and Strength Training: Engaging in exercises such as yoga and tai chi improves stability, reducing the risk of falls in individuals with osteoporosis.
- Calcium and Vitamin D Intake: Ensuring adequate levels of these nutrients through diet or supplements is vital for maintaining bone health and preventing osteoporosis.
- Lifestyle Modifications: Quitting smoking, moderating alcohol consumption, and adopting a healthy lifestyle are pivotal in lowering the chances of osteoporotic fractures.
Special Populations Considerations

When considering special populations in osteoporosis treatment, we must address the unique care needs of elderly patients and the impact of menopause on bone health.
Tailored approaches for elderly individuals, including fall prevention strategies and appropriate medication adjustments, are crucial in managing osteoporosis effectively.
Understanding how menopause affects bone density and implementing targeted interventions are essential aspects of providing comprehensive care for this specific group.
Elderly Patients' Care
Evaluating fall risk, optimizing bone health through exercise, and ensuring adequate calcium and vitamin D intake are crucial considerations for elderly patients with osteoporosis to prevent fractures and maintain their quality of life. When caring for elderly patients with osteoporosis, we must focus on:
- Fall Prevention: Implementing strategies to reduce the risk of falls, such as removing hazards in the living environment and promoting balance exercises.
- Regular Screening: Conducting routine screenings for osteoporosis to identify individuals at risk for fractures early on.
- Medication Management: Ensuring appropriate use of medications to strengthen bones and prevent further bone loss.
- Comprehensive Care: Adopting a multidisciplinary approach involving healthcare professionals to address all aspects of osteoporosis management and prevention in the elderly population.
Menopause Impact on Bone
Accelerated bone loss during menopause, driven by decreased estrogen levels, significantly heightens the risk of osteoporosis and fractures in women. Postmenopausal women often experience a rapid decline in bone mineral density, especially in the initial 5-7 years following menopause. Estrogen deficiency during this period affects bone remodeling, leading to decreased bone formation and increased bone resorption. Menopausal hormone therapy (MHT) stands out as a potential intervention to help preserve bone density and reduce fracture risk in postmenopausal women. Special considerations for menopausal women entail individualized assessment of fracture risk, continuous monitoring of bone health, and early implementation of preventive strategies.
| Menopausal Impact on Bone | |
|---|---|
| Accelerated bone loss due to decreased estrogen levels | Heightened risk of osteoporosis and fractures |
| Rapid decline in bone mineral density postmenopause | Effects on bone remodeling and increased resorption |
| Menopausal hormone therapy benefits bone density maintenance | Individualized fracture risk assessment and preventive strategies |
Osteoporosis Screening Guidelines

Bone density screening is recommended by ACOG for postmenopausal patients aged 65 and older to assess osteoporosis risk. When considering osteoporosis screening guidelines, it's essential to understand the following key points:
- ACOG Recommendations: ACOG emphasizes bone density screening for postmenopausal women aged 65 and older as a crucial step in assessing osteoporosis risk.
- Fracture Risk Assessment: Younger patients with a fracture risk exceeding 8.4% also benefit from screening to identify early signs of osteoporosis.
- Prevalence of Osteoporotic Fractures: Approximately 50% of women experience an osteoporotic fracture in their lifetime, highlighting the significance of early screening and diagnosis.
- Importance of Screening and Diagnosis: New recommendations stress the critical role that screening and diagnosis play in effectively managing osteoporosis and reducing the risk of fractures.
Fracture Risk Assessment Tools

When considering strategies for assessing osteoporosis risk beyond standard bone density screening, one valuable approach involves utilizing fracture risk assessment tools such as the Fracture Risk Assessment Tool (FRAX).
FRAX estimates the 10-year probability of major osteoporotic fractures by considering various factors such as age, sex, weight, height, previous fractures, parental history of hip fracture, smoking, alcohol use, rheumatoid arthritis, and glucocorticoid use.
Dual-energy X-ray absorptiometry (DXA) scans are employed to measure bone mineral density and assess fracture risk in conjunction with clinical risk factors. By incorporating FRAX calculations with bone density measurements, healthcare providers can categorize individuals into low, moderate, high, or very high risk for fractures, aiding in treatment decisions.
This comprehensive assessment of fracture risk assists in guiding osteoporosis management strategies effectively.
Initial Treatment Approaches

In formulating optimal treatment plans for osteoporosis patients, healthcare providers carefully consider a range of pharmacologic interventions tailored to individual fracture risk levels. The initial treatment approaches in 2022 focus on addressing the varying needs of patients with different levels of fracture risk. Here are key points to consider:
- Oral Bisphosphonates: These are the preferred first-line therapy for individuals at high and very high risk of fractures due to their proven efficacy in reducing fracture incidence.
- Anabolic Agents: For patients at high or very high risk of fractures, anabolic agents may be considered to improve bone density and reduce fracture risk.
- Additional Treatment Options: Denosumab, teriparatide, and romosozumab are additional pharmacologic interventions that may be included in the treatment plan based on individual risk levels.
- Tailored Treatment Strategies: Treatment strategies are individualized, taking into account factors such as age, fracture risk level, and specific clinical considerations to optimize outcomes and enhance patient care.
Addressing Treatment Failure

