Let’s delve into the disparities between osteoporosis and osteomalacia. While both conditions affect the bones, they differ in terms of their underlying causes and symptoms.
Understanding these distinctions could be vital in navigating the complexities of bone health management. By exploring the nuances between osteoporosis and osteomalacia, we can shed light on how these conditions impact individuals differently, paving the way for tailored treatment and preventive strategies.
It's time to unravel the intricacies of bone diseases and delve deeper into their implications for overall well-being.
Key Takeaways
- Osteoporosis: Decreased bone density, aging factor, proactive screening, bone density scans
- Osteomalacia: Severe vitamin D deficiency, bone and hip pain, muscle weakness
- Diagnosis methods: DEXA scan for osteoporosis, blood tests for osteomalacia
- Treatment options: Bisphosphonates, vitamin D supplements, lifestyle changes, hormone therapy
Symptoms of Osteoporosis and Osteomalacia
When comparing the symptoms of osteoporosis and osteomalacia, it's essential to recognize distinct patterns of presentation in these bone disorders.
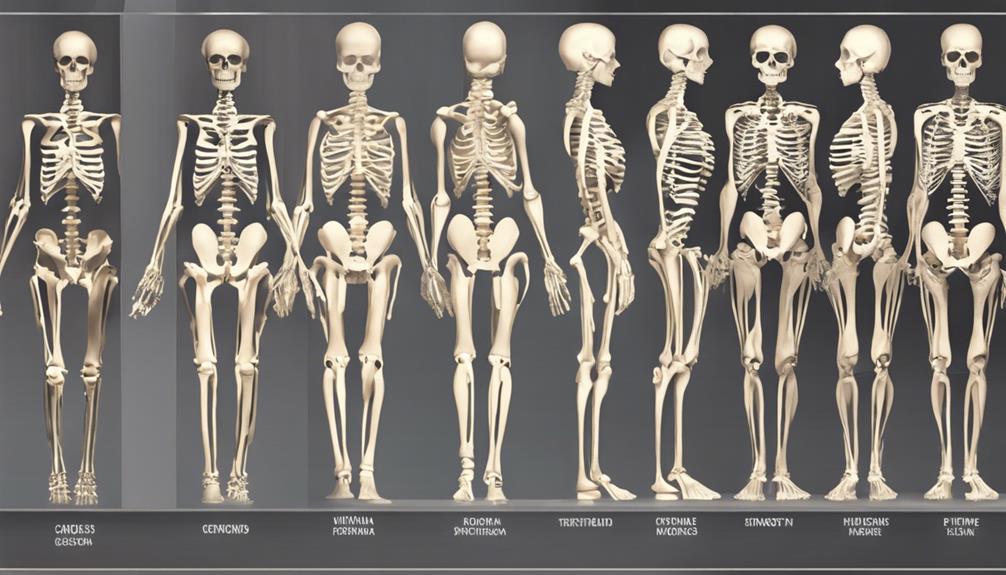
Osteoporosis, often termed a 'silent disease,' may manifest as loss of height, posture changes, shortness of breath, and lower back pain. In contrast, common symptoms of osteomalacia include bone and hip pain, muscle weakness, and difficulty walking.
Osteoporosis can lead to severe complications such as hunched posture, intense back pain, and fractures resulting from minor falls. On the other hand, osteomalacia presents with bone pain, muscle weakness, walking difficulties, and bone deformities.
Understanding these symptoms is crucial for early detection and intervention in these conditions. Risk factors such as age, gender, diet deficiencies, and hormonal imbalances play significant roles in predisposing individuals to these bone disorders.
Proper assessment and management can help alleviate symptoms and prevent debilitating consequences associated with osteoporosis and osteomalacia.
Causes of Osteoporosis and Osteomalacia

Pivoting from the discussion of symptoms, the causes of osteoporosis and osteomalacia stem from distinct underlying factors impacting bone health. Osteomalacia is primarily caused by severe vitamin D deficiency or issues with calcium and phosphate absorption, leading to inadequate new bone formation. Conversely, osteoporosis results from decreased bone density due to insufficient new bone formation or accelerated old bone reabsorption.
Vitamin D deficiency, often from lack of sunlight exposure or digestive/kidney diseases, is a common cause of osteomalacia. Aging is a significant factor in bone weakening, with bone mass loss accelerating after age 35, contributing to osteoporosis development. Various risk factors such as genetics, ethnicity, sex, inactivity, medical conditions, and certain medications can increase the likelihood of developing osteoporosis.
Understanding these distinct causes is crucial in diagnosing and managing these conditions effectively to promote better bone health.