Addressing treatment failure in osteoporosis management necessitates a comprehensive approach that involves assessing medication adherence, recognizing contributing factors, and implementing targeted interventions to enhance therapeutic outcomes. Poor adherence to osteoporosis medications can significantly contribute to treatment failure, with approximately 50% of patients discontinuing their treatment within the first year. Factors such as medication side effects, complex dosing regimens, and perceived lack of benefit can also play a role in treatment failure. Inadequate intake of essential nutrients like calcium and vitamin D can further exacerbate the situation, impacting bone health and increasing fracture risk.
To address treatment failure effectively, monitoring bone turnover markers can aid in early detection, allowing for timely adjustments in therapy to improve outcomes. A multidisciplinary approach involving healthcare providers, pharmacists, and patient education is crucial in optimizing treatment efficacy. By working together, healthcare professionals can identify barriers to adherence, provide necessary support, and tailor interventions to meet the individual needs of patients, ultimately improving osteoporosis management outcomes.
Management Post-Glucocorticoid Discontinuation

Upon glucocorticoid discontinuation, vigilant monitoring and strategic management are imperative to mitigate fracture risks and prevent bone loss. To effectively manage patients post-glucocorticoid discontinuation, the following steps should be considered:
- Fracture Risk Assessment: Conduct a thorough evaluation to assess the patient's risk of fractures based on clinical factors, bone density testing, and previous medical history.
- Osteoporosis Management: Develop an individualized treatment plan tailored to the patient's specific needs, considering factors such as fracture risk, bone health status, and prior response to osteoporosis therapies.
- Healthcare Collaboration: Foster close collaboration between healthcare providers and patients to ensure comprehensive care, timely interventions, and adherence to the treatment plan for optimal outcomes.
- Preventing Osteoporotic Fractures: Implement preventive strategies, including lifestyle modifications, medication adjustments, and regular follow-ups, to minimize the risk of osteoporotic fractures and promote long-term bone health.
Role of Nutrition in Osteoporosis Management

To optimize osteoporosis management, understanding the pivotal role of nutrition in supporting bone health is essential. Adequate calcium intake is crucial for bone health and osteoporosis prevention, with recommended daily amounts varying by age and gender.
Vitamin D is key for calcium absorption and bone mineralization, deficiency of which is linked to increased fracture risk and impaired bone health. Protein intake is vital for maintaining muscle mass and bone strength, contributing to overall bone health and reducing fracture risk.
Additionally, nutrients like magnesium, potassium, and vitamin K play roles in bone metabolism, impacting osteoporosis risk and management. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall health and positively influences bone density and osteoporosis outcomes.
Ensuring proper calcium intake, vitamin D levels, protein consumption, and overall nutrient balance through a varied and nutritious diet is fundamental for promoting bone health and reducing the risk of osteoporosis.
Exercise Recommendations for Bone Health

We emphasize the importance of weight-bearing exercises to enhance bone density and strength. Incorporating resistance training into exercise routines helps in promoting bone health and reducing the risk of fractures.
Additionally, focusing on balance exercises is crucial for improving stability and preventing falls in individuals at risk for osteoporosis.
Weight-Bearing Exercises Benefits
Engaging in weight-bearing exercises, such as walking, dancing, and stair climbing, is crucial for improving bone density and strength, thereby reducing the risk of fractures in individuals at risk for osteoporosis. Here are four key benefits of incorporating weight-bearing exercises into your routine:
- Stimulates Bone Remodeling: These exercises promote bone growth and remodeling, enhancing bone strength.
- Reduces Fracture Risk: Regular weight-bearing activities help decrease the likelihood of fractures, especially in those with osteoporosis.
- Enhances Balance and Coordination: Weight-bearing exercises can improve balance and coordination, lowering the risk of falls.
- Strengthens Muscles: These activities not only benefit bones but also support muscle strength, contributing to overall bone health.
Resistance Training for Bones
Incorporating resistance training into your exercise routine is essential for improving bone density and strength, playing a vital role in reducing the risk of fractures for individuals at risk for osteoporosis.
Resistance training, such as weightlifting or using resistance bands, helps stimulate bone formation and enhance bone health. These exercises can target specific areas like the spine, hips, and wrists that are prone to bone loss, thus aiding in preventing fractures.
Combining resistance exercises with weight-bearing activities has been shown to positively impact bone mineral density. By integrating resistance training into a comprehensive workout regimen, overall bone health can be improved, potentially lowering the risk of osteoporotic fractures.
Balance Exercises Importance
Balance exercises play a critical role in enhancing stability and reducing the risk of falls in individuals diagnosed with osteoporosis. These exercises help strengthen core muscles, enhance coordination, and improve posture, which are vital for preventing fractures.
Incorporating balance exercises into a routine can increase confidence in movement and daily activities for individuals with osteoporosis. Examples of balance exercises include standing on one leg, heel-to-toe walk, and tai chi, all of which promote better balance and coordination.
Regular practice of balance exercises can help individuals with osteoporosis maintain independence and reduce the likelihood of falls and fractures.
Surgical Interventions for Severe Cases

When addressing severe cases of osteoporosis, surgical interventions such as vertebroplasty or kyphoplasty are considered to stabilize spinal fractures. In severe osteoporosis cases where conservative treatments haven't been effective, procedures like spinal fusion or vertebral augmentation may be recommended to address fractures and enhance stability. These surgical interventions aim to reduce pain, restore vertebral height, and improve the overall quality of life for individuals with severe osteoporosis-related fractures.
Surgical options are typically reserved for cases where there's significant spinal instability or when conservative measures haven't provided adequate relief. Surgeons often opt for minimally invasive techniques when performing surgical interventions for severe osteoporosis. These techniques help minimize risks, reduce recovery time, and promote better outcomes for patients undergoing these procedures. By utilizing these advanced methods, healthcare providers strive to offer effective solutions for individuals facing severe osteoporosis-related challenges, ultimately aiming to improve their overall well-being and quality of life.
Monitoring and Follow-Up Protocols

Regular monitoring and follow-up protocols play a crucial role in evaluating the effectiveness of osteoporosis treatment strategies over time, ensuring adjustments are made based on changes in fracture risk and individual patient needs.
To achieve this effectively, we recommend the following protocols:
- Follow-up Bone Density Testing: Adults on chronic glucocorticoid therapy should undergo bone density testing every 1 to 2 years to track changes in bone mineral density.
- Comprehensive Monitoring: Regular assessments should include a review of clinical history, FRAX scores, bone mineral density measurements, and relevant imaging studies to provide a holistic view of the patient's bone health.
- Utilization of FRAX Scores: Specific thresholds for FRAX scores, bone mineral density values, and hip fracture risk percentages should guide the ongoing assessment of fracture risk to tailor treatment plans accordingly.
- Regular Reassessment: Scheduled reassessments are essential to evaluate the efficacy of osteoporosis treatment strategies, facilitating timely adjustments based on evolving fracture risk and individual patient requirements.
Frequently Asked Questions
What Is the Best and Safest Treatment for Osteoporosis 2022?
We believe the best and safest treatment for osteoporosis in 2022 includes various options like bisphosphonates, anabolic therapy, denosumab, teriparatide, abaloparatide, romosozumab, nasal spray calcitonin, and calcium with vitamin D. These treatments are recommended for postmenopausal women at high risk of fractures.
Regular monitoring of bone mineral density is crucial for those on pharmacological therapies. It's essential to consult healthcare providers to determine the most suitable treatment based on individual needs.
What Is the New Treatment for Osteoporosis in 2023?
In 2023, new treatment options for osteoporosis include bisphosphonates, denosumab, teriparatide, abaloparatide, and romosozumab as recommended therapies. Additionally, nasal spray calcitonin and calcium with vitamin D are added as extra treatment recommendations since 2020.
Anabolic therapy is considered for postmenopausal women with high fracture risk, especially those at very high risk. Regular monitoring of bone mineral density is crucial for high-risk individuals undergoing pharmacological treatments for osteoporosis.
Tailored treatment approaches based on patient factors, fracture risk levels, and shared decision-making principles are emphasized.
What Are the New Guidelines for Osteoporosis Treatment?
We recommend initial fracture risk assessment for adults starting glucocorticoid therapy, with reassessment every 1 to 2 years for those on chronic therapy. Consider clinical history, FRAX scores, BMD, and imaging.
Pharmacologic treatment is strongly advised for medium to very high risk, with oral bisphosphonates preferred for high and very high risk adults. Anabolic agents are conditionally recommended for high and very high fracture risk scenarios, reflecting tailored approaches for individual patient factors.
What Is the Number One Treatment for Osteoporosis?
The number one treatment for osteoporosis is bisphosphonates, commonly recommended for high-risk postmenopausal women. Anabolic therapy is reserved for those at very high fracture risk. Pharmacological interventions are crucial for medium to very high-risk individuals.
Regular risk reassessment is advised after 3-5 years of bisphosphonate use, with potential holidays for low-to-moderate risk patients. It's essential to tailor treatment to individual fracture risk levels for optimal outcomes.
Conclusion
As we wrap up our exploration of the 2022 Osteoporosis Treatment Guidelines, one thing is clear – prevention is key. By following the recommended screening, exercise, and treatment strategies outlined in the guidelines, we can significantly reduce the risk of fractures and improve bone health.
But, there's one more crucial piece of information that we haven't shared yet…
Stay tuned for our next article to uncover the latest breakthrough in osteoporosis research that promises to revolutionize treatment options.