Diagnosis of Osteoporosis and Osteomalacia
To accurately diagnose osteoporosis and osteomalacia, comprehensive evaluation through specialized tests is essential for assessing bone health and identifying potential fracture risks. For osteoporosis, a bone density test, such as a DEXA scan, is commonly used to measure bone strength and predict fracture risk.
Blood tests are crucial for diagnosing osteomalacia, checking levels of vitamin D, calcium, and phosphorus. X-rays play a vital role in identifying structural bone changes or fractures in osteomalacia, aiding in an accurate diagnosis.
Osteoporosis is often diagnosed after fractures occur due to its asymptomatic nature, underscoring the importance of proactive screening. In complex cases where distinguishing between osteoporosis and osteomalacia is challenging, a bone biopsy may be necessary for a precise diagnosis.
Treatment Options for Osteoporosis and Osteomalacia
Comprehensive treatment options for osteoporosis and osteomalacia encompass a range of pharmaceutical interventions, lifestyle modifications, and targeted supplementation strategies. For osteoporosis, bisphosphonates such as Fosamax, Boniva, and Actonel are commonly prescribed to prevent further bone loss. Hormone therapy may also be used to address low bone density. Lifestyle modifications like regular weight-bearing exercise are crucial for promoting bone growth and strength. Monitoring bone mineral density through bone density scans helps assess the effectiveness of treatment.
In the case of osteomalacia, vitamin D supplements play a vital role in managing the condition and addressing deficiencies. Additionally, addressing underlying causes and providing calcium or phosphate supplements are key components of treatment. Lifestyle changes, such as increasing sun exposure and consuming vitamin D-rich foods, can further support bone health in osteomalacia. Treatment strategies for both osteoporosis and osteomalacia aim to improve bone mass and density, reducing the risk of fractures and complications associated with these conditions.
Prevention Strategies for Osteoporosis and Osteomalacia
Ensuring adequate intake of vitamin D and calcium is foundational in the prevention of osteoporosis and osteomalacia. Vitamin D plays a crucial role in bone health by aiding in calcium absorption and maintaining bone density.
Exposure to sunlight is a natural way for the body to produce vitamin D. Engaging in weight-bearing exercises and strength training can further enhance bone density, reducing the risk of osteoporosis and osteomalacia.
Avoiding habits like smoking and excessive alcohol consumption can also contribute to maintaining strong bones. Early detection through regular screenings and check-ups is essential for identifying any bone health issues promptly and preventing the progression of osteoporosis and osteomalacia.
Frequently Asked Questions
What Are the Differences Between Osteoporosis and Osteomalacia?
When looking at bone health, understanding the contrast between osteoporosis and osteomalacia is crucial. Osteoporosis involves decreased bone density and raised fracture risk, mainly affecting older individuals.
Conversely, osteomalacia results from vitamin D deficiency, leading to bone softening and impacting individuals of any age. Distinguishing these conditions is vital for appropriate management and prevention strategies.
What Is the Difference Between Osteomalacia and Osteoarthritis?
When differentiating between osteomalacia and osteoarthritis, it's crucial to note that osteomalacia primarily affects bone mineralization due to vitamin D deficiency, while osteoarthritis targets joint cartilage, causing pain and stiffness.
Understanding these distinctions is vital for accurate diagnosis and treatment planning. By recognizing these unique characteristics, healthcare providers can offer tailored care to address the specific needs of patients with either condition.
Is Vitamin D Deficiency Osteoporosis or Osteomalacia?
When we consider the impact of vitamin D deficiency, it's important to note that it can contribute to both osteoporosis and osteomalacia.
In the context of bone health, vitamin D deficiency can lead to decreased bone density and increased fracture risk in osteoporosis. In osteomalacia, severe vitamin D deficiency causes bone softening.
What Is the Difference Between Osteogenesis and Osteoporosis?
Osteogenesis is like a master builder crafting sturdy, new structures, while osteoporosis weakens existing foundations, making them fragile. Osteogenesis involves bone formation and growth, creating robust skeletal frameworks.
In contrast, osteoporosis deteriorates bones, reducing density and strength, making them prone to fractures. Understanding these processes is crucial in managing bone health and preventing complications.
Regular exercise and adequate nutrition play vital roles in supporting both osteogenesis and combating osteoporosis.
Conclusion
In conclusion, understanding the differences between osteoporosis and osteomalacia is crucial for effective management and prevention of these bone diseases.
One interesting statistic to note is that osteoporosis affects over 200 million people worldwide, making it a significant public health concern.
By recognizing the symptoms, causes, diagnosis, and treatment options for these conditions, individuals can take proactive steps to maintain bone health and reduce the risk of fractures.
Stay informed and prioritize bone health for a better quality of life.